Transferrin is a blood plasma protein that is produced in the liver. Iron from food accumulates in the epithelial cells of the small intestinal mucosa. Transferrin takes part in the transport of iron from the site of absorption to the bone marrow, liver, and spleen. At the Yusupov Hospital, all conditions have been created for the treatment of patients whose transferrin saturation coefficient is outside the normal range:
- Laboratory technicians determine the coefficient of transferrin saturation with iron using modern techniques;
- For patients who have an increased or decreased percentage of transferrin in the blood, hematologists individually select therapy with modern medications;
- The tactics for managing patients with severe disorders of iron concentration in the blood are developed at a meeting of the Expert Council with the participation of professors, associate professors and doctors of the highest category.
General information about the study
This test in medical practice is most often used for the comprehensive diagnosis of iron deficiency anemia. To establish an accurate diagnosis and choose treatment tactics, a doctor needs to know not only the concentration of transferrin, but also its saturation rate (normally it is about 30%). The transferrin blood test
determines both the protein level and the iron-binding capacity of the blood serum. It indicates how much protein is able to bind to iron. Based on this indicator, the protein saturation coefficient is calculated (in the absence of pathologies, it is 10-50). Protein binds to microelements formed during the breakdown of red blood cells and those that enter the body along with food. Iron is a component of hemoglobin and muscle protein. It is necessary for the normal functioning of the body. The total content of this microelement in the body is 4-5 grams. About 0.1% of all trace element reserves circulate in the bloodstream.
If iron levels are below normal, transferrin concentrations increase. Thanks to this, the protein can contact the trace element, even if its concentration in the blood is very low. Protein levels are also influenced by diet, liver condition, and gastrointestinal function. When liver function is impaired, it loses the ability to produce sufficient amounts of protein, and its levels decrease. Its synthesis will also be below normal if a person consumes insufficient amounts of protein foods and in a number of other cases.
Transferrin
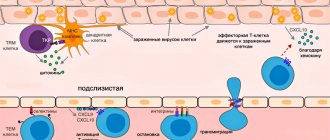
Transferrin transfers iron atoms from the gastrointestinal tract to the cells of iron-depositing organs, between the erythroid elements of the bone marrow and macrophages, and regulates the transport of iron into hepatocytes. Like all transport proteins, transferrin is synthesized in the liver and is also produced in small quantities in lymphoid tissue, mammary gland, testicles and ovaries. It is a glycoprotein with a MW of 76–77 kDa and has significant genetic polymorphism (more than 20 variants of primary structure disorders). Each transferrin molecule is capable of binding two iron atoms; binding requires the presence of bicarbonates.
Iron atoms are transported into the cell through the interaction of the iron-transferrin complex with specific receptors on the plasma membrane. The iron-transferrin complex penetrates into the cytosol, where the iron atom is released, and transferrin leaves the cell into the bloodstream, remaining capable of repeated and multiple binding of iron ions. Reticulocytes have the highest density of transferrin receptors on the plasma membrane. Iron in these cells binds to protoporphyrin to form heme, which when combined with globin forms hemoglobin or myoglobin.
The intensity of transferrin synthesis correlates with total iron reserves according to the feedback principle - when iron reserves are depleted, transferrin synthesis is activated, and when it increases, it decreases. When transferrin saturation is below 16%, the supply of iron to the erythrocyte lineage of the bone marrow becomes insufficient for hemoglobin synthesis, which leads to microcytosis and hypochromia. There is also a decrease in cell proliferation, which entails a decrease in the number of red blood cells. It should be remembered that transferrin is one of the “negative” acute phase proteins, i.e. in various inflammatory diseases, its concentration decreases, which can lead to errors in the diagnosis of iron deficiency.
Indications for the study
- Differential diagnosis of anemia;
- detection of hemochromatosis;
- malignant neoplasms;
- chronic infectious and inflammatory diseases;
- liver diseases;
- kidney diseases;
- pregnancy.
Conditions for collecting and storing the sample.
Sample without signs of hemolysis.
Research method.
To determine the concentration of transferrin in blood serum, immunoturbidimetry or immunonephelometry methods are used.
Increased values
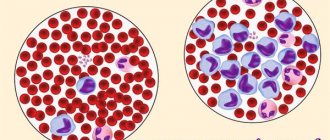
- Iron-deficiency anemia;
- pregnancy (last trimester);
- taking contraceptives, estrogen therapy.
Reduced values
- Hypoplastic, hemolytic, megaloblastic anemia, hemochromatosis, repeated blood transfusions, iron therapy;
- conditions characterized by a decrease in the concentration of iron in the blood serum and inhibition of synthetic processes in hepatocytes (protein starvation, acute and chronic infections, chronic hepatitis and cirrhosis of the liver, surgical interventions, neoplastic processes);
- loss of protein in chronic nephropathy, diseases of the small intestine.
Interpretation of results
The test results are assessed by a doctor; their use for self-diagnosis is unacceptable. When interpreting the results, the fact that the amount of protein is determined by the condition of the liver is taken into account. With iron deficiency, protein levels are increased. When interpreting the results obtained, the gender of the patient must be taken into account. For women, reference values are higher than for men. During pregnancy, indicators can increase significantly in the absence of any pathological changes in the body. The decrease in hepatic protein synthesis with age is due to physiological processes.
Protein deficiency
may be observed in the following cases:
- in the presence of liver cirrhosis;
- with frequent inflammatory and infectious diseases;
- in patients with hemochromatosis;
- with uncontrolled use of hormonal contraceptives;
- in patients with malignant neoplasms.
Excess protein
may indicate anemia.
Reasons for decrease and increase in indicators
In the diagnosis of diseases, a calculated value is used - the percentage of transferrin saturation with iron. Normally this figure is 30%. Anemia may be the cause of a decrease in transferrin iron concentrations. If the iron saturation coefficient of transferrin is increased, low molecular weight iron appears in the plasma. It can deposit in the liver and pancreas, causing damage.
In the third semester of pregnancy, the iron saturation coefficient of transferrin increases by 50 percent. The content of this protein decreases in older people. The percentage of transferrin saturation with iron is reduced in the acute phase of inflammation. Low transferrin and low iron saturation percentage lead to undesirable consequences.
What else is prescribed with this study?
Aspartate aminotransferase (AST)
1.21. Venous blood 1 day
290 RUR Add to cart
Alanine aminotransferase (ALT)
1.20. Venous blood 1 day
290 RUR Add to cart
Alcohol dehydrogenase 1B (class I) ADH1B: ADH1B*2 (Arg48His; Arg47His)
GN0007 Venous blood, DNA extraction 3 days
990 RUR Add to cart
Aldehyde dehydrogenase 2 ALDH2: ALDH2*1/*2 (Glu504Lys; E504K)
GN0017 Venous blood, DNA extraction 3 days
990 RUR Add to cart
Pancreatic amylase
1.23. Venous blood 1 day
440 RUR Add to cart
Urine analysis “Bad habits” (alcohol, nicotine, narcotic and psychoactive substances - more than 800 representatives)
1.91.1 Urine 6 days
RUB 3,500 Add to cart
Complete blood count without leukocyte formula (venous blood)
3.1.1. Venous blood 1 day
330 RUR Add to cart
Blood iron values
Serum iron levels vary significantly throughout the day, reaching a maximum in the morning (difference up to 40%). The indicator values depend on gender and age. Newborns experience a drop in iron levels within a few hours of birth.
Average iron levels in women are lower than in men, but in both men, iron levels in the blood decrease with age. Iron concentration in women is also associated with the menstrual cycle (the highest level is in the luteal phase, the lowest level is after menstruation).
Lack of sleep and stress, severe physical activity also cause a decrease in this indicator. During pregnancy, the iron content in the body decreases, especially in the second half (the increased need for iron during this period is associated with the formation of an iron depot in the fetus).
Normal blood iron levels:
References
- Mental and behavioral disorders caused by alcohol consumption. Alcohol dependence syndrome. Clinical recommendations of the Ministry of Health of the Russian Federation, 2018.
- Myagkova M.A. Determination of markers of chronic alcohol abuse using capillary electrophoresis. // Myagkova M.A., Pushkina V.V., Petrochenko S.N., Morozova V.S. — International Journal of Applied and Fundamental Research. 2015. No. 12-9. pp. 1640-1643.
- Sakran JV, Mehta A, Matar MM, Wilson DA, Kent AJ, Anton RF, Fakhry SM The Utility of Carbohydrate-Deficient Transferrin in Identifying Chronic Alcohol Users in the Injured Patient: Expanding the Toolkit. J Surg Res. 2021 Aug 17;257:92-100. Doi: 10.1016/j.jss.2020.07.027.
Diagnosis of colorectal cancer: determination of transferrin and hemoglobin in stool
Colorectal cancer is a widespread pathology in the world, the incidence is growing every year, and the annual mortality rate exceeds 500 thousand people. A particular problem is the identification of precancerous conditions and intestinal cancer in the early stages. The peak incidence of colorectal cancer occurs after 50 years of age. Men are diagnosed with colon cancer 1.5-2 times less often than women, but rectal cancer is 1.5 times more common.
A new laboratory research method has been introduced in the Centralized Laboratory of the Diagnostic Center, which makes it possible to diagnose gastrointestinal diseases at the world level when examining stool. This method is the determination of transferrin and hemoglobin in feces.
This method is intended for the early detection of intestinal diseases, including precancerous conditions, including intestinal polyps, and intestinal cancer.
How is the quantitative method better than the qualitative occult blood test?
- Taking medications and diet do not affect the results of the analysis; there is no need to limit food and stop medications a few days before donating stool, as is done with the routine “stool occult blood” test.
- The research is performed by a fully automated system.
- The amount of transferrin and hemoglobin is determined, which, with repeated studies, allows the doctor to draw a conclusion about the course of the disease.
- They surpass it many times in sensitivity and specificity (there are no false results).
- Allows you to determine the depth and level of intestinal damage. Diagnostics is improved (including in the early stages) by determining a new indicator - fecal transferrin.
- Fecal transferrin persists for a longer time (up to 5 days).
- After collection in special containers, feces can be stored for a long time (up to 7 days) without reducing the level of transferrin and hemoglobin, which allows the containers to be delivered to the laboratory at a time convenient for the patient.
An increased content of transferrin indicates a predominant damage to the upper intestines, and hemoglobin - to the lower intestines. High values of both indicators allow us to conclude that the process is extensive. The higher the indicator, the greater the depth or affected area.
Indications for examination:
- Suspicion of an intestinal tumor or its presence.
- Monitoring the condition of the intestine after surgery in the presence of a tumor process in the intestine.
- Hereditary nonpolyposis colorectal cancer.
- Familial adenomatous polyposis.
- Polyps and suspicion of their presence.
- Chronic inflammatory diseases of the gastrointestinal tract, colitis.
- After long-term antibacterial therapy and repeated courses.
- Necrotizing enterocolitis.
- Ulcerative processes of the stomach and intestines.
- Crohn's disease and suspicion of it.
- Autoimmune diseases.
- Examination of first- and second-degree family members who have been diagnosed with intestinal cancer or polyposis.
- Screening for colorectal cancer is a preventive examination of people over 40 years of age (once a year is mandatory).
The study does not require preparation.