Life after surgery
Recommendations for patients after radiofrequency catheter ablation of atrial fibrillation (AF):
- Observation by a cardiologist (therapist) at the place of residence;
- Limiting physical activity for 2 weeks;
- Control of daily monitoring of ECG (CMECG), echocardiography after 3 months at the place of residence;
- Taking Warfarin or new oral anticoagulants (Pradaxa, Xarelto, Eliquis) for at least 3 months, possibly up to 6-12 months, with a permanent form of AF - lifelong use;
- Taking antiarrhythmic drugs (AAP) for at least three months;
- If paroxysmal AF occurs, call an ambulance 03, take an ECG;
- After surgical treatment of AF, the effectiveness of the operation is not assessed for three months. At this time, sensations of interruptions in the work of the heart, discomfort, and possible rhythm disturbances may persist. In 10-15% of patients, AF paroxysms persist after three months; a repeat consultation with an arrhythmologist may be required to decide whether a repeat procedure is necessary.
About cryoablation surgery
Cryoablation is one of the most effective, safe and simple ways to treat heart rhythm disorders.
It is used to isolate the mouth of the pulmonary veins (the source of pathological pulsation that leads to atrial fibrillation) and stop the transmission and spread of unwanted electrical impulses throughout the atria. It is performed without incisions using local anesthesia, through controlled destruction of arrhythmogenic areas using freezing. In the cardiology center of the Federal Scientific Research Center FMBA, a fairly young, but successful type of operation has been carried out since 2021. Holter monitoring is carried out in two ways:
- Spot – replaces radio frequency; instead of high-frequency current, liquid nitrogen is supplied and spot freezes the damaged areas;
- Balloon - a catheter with a balloon at the end is inserted into the femoral artery, reaching the pulmonary veins, the balloon is inflated, completely filling the place where the vein flows into the atrium, and cauterizes the pathological area with cold.
Key benefits of cryotherapy
efficiency - during the operation, the pathological focus that provokes rapid heartbeat is completely blocked, the heart rhythm is restored
duration – the operation takes 1-1.5 hours
safety - due to the speed of the procedure, the time of radiation exposure to the patient is reduced, and the likelihood of blood clots is reduced. The risk of postoperative complications is minimal
simplicity of execution - the operation does not require dissection of the chest, it is performed using a single puncture of the femoral artery
Briefly about the main thing
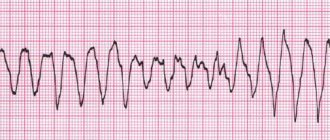
Cardiac arrhythmia is a disturbance in the rhythm of the heart chambers or conduction. The main mechanism of development is the pathology of the conduction system of the heart, which is caused either by organic or functional disorders of myocardial contractions, or by extracardiac causes (thyrotoxicosis, diseases of the nervous system, etc.). Pathology of heart rate (HR) increases the load on the myocardium and reduces the supply of oxygen to organs. Some arrhythmias threaten the development of cardiac arrest, the occurrence of heart attacks and strokes, and thromboembolic complications.
Indications for balloon cryoablation
The indication for the operation is atrial fibrillation.
Like any minimally invasive operation, cryoablation has contraindications:
- life-threatening condition of the patient;
- the presence of blood clots in the atrium;
- thrombosis of the left atrial appendage;
- acute myocardial infarction;
- acute stroke;
- infectious diseases;
- inflammatory processes in the body;
- diseases of the kidneys, liver, respiratory organs;
- an allergic reaction to the contrast used during surgery.
Why is heart cauterization surgery performed for arrhythmia and tachycardia?
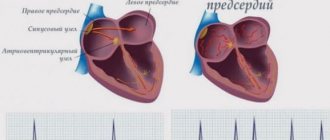
Cauterization of the heart during atrial fibrillation
In a healthy person, the muscles always contract at the same time, but this does not happen in a patient with atrial fibrillation. A circulation of impulses is created and a focus of excitation is formed. Why is heart cauterization surgery performed for arrhythmia and tachycardia?
- Surgery is considered necessary in most cases for atrial fibrillation.
- First, during diagnosis, the patient is diagnosed in the hospital and prescribed medication.
- If after drug treatment the dynamics do not become positive, then the person needs ablation.
- Such cauterization is necessary for people suffering from gastric tachycardia. This is the most dangerous disease because a person's heart rate accelerates and fibrillation may develop over time. This leads to the fact that the myocardium completely ceases to function.
Indications for cauterization of the heart may vary, but all examinations and prescriptions should be carried out only by a qualified cardiologist.
Preparing for surgery
To determine whether there are contraindications to the operation and to ensure a successful outcome of ablation, the patient must undergo a series of studies. They can be divided into two parts:
- clinical and laboratory tests:
- clinical blood test;
biochemical blood test: total protein, creatinine, urea, total bilirubin, direct bilirubin, glucose, pancreatic amylase;
- general urine analysis;
- expanded coagulogram;
- ADP platelet aggregation;
- determination of blood group and Rh factor;
- markers of infections: HIV, hepatitis B, hepatitis C, syphilis;
- Pro-BNP, CRP, troponin.
- Instrumental studies:
- chest x-ray;
ECG;
- EchoCG;
- EGDS;
- Ultrasound scanning of brachiocephalic arteries;
- Ultrasound scanning of the arteries of the lower extremities;
- Ultrasound scanning of the veins of the lower extremities;
- FVD;
- Ultrasound of internal organs;
- TEE;
- coronary angiography;
Depending on the presence of concomitant diseases, additional studies, tests and consultation with specialized specialists (neurologist, endocrinologist, ophthalmologist, etc.) may be prescribed.
After the studies, the patient needs to prepare for surgery:
- a few days before cryoblation, the doctor stops taking medications;
- on the day before surgery, breakfast, lunch and light dinner are allowed;
- 12 hours before the test you cannot eat anything, you must stop taking liquids 8 hours before;
- at night the patient is given a cleansing enema;
- in the morning on the day of surgery, the patient takes a shower and performs hygiene procedures (it is necessary to shave the hair at the site of the catheter insertion - usually in the groin area);
- Before the operation, the patient is examined by a surgeon and an anesthesiologist. A mild sedative is administered to help relax and calm anxiety.
The Cardiology Center of the Federal Scientific and Clinical Center of the Federal Medical and Biological Agency offers patients planned hospitalization to conduct all necessary studies and prepare for ablation. Our multidisciplinary center is equipped with its own laboratory and modern equipment. Therefore, you can take tests and undergo all studies in our clinic. We guarantee the accuracy of the results and the speed of their delivery.
Diagnostics
To shorten the diagnostic search, tell your doctor about diseases that contribute to the development of pathology: • heart disease; • myocardiopathy; • atherosclerosis; • arterial hypertension; • diabetes; • thyroid disease; • kidney diseases. If you are taking medications, tell your doctor. To your appointment, you must bring with you all available medical documents, the latest ECG data, cardiac ultrasound, and laboratory tests. The main method of establishing a diagnosis for disturbances in the rhythm of myocardial contractions is electrocardiography and its modifications: provocative tests, Holter monitoring (ECG recording for hours, days or even several days).
Carrying out cryoablation
Cryoablation to isolate the pulmonary veins is performed in the radiology department.
During the operation the following manipulations are performed:
- the arrhythmologist surgeon makes a puncture in the groin area, inserts a diagnostic catheter through the femoral artery and leads it to the heart;
- reaching the right atrium, the doctor makes a puncture (puncture) of the interatrial septum. This allows access to the left atrium;
- a contrast agent is injected, using a diagnostic catheter, the doctor will determine the pathological focus and see the necessary place for ablation on the screen of the X-ray machine;
- after the diagnostic catheter, a cryoballoon is inserted, reaching the left atrium, the balloon is inflated;
- the doctor brings the balloon to the mouth of the pulmonary vein and closes the passage, thereby stopping the blood flow between the atrium and the vein;
- once closure is confirmed, the physician injects a refrigerant into the cryaballoon;
- The criaballoon, evaporating, takes heat from the damaged heart tissue. At this point, the tissue becomes scarred and can no longer generate and distribute electrical impulses that were the cause of heart rhythm disturbances;
- the balloon is deflated and the catheters are removed. A tight antiseptic bandage is applied to the puncture site;
- The patient is transported from the operating room to the intensive care unit.
Cryoablation is a modern method of treating arrhythmias, which appeared in medical practice quite recently, but has already proven itself to be effective and safe. Our arrhythmologist surgeons perform this operation every day and see how effective and safe it is. If you have concerns or doubts, you can always call us and consult with a specialist.
Radiofrequency catheter ablation (RFA) of the heart.
Radiofrequency catheter ablation (RFA) of the heart.
RFA of the heart is a surgical catheter intervention using special catheters inserted into the heart cavity through vessels and radiofrequency energy, aimed at eliminating heart rhythm disturbances (arrhythmias).
Radiofrequency ablation is one of the most modern methods of treating certain types of heart rhythm disorders. This type of treatment is a minimally invasive procedure, since it does not require any incisions or access to the heart, but sometimes RFA is performed during open-heart surgery. Radiofrequency ablation is performed using a thin, flexible guide catheter that is inserted through a blood vessel and directed to the source of the abnormal rhythm in the heart that is causing the arrhythmia. Next, a radiofrequency pulse is sent through this conductor, which destroys the area of tissue responsible for the abnormal rhythm. For the first time, high-frequency energy to eliminate additional AV pathways, which is still used today, was produced in 1986 by M. Borggrefe et al. Since that time, the rapid development of interventional arrhythmology in the treatment of cardiac arrhythmias began.
Such destruction of a pathological focus can also be carried out through other physical influences, according to which other types of ablation are distinguished:
- Laser ablation.
- Ultrasound ablation.
- Cryodestruction, i.e. ablation using low temperatures.
Indications for RF ablation are heart rhythm disturbances that cannot be corrected with medication:
- Atrial fibrillation .
- Ventricular and supraventricular tachycardia .
- Wolf-Parkinson-White syndrome, or WPW syndrome.
- Paroxysmal tachycardia.
Along with the indications for RFA, ablation also has a list of contraindications:
- Poor general health of the patient.
- Acute infectious diseases.
- Severe diseases of the respiratory system and (or) kidneys.
- Endocarditis is inflammation of the inner lining of the heart.
- Unstable angina for 4 weeks.
- Acute myocardial infarction.
- Heart failure in a patient in the stage of decompensation.
- Severe arterial hypertension .
- Left ventricular aneurysm with thrombus.
- The presence of blood clots in the cavities of the heart.
- Hypokalemia and other manifestations of electrolyte imbalance in the blood.
- Anemia , i.e. pathology of the cellular composition of the blood.
- Allergic reaction caused by X-ray contrast agent.
- Iodone intolerance
- Stenosis of the trunk of the left coronary artery more than 75%, high degree of valvular or subvalvular stenosis of the aortic valve (if it is necessary to enter the LV cavity)
- Thrombophlebitis
- Bilateral limb amputation
Radiofrequency (RF) energy has a wide range and depends on the resistance and dielectric properties of tissue. RF current is a current with changing polarity at a frequency of 30 kHz to 300 MHz. All RF current generators used for ablation operate in the 300 kHz - 1 MHz range. For ablation of cardiac structures, unmodulated current is used, since it is this that leads to the formation of coagulative necrosis.
There are two options for supplying electrical energy: monopolar and bipolar. In monopolar ablation, an alternating current is passed from the distal end of an “active” electrode through the tissue to a “passive” electrode on the surface of the chest wall. Typically the “passive” or reference electrode is a plate. Experiments have shown that the position of the plate has little effect on the size of the impact, while increasing its area leads to impedance deviation and leads to increased energy and overheating of the electrode. In the case of bipolar coagulation, the current passes between two active electrodes in the cavities of the heart.
The leading mechanism of tissue coagulation under the influence of radiofrequency current is the conversion of electrical energy into thermal energy. If the current density is high and the electrical conductivity is low, then this leads to the excitation of ions, which begin to follow changes in the direction of the alternating current. Both of these factors take place in the tissue surrounding the “active” electrode. This excitation of the ions leads to the generation of frictional heat so that the tissue adjacent to the electrode, and not the electrode itself, is the main source of heat. An increase in temperature in myocardial tissue leads to some electrophysiological effects. Using isolated papillary muscles of pig hearts, it was noted that at a tissue temperature of 38-45°C for 1 minute, the function of K-Na channels of cells increases up to a critical level. Heating to 45-50°C leads to inactivation of these structures. Abnormal cell automatism was noted when the temperature increased above 45°C, and increased excitability above 50°C. Biological cell death depends on two factors - exposure time and temperature. Reversible cellular changes occur with prolonged heating even at temperatures below 45°C, while irreversible cell death probably occurs between 52°C and 55°C. Denaturation of the inner layer of cell membrane proteins, which plays a critical role in transport metabolic processes, is the most important mechanism of terminal cell death. At temperatures above 100°C, evaporation of cell fluid occurs and damage to the cell membrane of the myocyte, sarcoplasmic reticulum and mitochondria. If the temperature exceeds 140°C, carbonization of the fabric may occur. In this regard, in order to ensure softer tissue coagulation, tissue temperature should be maintained below 100°C. The temperature of the tissue in contact with the electrode can be monitored with a special ablation catheter with thermistors or thermocouples built into the end of the catheter. Direct heating of the electrode by electric current does not occur due to its good electrical conductivity.
Progressive exposure is achieved through the development of high-frequency energy temperature control devices (Haverkampf et al. 1991). Temperature control means that the temperature at the tip of the catheter not only changes during the coagulation process, but is also maintained at a certain level thanks to a feedback mechanism for the power supplied. Such a device allows the creation of a limited lesion with a predictable extent in vitro and ensures good contact between the ablation electrode and the myocardium. Temperature monitoring becomes practically difficult as the electrode size or geometry increases. For example, for linear ablation of AF and AFL, elongated electrodes with one thermocouple are used, so it is impossible to predict which side of the electrode surface is in contact with the endocardium, and the temperature of the edge surface may be much higher than the body of the electrode where the temperature sensor is located. Thus, the temperature at the midpoint remains underestimated.
Some experimental studies have demonstrated three-dimensional definitive elementary analysis of the influence of electrode geometry, electrode-tissue contact angle, and surrounding blood circulation on ablation lesion size.
The duration of radiofrequency ablation is also an important criterion affecting the transmurality of the effect. The greatest increase in lesion size occurs during the first 30 seconds of ablation and then plateaus. Some improvements in ablation have been achieved by using an electrode with tip cooling by saline infusion. This design allows the use of high impact energy numbers, increasing the size of the damage, but avoiding high impedance numbers. This concept has been confirmed in in vivo and in vitro experiments. Cooling during ablation results in an increase in temperature deeper than the endocardial surface. The maximum temperature is recorded at a depth of 1 mm or more from the endocardial surface, thus even higher than in the area of contact of the electrode with the endocardial surface. Catheters for cold ablation can be of a closed type, when a cooling solution circulates inside the system, and an open type, with small holes through which the electrode is irrigated and the liquid flows out.
Thus, radiofrequency ablation is a safe and effective technique. During experimental studies, no serious complications such as arrhythmias, hemodynamic disorders, ischemia, thrombosis or embolism were observed. The greatest danger is overheating and subsequent damage to the ablation catheter and vaporization of tissue. In order to limit the risk of these complications, many researchers believe it is necessary to measure biophysical parameters (current strength, voltage, temperature) at the end of the catheter.
Possible complications of cardiac RFA are divided into 4 groups:
1. Complications caused by radiation exposure (approximately 1 millisievert) - 2. Complications associated with puncture and catheterization of blood vessels (arterial damage, thrombophlebitis, arteriovenous fistula, pneumothorax); 3. Complications during catheter manipulations (damage to heart valves, embolism - systemic or in the pulmonary artery, perforation of the coronary sinus or myocardial wall, cardiac perforation, tamponade, infection - systemic or at the puncture site);
4. Complications caused by radiofrequency exposure (AV block)
5. Accidental disruption of the integrity of cardiac muscle tissue at the time of ablation.
6. Malfunctions in the electrical system of the heart, aggravating cardiac arrhythmias and requiring pacemaker transplantation.
7. Stenosis of the pulmonary veins, i.e. narrowing of their lumen.
Complications after RFA of the heart are extremely rare: the probability of negative consequences of ablation does not exceed 1%. Therefore, RFA is classified as a low-risk operation. However, to prevent complications, there are a number of special measures taken at each stage of detection and treatment of tachycardia.
The risk of such complications increases in cases where the patient is diabetic, if he has impaired blood clotting, and also if he has passed the 75-year age threshold.
This operation belongs to the class of minimally invasive interventions. The advantages of such a surgical intervention are obvious: minimal trauma, as a rule, no need for general anesthesia, short duration of the operation, short postoperative bed-day
How to prepare for RFA.
Preparation for this operation consists of conducting an electrophysiological study (EPS) of the heart. The need for RFA in a particular patient is determined by his attending physician based on the history of the disease and data from such diagnostic methods as:
- Electrocardiography (ECG) is a popular method of electrophysiological instrumental diagnostics, based on recording and studying the electric fields that are formed during the work of the heart;
- Long-term recording of an ECG (LMECG) is an electrophysiological diagnosis, the essence of which is the continuous recording of an electrocardiogram for at least 24 hours.
After registering an attack of tachycardia using an ECG, the patient is hospitalized in a hospital to undergo a full course of examination and submit a list of necessary tests, on the basis of which he can be prescribed radiofrequency ablation of the heart:
- Laboratory blood tests (biochemical analysis, hormonal studies, determination of lipid levels, electrolytes, etc.);
- Stress test, echocardiography;
- Ultrasound examination of the heart (ultrasound);
- Magnetic resonance imaging (MRI).
General principles of preparation for surgery include: • Last meal the evening before surgery (12 hours of fasting). • Hair should be shaved at the catheter installation site (groin and subclavian area)
• The night before the study, bowel cleansing is carried out. • Ask your doctor if you should take your regular medications in the morning. • All antiarrhythmic drugs are discontinued 2–3 days before the study (five half-lives), for cordarone this is 28 days. • If you have diabetes, ask your doctor whether you should take insulin or other oral blood glucose-lowering medications before the test.
Methodology for RFA of the heart.
RFA of the heart is performed routinely in a specially equipped operating room equipped with:
• X-ray television system for fluoroscopy and/or radiography; • equipment for monitoring the vital functions of the body and carrying out resuscitation measures (defibrillator, breathing apparatus, monitors);
• specialized EPI equipment for recording surface electrocardiograms and intracardiac electrograms and equipped with • a specialized pacemaker and a set of instruments for cardiac catheterization and catheter electrodes for EPI and RFA;
• protective equipment for the patient and staff (suits, aprons, glasses, mobile walls, etc.).
The patient for RFA surgery enters the operating room on an empty stomach, in a slightly sedated state. The areas of intended vascular puncture are carefully processed and covered with sterile linen. Catheter placement is always done using a percutaneous technique. For puncture, the femoral veins on the right and/or left, the subclavian vein on the left and/or right and the jugular vein on the right, as well as the veins of the forearm are usually used. For arterial access, the right femoral artery is usually used, but puncture of the left femoral artery and radial arteries is possible.
Local anesthesia is applied to the puncture site, after which the vein is punctured using a needle, which is inserted into the vessel, and a guidewire of the required length is inserted, after which the needle is pulled out. Next, an introducer is inserted through the guidewire, and then a catheter electrode is inserted into the corresponding chamber of the heart. After placing the catheters in the various chambers of the heart, they are connected to a junction box that carries electrical signals from the electrodes in the heart to the recording equipment and allows the pacing pulse from the pacemaker to reach the surface of the various chambers of the heart. EPI of the heart is performed. Electrical signals received from the endocardial surface of the heart are filtered, amplified, and displayed on a computer monitor. A programmable pacemaker must have the ability for constant and programmable stimulation, supplying multiple extrastimuli (up to 7), adjusting the amplitude and duration of the impulse, as well as the ability to perceive external and intracardiac signals.
During EPI, the patient may feel discomfort in the chest, palpitations, and slight pain. The sensations that arise during EPI, in the form of heart interruptions, second stops, acceleration or deceleration of the rhythm, are the result of the doctor’s work, i.e., with the help of electrical impulses supplied directly to the heart, the doctor completely controls the heartbeat, provoking an attack of palpitations or stopping it during search for arrhythmogenic areas. When arrhythmogenic zones are detected (additional atrioventricular connections, ectopic activity, etc.), it is exposed to radiofrequency energy using a “therapeutic” electrode. After which, without fail (after about 20 minutes), EPI is performed again to assess the effectiveness of the effect. If the electrophysiological indicators satisfy the doctor, then the operation is completed. Catheters are removed. Hemostatic (pressure) bandages are applied to the puncture sites.
You are transferred to the department and prescribed bed rest in the supine position for several hours (in some cases up to a day) in order to prevent bleeding from the puncture site. Observation in hospital from one to 3 days.
Surgical treatment of atrial fibrillation
Atrial fibrillation (AF) in medical terminology is a heart rhythm disturbance (atrial fibrillation). It can be caused by an increased number of electrical circuits in the atria, which lead to erratic contractions of the heart's ventricles and failure of the atria to contract effectively. This, in turn, causes blood clots to form in the atria, which can ultimately lead to blockage of blood vessels in the brain and death of the patient.
Among the main methods of treatment for atrial fibrillation today are drug therapy, catheterization, as well as the surgical labyrinth technique (Maze) - quite complex and therefore not very popular among cardiac surgeons.
A “new word” in the treatment of atrial fibrillation has become radiofrequency ablation of the heart (RFA) of the ostia of the pulmonary veins - a minimally invasive operation through small punctures, carried out using the latest computer technologies and under constant X-ray monitoring.
After ablation: chaotic impulses that provoke arrhythmia cannot enter the atrium cavity
Rehabilitation after RFA
In general, rehabilitation after RFA lasts several months, during which the patient may be prescribed antiarrhythmic drugs (for example, Propafenone, Propanorm, etc.), including those that the patient took before ablation. Bed rest with monitoring of heart rate and blood pressure is indicated for the patient only on the very first days after surgery, during which a rapid recovery and stabilization of the patient’s normal general well-being occurs. The need for repeated RFA, as practice shows, occurs less frequently in operated patients if the patient reconsiders his usual lifestyle:
- Limit consumption of drinks with alcohol and caffeine;
- Reduce the amount of salt in your diet;
- Will adhere to an appropriate diet;
- Choose the optimal mode of physical activity;
- Quit smoking and give up other bad habits.
Ablation results
Cardiac ablation can be successful, but some patients have to repeat the procedure. You may need to take medications even after ablation.
After operation
After ablation, the patient is under the supervision of our specialists in the postoperative rehabilitation ward. For the first few hours, medical personnel monitor the patient's vital signs, heart rate and pain symptoms. The first day the patient was prescribed bed rest. During this time, the heart will adjust to a new rhythm, and the wound at the site of insertion of the catheter will begin to heal. On the second day, you are allowed to gradually get up and move slowly around the ward. If all indicators are normal, the patient is discharged on the 3rd day. Before discharge, the patient is examined by a doctor, who gives his recommendations and instructions on rehabilitation.
Cryoblation therapy is very effective and can completely relieve the patient of arrhythmia, but the effect of the operation largely depends on the patient himself. During the rehabilitation period (1-3 months), it is necessary to follow all doctor’s instructions and recommendations for recovery:
- avoid heavy physical activity;
- avoid psycho-emotional stress and stress;
- refuse hardening, hot baths, trips to the bathhouse and other activities with possible temperature changes;
- monitor proper nutrition and follow a diet: give preference to boiled dishes rather than fried ones, exclude fatty foods, do not eat fast food, avoid excessive consumption of salt and sugar, add fish, lean meat, fresh vegetables and fruits to the diet;
- give up bad habits (smoking, drinking alcohol, overeating);
- Take medication in consultation with your doctor;
- Visit a cardiologist promptly for a routine examination. An ECG must be done a month after surgery, then after 3 and 6 months.
Treatment of cardiac arrhythmia - cauterization: price, cost of such an operation to restore rhythm
Any patient is concerned about the cost of this or that medical procedure. In Russia, many operations are carried out free of charge and are paid for by the state. When asked whether treatment for cardiac arrhythmia, namely cauterization, is included in the list of free services, only a doctor will answer you.
However, it is worth noting that good specialists who carry out such manipulations are located in the capital and other big cities. Treatment in this case can vary within 300,000 rubles . The price of an operation to restore rhythm in Israel or Germany can reach up to 20,000 euros . The price will include a complete diagnosis before treatment, the manipulation itself and rehabilitation.