Anticoagulant therapy is a set of therapeutic measures aimed at inhibiting blood clotting activity and preventing the formation of blood clots. The use of anticoagulants makes it possible to have a targeted effect on different parts of the blood coagulation process. This makes it possible to use them in a number of serious pathological conditions.
CELT phlebologists are well acquainted with the principles of anticoagulant therapy and have been successfully applying them in practice for several years. They carry out an individual selection of appropriate drugs, preventing the development of such dangerous conditions as thrombosis and blockage of blood vessels. Their efforts reduce the risk of heart attacks and strokes.
Classification of drugs and indications
Medicines are divided into groups based on their therapeutic effect and mechanism of influence on the body. There are only 2 types of anticoagulants: direct and indirect.
Direct anticoagulants
The mechanism of action of the drugs is associated with the activity of components that promote the unification of red blood cells, leukocytes and platelets, the rapid restoration of the integrity of affected vessels that are damaged due to the influence of the causative factor.
The main compound affected by direct anticoagulants is thrombin. The components of the drugs stop its activity without changing the volume of content. The structural element of blood is produced in normal quantities and can be detected by laboratory analysis.
Medicines are rapidly metabolized, processed and eliminated from the human body. The therapeutic effect is not long-lasting. Severe adverse reactions, including severe internal bleeding, may occur. For this reason, treatment with direct anticoagulants is carried out under the supervision of a physician. Tablets are prescribed for the treatment of the following diseases:
- Thrombosis
. More often, corresponding changes are diagnosed in the large vessels of the legs, which are characterized by the formation of blood clots that block the lumen. In the initial stages of the disease, you can get by with anticoagulants that restore blood circulation. In the later stages, medications that are classified as thrombolytics are prescribed. - Pulmonary embolism
. The pathology occurs with an increase in pressure in the corresponding structure, which causes disruption of the heart. In this case, anticoagulants are prescribed in complex therapy. - Thrombophlebitis
. The disease is characterized by the formation of blood clots in the vessel and the development of an inflammatory reaction. Drugs from the group of anticoagulants are used in combination with other etiotropic and symptomatic drugs. - Angina pectoris
. Treatment with anticoagulants is effective due to the absence of areas with death of organ tissue. With timely initiation of therapy, a favorable prognosis occurs, which means the risk of complications is minimized. - Acute myocardial infarction
. Tablets are prescribed at any stage of the pathology, including in the post-infarction period to prevent the formation of blood clots. - Autoimmune disorders
related to kidney function (lupus nephritis, etc.), systemic pathologies.
In the treatment of hemorrhoids, the best drugs are in the form of ointments and suppositories, which are easier to use.
The level of lymphocytes in the blood is an important indicator that is used in diagnosing and assessing the condition of the body. A significant change in their concentration indicates serious disturbances in the functioning of various organs and systems, and therefore requires immediate correction. Read more in the article: “how to reduce lymphocytes in the blood.”
Indirect anticoagulants
Advertising:
The difference between direct and indirect anticoagulants is in action. The latter have a complex effect, unlike the other group of drugs. The drugs affect thrombin, but do not suppress activity, but completely destroy it. The mechanism of action of these is also associated with the influence on other coagulation factors, including the rate of aggregation.
Indirect anticoagulants not only help thin the blood, but also restore nutrition to myocardial tissue, relieve spasm from blood vessels, and accelerate the removal of organic salts and excess cholesterol from the body.
Given their complex action, anticoagulants have a large list of possible adverse reactions, especially with long-term use.
Drugs are prescribed for the treatment of the following conditions:
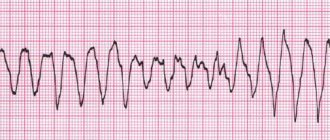
- chronic heart failure, atrial fibrillation;
- severe thrombosis of the deep veins of the lower extremities, if other medications do not help get rid of the pathology;
- recurrent myocardial infarction;
- disruption of the pulmonary artery (in this case, indirect anticoagulants are combined with thrombolytic drugs, despite the risk of developing dangerous complications as a result of complex use).
Indirect anticoagulants are also prescribed for diseases that are treated with drugs from the direct group. The difference is that the former are more often used in chronic pathologies, and the latter in the treatment of acute conditions.
Dexpanthenol is perceived by people as an ointment, but in fact this pharmaceutical product based on vitamin B5 has many forms and also many functions. Read more in the article: “What is dexpanthenol ointment used for?”
Physiology of hemostasis
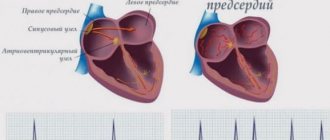
There are cellular and plasma coagulation factors. Cellular factors include platelets, and plasma factors include proteins and enzymes involved in the process of blood coagulation. Plasma coagulation factors are synthesized in the liver and circulate in the blood in an inactive form.
Stopping bleeding occurs in 3 stages and involves both blood vessels and platelets, and plasma coagulation factors:
- Temporary (primary) vasospasm (VascularPhase).
- Formation of an unstable, loose platelet plug due to platelet adhesion and aggregation (PlateletPhase).
- Retraction (contraction and compaction) of the platelet plug due to fibrin threads (CoagulationPhase).
Effective drugs
Advertising:
Direct anticoagulants exist in the form of tablets, ointments, gels, and solutions for subcutaneous or intravenous administration. The components of the drugs are quickly absorbed into the bloodstream, the therapeutic effect lasts throughout the day. The list of direct-acting anticoagulant drugs and the features of administration can be placed in the table:
| Name | Release form | Dosage and frequency of administration | approximate price |
| Heparin ointment | Ointment | 0.5-1 g topically twice a day | From 65 rub. |
| Lyoton | Gel | 3-10 cm of gel topically three times a day | From 350 rub. |
| Venitan | Gel | Apply a thin layer, without rubbing, topically, three times a day | From 260 rub. |
| Fraxiparine | Solution | Subcutaneously or intravenously, taking into account body weight | From 2100 rub. |
| Clexane | Solution | Subcutaneously at a dose prescribed by your doctor | From 570 rub. |
The names of effective indirect anticoagulants are in the table:
| Group | Name | Release form | Dosage and frequency of administration | approximate price |
| Monocoumarins | Warfarin | Pills | Initial dose: 10 mg per day | From 80 rub. |
| Markumar | Pills | Initial dose - 4-6 tablets with a gradual decrease in daily volume | From 3500 rub. per pack of 100 pcs. | |
| Sinkumar | Pills | Initial dose - 4-8 tablets with a gradual decrease in daily volume | From 580 rub. | |
| Dicumarins | Tranexam | Pills | The doctor calculates the dose based on the indication | From 250 rub. |
| Indandions | Omefin | Pills | Initial dosage - 0.05 g per day | No data available |
| Fenilin | Pills | Initial dosage - 0.12-0.2 g in 3-4 doses | From 150 rub. |
There is another group of anticoagulants - a new generation, which include Apixaban, Rivaroxaban, Dabigatran. Medicines are under development. Advantages - rapid therapeutic effect, fewer side effects, no risk of internal bleeding. These are often prescribed to prevent stroke in people with atrial fibrillation.
Clopidogrel (Plavix)
Platelet aggregation is a process that consumes energy. Platelets receive this energy from a special cell energy carrier, adenosine diphosphate (ADP). To do this, adenosine diphosphate needs to attach to a special binding site (receptor).
Clopidogrel irreversibly changes platelet ADP receptors, and therefore platelets remain nonfunctional throughout life, and restoration of normal function occurs as platelets are renewed (after approximately 7 days).
ADP receptor blockers are used if ASA is intolerant or if Aspirin does not work sufficiently. Compared with ASA, patients taking clopidogrel are more prone to bleeding and bruising.
Contraindications for taking medications
Advertising:
Despite the effectiveness of direct and indirect anticoagulants, the drugs are contraindicated in certain cases:
- in the presence of ulcerative tumors in the organs of the digestive system, which creates a risk of internal bleeding;
- for severe kidney pathologies, including failure of the paired organ;
- for severe liver diseases, for example, chronic hepatitis, and others that occur with impaired bile secretion;
- with vitamin deficiency associated with vitamin K or ascorbic acid;
- for blood diseases;
- with septic endocarditis;
- in the presence of blood impurities in the cerebrospinal fluid, as shown by the results of laboratory tests;
- women during pregnancy.
In the latter case, the restriction is due to an increased risk of internal bleeding, as well as the development of intrauterine anomalies in the fetus. Therefore, if possible, it is recommended to stop taking medications already at the stage of pregnancy planning.
It is prohibited to take anticoagulants after a cerebral injury, especially the brain. Otherwise, a negative phenomenon occurs in the form of inhibition of consciousness.
Related medical procedures
Before any medical procedure, be sure to inform your doctor that you are taking anticoagulants and strictly follow his recommendations. On the eve of the procedure, monitoring the level of blood clotting is mandatory. For some dental procedures (filling, canal cleaning, removal of tartar, installation of crowns and bridges), if clotting is within the individual corridor, a change in the therapy regimen is not required. Before tooth extraction, a slight reduction in the dose of the drug taken may be required.
It must also be remembered that patients with a prosthetic heart valve require infection prevention
(bacterial endocarditis).
For this purpose, antibiotics are recommended before and after invasive intervention. This is necessary before visiting the dentist, any urological procedure, gynecological intervention, colon examination, tonsillectomy or implantation of any medical device. Back to section
Possible adverse reactions
The risk of developing negative symptoms after taking anticoagulants is increased if the following factors are present:
- with the development of diseases that are contraindications to taking medications (renal failure, etc.);
- when taken simultaneously with other drugs with which anticoagulants are incompatible;
- when treating patients over 65 years of age;
- with a history of stroke and gastrointestinal bleeding.
Advertising:
The most common side symptom is internal bleeding. Other negative manifestations include:
- skin symptoms characteristic of an allergic reaction of the body: rash, itching, burning, areas with hyperemia, etc.;
- necrotic changes in the epidermis caused by thrombosis of veins and capillaries localized in the subcutaneous fat layer;
- symptoms of general intoxication: headache, weakness, febrile syndrome;
- clinical manifestations from the digestive system: nausea and vomiting, pain in the epigastric region, the formation of ulcerative tumors in the oral cavity;
- dysfunction of the liver and kidneys;
- Among the long-term side symptoms (occurring after 1-2 weeks of anticoagulant therapy) are cholesterol microembolism, leukopenia, and agranulocytosis.
To prevent the development of negative reactions, before starting to take anticoagulants, you need to visit a doctor who will prescribe the correct dosage and determine the maximum possible duration of treatment.
Our doctors
Malakhov Yuri Stanislavovich
Doctor - cardiovascular surgeon, phlebologist, Honored Doctor of the Russian Federation, Doctor of Medical Sciences, doctor of the highest category
Experience 36 years
Make an appointment
Drozdov Sergey Alexandrovich
Cardiovascular surgeon, phlebologist, Doctor of Medical Sciences
47 years of experience
Make an appointment
Disadvantages of anticoagulants and interactions
One of the significant disadvantages of therapy with direct and indirect anticoagulants is the possibility of internal bleeding. In addition to hemorrhage in internal organs, for example, in the digestive tract, this can also occur in the subcutaneous layer.
Another disadvantage of drugs from the group of anticoagulants is their high price. Relatively cheap products containing warfarin.
Despite the affordable pricing policy for warfarin products, regular monitoring of laboratory parameters is necessary during treatment.
Among the disadvantages is the frequent occurrence of specific adverse reactions. For example, drugs containing heparin cause thrombocytopenia, and drugs based on warfarin cause necrosis of skin tissue and other epidermal pathologies.
The disadvantage of anticoagulant therapy is the impossibility of combining it with certain medications due to the development of specific reactions. Reduced therapeutic effect when taken in combination:
Advertising:
- with barbiturates, carbamazepine, griseofulvin, glutethimide;
- estrogen preparations, hormonal contraceptives;
- aluminum hydrochloride, cholestyramine, colestipol;
- alcoholic drinks (for chronic alcoholism).
Increased risk of internal and epidermal bleeding with combined use:
- with acetylsalicylic acid, ticlopidine, non-steroidal anti-inflammatory drugs, cephalosporins, penicillins, phenylbutazone, sulfinpyrazone;
- antimetabolites, quinidine, quinine, salicylates;
- glucocorticoids.
Increasing the therapeutic effect when taken in combination:
- with oral antibiotics, sulfonamides;
- with acetaminophen, chloral hydrate, ethacrynic acid, miconazole;
- with omeprazole, co-trimoxazole, ethanol, metronidazole, ofloxacin, statins;
- with anabolic steroids, influenza vaccine, tetracyclines, thyroid hormones, vitamin E.
If it is impossible to exclude the complex use of incompatible drugs, constant monitoring of the patient’s condition is important (checking the rate of blood clotting, identifying sediment in the urine, determining the level of prothrombin, etc.).
Patient taking antiplatelet drugs
Monotherapy
Recent studies have shown that basic surgical skills and local bleeding control measures are sufficient to control bleeding. Antiplatelet monotherapy does not pose a significant risk during or after surgery.
Recommendations [6]: it is strictly not recommended to interrupt the intake of oral antiplatelet agents during outpatient dental procedures, including surgical procedures.
Dual antiplatelet therapy after stent implantation in patients with stable coronary artery disease or acute coronary syndrome (ACS)
Cardiologists recommend dual antiplatelet therapy for at least six weeks after bare metal (inactive) stent implantation, and for 12 months after an episode of ACS or drug-eluting stent (active stent) implantation.
Recommendations [7]: Low-risk dentoalveolar surgery does not require any changes in the treatment plan.
Dentoalveolar surgery with an average risk of bleeding requires consultation with a cardiologist about temporarily stopping one of the drugs before the surgical procedure (monotherapy does not pose a serious risk). If it is not possible to cancel one of the drugs, you can perform the surgical procedure in stages: divide the surgical procedure with an average risk of bleeding into several smaller interventions.
Dentoalveolar surgical procedures with a high risk of bleeding require consultation with a cardiologist regarding temporary discontinuation of one of the medications before the surgical procedure. If it is not possible to discontinue one of the drugs, major surgical operations should be delayed for 1 year.
Overdose and treatment
Relevant studies and observations have proven that one hundred times taking a warfarin-based drug in an increased dosage does not cause serious negative reactions. An overdose of anticoagulants with another active substance or multiple excesses of the recommended dose of warfarin is accompanied by the following symptoms:
- the appearance of subcutaneous hemorrhages (bruises);
- the presence of blood in urine and feces;
- an increase in the volume of menstrual blood secreted in women;
- the formation of extensive hematomas in the cervical region, which contributes to compression of the respiratory tract;
- intracranial hemorrhage.
Before the active components are absorbed into the blood, you need to induce vomiting by drinking a large amount of liquid and pressing on the root of the tongue. To remove drug residues from the intestines, the victim is given any sorbent, for example, activated carbon.
First aid is recommended to be carried out in the first 2 hours after taking an increased dosage of the drug, since later measures will be ineffective.
Further rehabilitation measures are carried out in a hospital setting. In case of hemodynamic disturbances or hypoxemia, a blood transfusion is performed.
Anticoagulants are prescribed in the treatment of many diseases that occur with an increase in blood viscosity. To achieve the maximum therapeutic effect, before taking the drug, you need to exclude contraindications and determine the daily dose, taking into account the primary pathology.
Secondary hemostasis (coagulation)
The formed platelet plug (without subsequent formation of fibrin) can only temporarily stop bleeding, and if the platelet thrombus does not thicken with insoluble fibrin, then such a thrombus will disintegrate after a few hours. Simultaneously with platelet activation, plasma coagulation factors are activated (secondary hemostasis). Goal: stabilization of the primary platelet plug due to the formation of fibrin networks and the formation of a dense and stable fibrin clot.
Clinical significance:
- if disturbances are present at the stages of primary hemostasis (vascular-platelet), for example, thrombocytopenia (< 50,000 cells/mm3) or taking antiplatelet drugs (Aspirin, Plavix), then prolonged and continuous bleeding should be expected during and immediately after surgery (due to disturbances in the formation of the primary platelet plug);
- if disturbances are present at the stages of secondary hemostasis (coagulation), and primary hemostasis is not impaired (for example, taking anticoagulants), bleeding problems will be detected only a few hours, or even the next day, after surgery (when the patient is no longer in the clinic) .