The issue of disability worries many patients who suffer from severe forms of arrhythmia. To get the answer, you need to look at the basic rules and regulations followed by medical examinations.
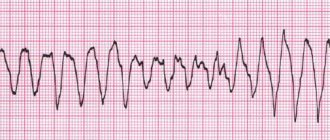
Arrhythmia is a disorder of the heart rhythm (HRR), characterized by a change in the frequency of heart contractions, rhythm, and the basic capabilities of the organ (conductivity, automaticity, excitability). According to the Doshchitsin classification from 1991, there are 10 types of arrhythmias, among which the most severe are considered to be: atrial fibrillation, flutter and ventricular/atrial fibrillation.
Arrhythmia and disability are a pressing issue for many related to health status, performance, and disease prognosis.
To provide the correct answer to the question “Do arrhythmia provide disability?” It is not enough to know the exact diagnosis of the patient, because the assignment of disability is not only a medical field, but more of a medical and social category. Therefore, first of all, you need to know what criteria exist for differentiating patients referred for disability with heart rhythm disturbances.
CLASSIFICATION of cardiac arrhythmias (V.L. Doshchitsin, 1991).
I. Impairment of impulse formation. 1. Sinus tachycardia. 2. Sinus bradycardia. 3. Sinus arrhythmia. 4. Migration of the rhythm source. 5. Extrasystole: a) suprapentricular and ventricular; b) single, group, allorhythmic. 6. Paroxysmal tachycardia: a) supraventricular and ventricular; b) paroxysmal and constantly recurrent. 7. Non-paroxysmal tachycardia and accelerated ectopic rhythms - supraventricular and ventricular. 8. Atrial flutter: a) paroxysmal and persistent; b) regular and irregular shapes. 9. Atrial fibrillation: a) paroxysmal and persistent; b) tachysystolic and bradysystolic forms. 10. Flickering (fibrillation) and ventricular flutter.
II. Conduction disorders. 1. Sinoatrial blockade—complete and incomplete. 2. Intraatrial block - complete and incomplete. 3. Atrioventricular block: a) I, II and III degrees; b) proximal and distal. 4. Intraventricular block: a) mono-, bi- and tri-fascicular, focal, arborptic; b) complete and incomplete.
III. Combined arrhythmias. 1. Sick sinus syndrome. 2. Escaping (slipping) contractions and rhythms - supraventricular and ventricular. 3. Syndromes of premature excitation of the ventricles. 4. Parasystoles. 5. Long QT syndrome.
The main drugs for preventing stroke in AF are anticoagulants
The main drugs for patients with AF that prevent stroke are anticoagulants, the effect of which reduces blood clotting. They prevent the formation of blood clots and therefore reduce the risk of stroke. Coagulation is a normal protective reaction of the body to damage to the vascular wall. With atrial fibrillation, anticoagulants are absolutely necessary for almost everyone.
The most famous anticoagulants in Russia are Eliquis, Xarelto and Pradaxa.
Also, some patients can take Warfarin (with INR monitoring). It is prescribed for low glomerular filtration rate (or creatinine clearance - an indicator of kidney function) or for prosthetic valves.
When taking Warfarin, it is necessary to monitor the INR in the blood (International Normalized Ratio) - the indicator should be from 2.0 to 3.0.
| The main drugs for patients with AF that prevent stroke are anticoagulants, the effect of which reduces blood clotting. With atrial fibrillation, anticoagulants are absolutely necessary for almost everyone. |
Classification of ventricular extrasystoles and (Lown, 1983).
1 tbsp. - single, rare monotonous extra-tables, no more than 60 per 1 hour (no more than 1 per 1 minute). Stage 2—frequent—monotopic extrasystoles, more than 1 per minute. 3st. - polytopic, frequent ventricular extrasystoles. 4st. - group ventricular extrasystoles (double and volley). 5th stage - early extrasystoles, type “R” to “T” and extra early.
3-5 tbsp. - these are extrasystoles of high gradation, indicate myocardial damage, are prognostically unfavorable (can develop into more serious rhythm disturbances).
With ischemic heart disease, almost all of the listed cardiac arrhythmias are possible, usually in combination with other manifestations of the disease: angina pectoris, myocardial infarction, heart failure. Thus, in the acute period of myocardial infarction, rhythm disturbances are recorded in almost all patients. 60-80% of patients with coronary artery disease die suddenly due to ventricular fibrillation (E. Chazov, 1985; Lown, 1983).
Indications:
patient complaints of heart rhythm disturbances not documented by ECG; identification of asymptomatic arrhythmias in individuals at high risk of their occurrence (hypertrophic cardomnopathy, aortic stenosis, etc.); examination of the ability to work of persons engaged in professions related to the performance of work, the sudden cessation of which could harm others (pilot, dispatcher, driver, etc.); syncope of unknown origin.
3. EPI - transesophageal. 4. Endocardial EPI and programmed electrical stimulation of the heart.
TREATMENT
A. Drug treatment. Classification of antiarrhythmic drugs: Group I (membrane stabilizing agents) A: quinidine, novocainamide, etc.; B: Lidocaine, diphenylhydantoin; C: ajmaline, ethmoznn, etacizin, allapinin. Group II (beta-blockers). Group III (drugs that slow down repolarization): amiodarone, bretylium tosylate. Group IV (calcium antagonists): verapamil, nifedipine.
Any antiarrhythmic drug can cause both antiarrhythmic and arrhythmogenic effects. The probability of an antiarrhythmic effect for most drugs is on average 50% and very rarely, only in a few clinical forms of arrhythmias, reaches 90-100%: a) relief of reciprocal atrioventricular tachycardia using intravenous administration of ATP, adenosine or verapamil; b) relief and prevention of paroxysmal tachycardia with complexes such as right bundle branch block and sharp deviations of the heart axis to the left with the help of verapamil; c) elimination of ventricular extrasystole with etacizine, flecainide.
In all other cases, the selection of antiarrhythmic therapy will be done by trial and error. In this case, the probability of an arrhythmogenic effect is on average 10%, in some cases life-threatening for the patient. The more severe the rhythm disturbances and the degree of myocardial damage, the higher the risk of an arrhythmogenic effect. Therefore, at present, most researchers believe that for asymptomatic and low-symptomatic arrhythmias, as a rule, the prescription of antiarrhythmic drugs is not required (A. S. Smetnen et al., 1993).
If drug therapy is necessary, the selection of antiarrhythmic drugs is based on the nature of the rhythm disturbance.
How to treat atrial fibrillation?
Atrial fibrillation is difficult to treat. Drug therapy is aimed at correcting atrial rhythm and preventing attacks.
The following drugs are used: quinidine (quinipek, kinylentine, kinitard), procainamide (novocainamide), propafenone (propanorm, propastad, profenan), esmolol (breviblok), metoprolol (vasocardin, corvitol, metolol), propranolol (anaprilin, prolol, obzidan), amiodarone (aldarone, sedacorone, cardiodarone), sotalol (darob, loritmic, sotahexal), diltiazem (diazem, diacordin, Herbesser), verapamil (isoptin, veramil, danistol), digoxin (dilanacin, lanicor), korglykon (lily of the valley leaf glycoside), as well as many other drugs of different groups.
To prevent thrombosis, acetylsalicylic acid (aspirin) is prescribed. To stop attacks of atrial fibrillation, electrical cardioversion is used - a current discharge synchronizes the atrial rhythm.
Therapy is prescribed taking into account the cause of the pathology and the patient’s condition. The dosage and method of administration of drugs (orally or intravenously) depend on the form of atrial fibrillation. Invasive (surgical) treatment is also carried out.
Special forms of rhythm disturbance:
1. WPW syndrome: cordarone, ethmozin, gilurythmal (ajmalin). Contraindicated: cardiac glycosides and partially isoptic. 2. Sick sinus syndrome: rhythmylene, quinidine (under control of sinus node activity).
B. Non-drug treatment methods. 1. Electrical defibrillation. 2. Electrical stimulation of the heart.
B. Surgical treatment. 1. Intersection of additional pathways. 2. Removal, destruction or isolation of arrhythmogenic foci in the heart. 3. Cardiac stimulation (permanent, temporary). 4. Destruction of the atrioventricular node with implantation of a pacemaker.
Severity of heart rhythm disturbances. The severity of heart rhythm disturbances is determined by:
a) the frequency of their occurrence (paroxysmal form); b) duration (paroxysmal form); c) hemodynamic state; d) actual and probable complications: heart failure (acute and chronic); acute coronary insufficiency or progressive chronic; acute cerebrovascular insufficiency or progressive chronic; thromboembolic complications; syncope or sudden death.
In terms of assessing work capacity, it is inappropriate to separate different forms of NSR and conductivity according to their severity and prognostic significance.
1. Mild degree (insignificant NSR and conductivity): supraventricular and ventricular extrasystoles (I-II gradations according to Lown); brady- or normosystolic constant form of atrial fibrillation; sick sinus syndrome with a rhythm frequency of more than 50 per minute; paroxysms of atrial fibrillation and supraventricular tachycardia, occurring once a month or less, lasting no more than 4 hours and not accompanied by subjectively perceived changes in hemodynamics; A-B blockade of the 1st degree and 2nd degree (Mobitz type I); mono- and bifascicular blockades of the branches of the His bundle.
2. Moderate severity: polytopic frequent (1: 10) ventricular extrasystole (III gradation according to Lown); paroxysms of atrial fibrillation, atrial flutter; supraventricular tachycardia, occurring 2-4 times a month, lasting more than 4 hours, accompanied by changes in hemodynamics felt by patients; conduction disorders: A-B Mobitz block II and III degrees, tri-fascicular block of the branches of the His bundle, sick sinus syndrome, sinoauricular block III degree, junctional rhythm with a heart rate of more than 40 per minute and the absence of HF.
3. Severe degree: ventricular extrasystole - frequent polytopic, volley, early (IV-V gradations according to Lown); paroxysms of atrial fibrillation, atrial flutter, supraventricular tachycardia, occurring several times a week, accompanied by pronounced changes in hemodynamics, difficult to tolerate by patients; paroxysms of ventricular tachycardia; a permanent form of atrial fibrillation, tachysystolic atrial flutter, not corrected by medications and accompanied by progressive heart failure; sick sinus syndrome, trifascicular His bundle block, Frederick's syndrome with heart rate less than 40 per minute, attacks of MES and syncope, progressive heart failure.
Functionally significant deterioration of hemodynamics as a result of rhythm and conduction disturbances, the emergence or increase in the severity of heart failure is determined not only by the form of NSR, but also by the initial state of the myocardium (cardiosclerosis) and coronary and cerebral arteries (atherosclerosis).
Thromboembolic complications, syncope and sudden death can occur when NSR and conduction are the only manifestation of the disease: congenital anomalies of the cardiac conduction system; isolated damage to the artery supplying the sinus node, isolated focal cardiosclerosis involving the conduction system of the heart, non-progressive hypertrophic cardiomyopathy.
Medical and social examination
Medical and social examination and disability in cases of heart rhythm disorders DEFINITION Heart rhythm disturbances (arrhythmias) are understood as any heart rhythm that is not a regular sinus rhythm of normal frequency, caused by changes in the basic functions of the heart - automatism, excitability, conductivity or their combined disturbance. CLASSIFICATION of cardiac arrhythmias (V.L. Doshchitsin, 1991). I. Impairment of impulse formation. 1. Sinus tachycardia. 2. Sinus bradycardia. 3. Sinus arrhythmia. 4. Migration of the rhythm source. 5. Extrasystole: a) suprapentricular and ventricular; b) single, group, allorhythmic. 6. Paroxysmal tachycardia: a) supraventricular and ventricular; b) paroxysmal and constantly recurrent. 7. Non-paroxysmal tachycardia and accelerated ectopic rhythms - supraventricular and ventricular. 8. Atrial flutter: a) paroxysmal and persistent; b) regular and irregular shapes. 9. Atrial fibrillation: a) paroxysmal and persistent; b) tachysystolic and bradysystolic forms. 10. Flickering (fibrillation) and ventricular flutter. II. Conduction disorders. 1. Sinoatrial blockade—complete and incomplete. 2. Intraatrial block - complete and incomplete. 3. Atrioventricular block: a) I, II and III degrees; b) proximal and distal. 4. Intraventricular block: a) mono-, bi- and tri-fascicular, focal, arborptic; b) complete and incomplete. III. Combined arrhythmias. 1. Sick sinus syndrome. 2. Escaping (slipping) contractions and rhythms - supraventricular and ventricular. 3. Syndromes of premature excitation of the ventricles. 4. Parasystoles. 5. Long QT syndrome. Classification of ventricular extrasystoles and (Lown, 1983). 1 tbsp. - single, rare monotonous extra-tables, no more than 60 per 1 hour (no more than 1 per 1 minute). Stage 2—frequent—monotopic extrasystoles, more than 1 per minute. 3st. - polytopic, frequent ventricular extrasystoles. 4st. - group ventricular extrasystoles (double and volley). 5th stage - early extrasystoles, type “R” to “T” and extra early. 3-5 tbsp. - these are extrasystoles of high gradation, indicate myocardial damage, are prognostically unfavorable (can develop into more serious rhythm disturbances). With ischemic heart disease, almost all of the listed cardiac arrhythmias are possible, usually in combination with other manifestations of the disease: angina pectoris, myocardial infarction, heart failure. Thus, in the acute period of myocardial infarction, rhythm disturbances are recorded in almost all patients. 60-80% of patients with coronary artery disease die suddenly due to ventricular fibrillation (E. Chazov, 1985; Lown, 1983). Diagnostic methods 1. ECG at rest and during dosed physical activity (VEM). 2. Daily (Holter) monitoring. Indications: patient complaints of heart rhythm disturbances not documented by ECG; identification of asymptomatic arrhythmias in individuals at high risk of their occurrence (hypertrophic cardomnopathy, aortic stenosis, etc.); examination of the ability to work of persons engaged in professions related to the performance of work, the sudden cessation of which could harm others (pilot, dispatcher, driver, etc.); syncope of unknown origin. 3. EPI - transesophageal. 4. Endocardial EPI and programmed electrical stimulation of the heart. Indications: repeated episodes of ventricular fibrillation; severe attacks of ventricular tachycardia; frequent and severe attacks of supraventricular tachycardia; syncope of presumably arrhythmic origin; indications for surgical treatment of arrhythmias; selection of drug antiarrhythmic therapy. TREATMENT A. Drug treatment. Classification of antiarrhythmic drugs: Group I (membrane stabilizing agents) A: quinidine, novocainamide, etc.; B: Lidocaine, diphenylhydantoin; C: ajmaline, ethmoznn, etacizin, allapinin. Group II (beta-blockers). Group III (drugs that slow down repolarization): amiodarone, bretylium tosylate. Group IV (calcium antagonists): verapamil, nifedipine. Any antiarrhythmic drug can cause both antiarrhythmic and arrhythmogenic effects. The probability of an antiarrhythmic effect for most drugs is on average 50% and very rarely, only in a few clinical forms of arrhythmias, reaches 90-100%: a) relief of reciprocal atrioventricular tachycardia using intravenous administration of ATP, adenosine or verapamil; b) relief and prevention of paroxysmal tachycardia with complexes such as right bundle branch block and sharp deviations of the heart axis to the left with the help of verapamil; c) elimination of ventricular extrasystole with etacizine, flecainide. In all other cases, the selection of antiarrhythmic therapy will be done by trial and error. In this case, the probability of an arrhythmogenic effect is on average 10%, in some cases life-threatening for the patient. The more severe the rhythm disturbances and the degree of myocardial damage, the higher the risk of an arrhythmogenic effect. Therefore, at present, most researchers believe that for asymptomatic and low-symptomatic arrhythmias, as a rule, the prescription of antiarrhythmic drugs is not required (A. S. Smetnen et al., 1993). If drug therapy is necessary, the selection of antiarrhythmic drugs is based on the nature of the rhythm disturbance. Supraventricular rhythm disturbances. 1. Acute (extrasystole, paroxysmal atrial fibrillation, atrial flutter): procainamide, quinidine; (paroxysmal tachycardia): physical methods, isoptin, ATP, beta-blockers. 2. Prevention of paroxysms: cordarone, quinidine, beta-blockers. Ventricular rhythm disturbances. 1. Acute (extrasystole, paroxysmal tachycardia, fibrillation): lidocaine, nonocainamnd, etacizium, cordarone. 2. Prevention of paroxysms: cordarone, quinidine, diphenylhydantoin, novocainamide. Special forms of rhythm disturbance: 1. WPW syndrome: cordarone, ethmosin, gilurythmal (ajmalin). Contraindicated: cardiac glycosides and partially isoptic. 2. Sick sinus syndrome: rhythmylene, quinidine (under control of sinus node activity). B. Non-drug treatment methods. 1. Electrical defibrillation. 2. Electrical stimulation of the heart. B. Surgical treatment. 1. Intersection of additional pathways. 2. Removal, destruction or isolation of arrhythmogenic foci in the heart. 3. Cardiac stimulation (permanent, temporary). 4. Destruction of the atrioventricular node with implantation of a pacemaker. MSE IN NSR IS DETERMINED BY THE FOLLOWING MAIN FACTORS: a) the severity of rhythm disturbances; b) the nature of the disease that caused the rhythm disturbances; c) the presence of contraindicated working conditions; d) the nature of the treatment (medicinal, surgical). Severity of heart rhythm disturbances. The severity of heart rhythm disturbances is determined by: a) the frequency of their occurrence (paroxysmal form); b) duration (paroxysmal form); c) hemodynamic state; d) actual and probable complications: heart failure (acute and chronic); acute coronary insufficiency or progressive chronic; acute cerebrovascular insufficiency or progressive chronic; thromboembolic complications; syncope or sudden death. In terms of assessing work capacity, it is inappropriate to separate different forms of NSR and conductivity according to their severity and prognostic significance. 1. Mild degree (insignificant NSR and conductivity): supraventricular and ventricular extrasystoles (I-II gradations according to Lown); brady- or normosystolic constant form of atrial fibrillation; sick sinus syndrome with a rhythm frequency of more than 50 per minute; paroxysms of atrial fibrillation and supraventricular tachycardia, occurring once a month or less, lasting no more than 4 hours and not accompanied by subjectively perceived changes in hemodynamics; A-B blockade of the 1st degree and 2nd degree (Mobitz type I); mono- and bifascicular blockades of the branches of the His bundle. 2. Moderate severity: polytopic frequent (1: 10) ventricular extrasystole (III gradation according to Lown); paroxysms of atrial fibrillation, atrial flutter; supraventricular tachycardia, occurring 2-4 times a month, lasting more than 4 hours, accompanied by changes in hemodynamics felt by patients; conduction disorders: A-B Mobitz block II and III degrees, tri-fascicular block of the branches of the His bundle, sick sinus syndrome, sinoauricular block III degree, junctional rhythm with a heart rate of more than 40 per minute and the absence of HF. 3. Severe degree: ventricular extrasystole - frequent polytopic, volley, early (IV-V gradations according to Lown); paroxysms of atrial fibrillation, atrial flutter, supraventricular tachycardia, occurring several times a week, accompanied by pronounced changes in hemodynamics, difficult to tolerate by patients; paroxysms of ventricular tachycardia; a permanent form of atrial fibrillation, tachysystolic atrial flutter, not corrected by medications and accompanied by progressive heart failure; sick sinus syndrome, trifascicular His bundle block, Frederick's syndrome with heart rate less than 40 per minute, attacks of MES and syncope, progressive heart failure. Functionally significant deterioration of hemodynamics as a result of rhythm and conduction disturbances, the emergence or increase in the severity of heart failure is determined not only by the form of NSR, but also by the initial state of the myocardium (cardiosclerosis) and coronary and cerebral arteries (atherosclerosis). Thromboembolic complications, syncope and sudden death can occur when NSR and conduction are the only manifestation of the disease: congenital anomalies of the cardiac conduction system; isolated damage to the artery supplying the sinus node, isolated focal cardiosclerosis involving the conduction system of the heart, non-progressive hypertrophic cardiomyopathy. Contraindicated working conditions: 1. Working conditions contraindicated for the underlying disease that caused NSR and conductivity (coronary artery disease, rheumatism and others). 2. The presence or risk of ventricular arrhythmias and asystole: work that poses a danger to others and the patient in the event of its sudden cessation (driver, pilot, railway and aeroflot dispatcher, work at height and in extreme conditions). In most cases of NSD, the ability of patients to work is determined by the underlying disease that was their cause. Difficulties in MSE, as a rule, arise more often when the only manifestation of the pathological process is a violation of rhythm and conduction. Able to work: 1. Insignificant (mild) rhythm disturbances. 2. Average severity of rhythm disturbances with the exception of contraindicated labor factors. Reduced ability to work (limited ability to work - disability group III): 1. Severe degree of rhythm disturbance. Heart rhythm and conduction disturbances, as a rule, do not have independent significance in permanent disability and are considered in combination with the underlying disease that caused their occurrence. It should be taken into account that NSR and severe conduction may contribute to the progression of heart failure and indicate a high risk of sudden death. The greatest difficulties arise when it is necessary to assess the ability to work and rationally employ patients with continuous electrical cardiac stimulation (PECS). This method is currently widely used for the treatment of the following NSR and conduction: acquired complete A-B block in the presence of MES attacks and a heart rate of less than 40 beats per minute; congenital permanent A-B block with a heart rate less than 50 beats per minute; A-B blockade of the second degree (Mobitz II); blockade of both bundle branches; sick sinus syndrome, tachybradcardia syndrome; supraventricular paroxysmal tachycardia and atrial fibrillation, resistant to drug therapy; WPW syndrome. Indications for referring patients with implanted pacemakers to MSE: 1. To extend the duration of VUT in cases of effective pacemaker implantation and a favorable clinical and labor prognosis in the following cases: - the presence of complications in the postoperative period (pleurisy, pericarditis, etc.); - heart rhythm disturbances of moderate severity (for example, ventricular extrasystole more than 6-8 per minute, parasystole, etc.), requiring active and long-term drug therapy; — presence of signs of the initial stage of heart failure; disorders of psychological adaptation to ECS requiring psychotherapeutic correction. 2. To determine the disability group for persons of working age: - the presence of absolute medical contraindications to the continuation of the previous professional activity and the need, in connection with this, to transfer to another job with a reduction in volume, qualifications or a change in profession; — ineffectiveness of PEX, as a result of which attacks of NSR and conduction persist, which is accompanied by significant dysfunction of the cardiovascular system; — presence of complications of PEX requiring long-term treatment; - absolute dependence of the patient on PEX; - worsening of the underlying disease. 3. Re-examination of disabled people with PEX. The required minimum of research when referring a patient for medical examination. The required amount of research is determined by the underlying disease and includes: a) the results of a study of the degree of dependence of the patient on the pacemaker; b) ECG at rest; VEM test (threshold power - 75 W); c) daily monitoring (according to indications); d) integral rheography or echocardiography; e) chest x-ray; f) consultation with a psychotherapist. Contraindicated working conditions (absolute): 1. Work associated with exposure to strong static charges, magnetic fields and pronounced effects of microwave fields. 2. Work related to electrolytes and under conditions of exposure to strong induction of thermal and light radiation from stoves and radiators. 3. Work related to the maintenance of existing powerful electrical installations. 4. Work in conditions of severe vibration. 5. Work associated with constant or episodic significant physical stress throughout the entire working day, at a prescribed pace, and in a forced body position. 6. Work associated with potential danger to others due to its sudden cessation by patients. Patients should be considered able to work if they are effectively treated with a permanent pacemaker: the disappearance of previously existing PSR and conductivity, significant or complete regression of HF phenomena, and the absence of complications in the postoperative period. As a result, in such patients, after 1.5-2 months, the quality of life improves, a normal psychological reaction is established, the required level of physical activity is achieved, and they can resume their professional activities in professions of mental or light physical labor. A necessary condition for the restoration of working capacity is the patient’s independence from the pacemaker: the emergence of his own heart rhythm after suppression of the pacemaker. Disability criteria In case of pathology of the cardiovascular system (including heart rhythm disturbances), the decisive criterion for establishing disability is the stage of CHF (chronic heart failure). The relationships between the stages of CHF and disability are as follows: With CHF 0 and CHF 1st. - disability is not established. With CHF 2Ast. — 3rd disability group in adults (category “disabled child” in children). With CHF 2Bst. — 2nd disability group in adults (category “disabled child” in children). With CHF stage 3. — 1st disability group in adults (category “disabled child” in children). The above ratios apply provided that the patient has a PERSISTENT (not treatable for at least the last 4-6 months before MSA) corresponding stage of CHF. Exceptions to the above ratios are cases where a child (a person under the age of 18 years) has: - an implanted pacemaker (in this case, the category “disabled child” is established regardless of the stage of CHF, i.e. even with CHF stage 0); — the presence of a vascular implant that periodically requires replacement due to the growth of the child (in this case, the category “disabled child” is also established regardless of the stage of CHF, i.e. even with CHF stage 0).A patient can receive an official conclusion on the presence (or absence) of grounds for establishing disability only based on the results of his examination at the ITU Bureau relevant region
.
The procedure for completing documents for undergoing MSE (including the algorithm of actions in case of refusal of attending physicians to refer a patient to MSE) is described in sufficient detail in this section of the forum: Registration of disability in simple language
Source
Contraindicated working conditions:
1. Working conditions contraindicated in case of the underlying disease that caused NSR and conductivity (IHD, rheumatism, and others). 2. The presence or risk of ventricular arrhythmias and asystole: work that poses a danger to others and the patient in the event of its sudden cessation (driver, pilot, railway and aeroflot dispatcher, work at height and in extreme conditions).
In most cases of NSD, the ability of patients to work is determined by the underlying disease that was their cause. Difficulties in MSE, as a rule, arise more often when the only manifestation of the pathological process is a violation of rhythm and conduction.
How does atrial fibrillation manifest?
Atrial fibrillation often may not reveal itself in any way. The most common symptoms are palpitations, shortness of breath, chest pain, dizziness, weakness or fainting. Sometimes these manifestations are combined with increased frequency of urination. Fainting and angina are much less common symptoms of atrial fibrillation.
On clinical examination, an irregular pulse is noted; There is a continuous fluctuation in blood pressure values. In most cases, the pulse is frequent (with a tachysystolic form).
More often, an attack of atrial fibrillation occurs for no apparent reason; less often it is associated with alcohol abuse, strong coffee, smoking, stress, and excessive physical activity.
Able-bodied:
1. Insignificant (mild) rhythm disturbances. 2. Average severity of rhythm disturbances with the exception of contraindicated labor factors.
Reduced ability to work (limited ability to work - disability group III): 1. Severe degree of rhythm disturbance. Heart rhythm and conduction disturbances, as a rule, do not have independent significance in permanent disability and are considered in combination with the underlying disease that caused their occurrence. It should be taken into account that NSR and severe conduction may contribute to the progression of heart failure and indicate a high risk of sudden death.
The greatest difficulties arise when it is necessary to assess the ability to work and rationally employ patients with continuous electrical cardiac stimulation (PECS).
This method is currently widely used for the treatment of the following NSR and conduction: acquired complete A-B block in the presence of MES attacks and a heart rate of less than 40 beats per minute; congenital permanent A-B block with a heart rate less than 50 beats per minute; A-B blockade of the second degree (Mobitz II); blockade of both bundle branches; sick sinus syndrome, tachybradcardia syndrome; supraventricular paroxysmal tachycardia and atrial fibrillation, resistant to drug therapy; WPW syndrome.
How does atrial fibrillation occur?
Atrial fibrillation affects approximately 1% of adults worldwide. The frequency of this pathology among adults doubles with every decade of life. In addition to old age, risk factors for the development of MA include organic diseases of the cardiovascular system: arterial hypertension (hypertension), coronary heart disease (CHD), mitral valve defects (stenosis, insufficiency) usually of a rheumatic nature, as well as increased function of the thyroid gland (hyperthyroidism) .
However, less than a tenth of patients with this pathology do not have any organic heart disease. Atrial fibrillation can also be caused by conditions that are not accompanied by structural changes in the atria: intoxication, hypoxia (oxygen starvation) of the myocardium).
For any of the reasons described above, electrical impulses begin to appear chaotically in the atria. Abnormal electrical activity causes the muscle fibers of the atria to contract erratically, called fibrillation. Atrial fibrillation looks like twitching of the atrial muscle bundles separately, “in discord.” Because of this, the atrium does not contract completely. For this reason, the phase of active blood ejection from the atria is disrupted (cardiac output decreases).
As a result of these disorders, exercise tolerance decreases and symptoms of heart failure increase (shortness of breath, swelling of the legs, etc.). In the enlarged chambers of the heart, blood stagnates and thickens, thus forming blood clots that are life-threatening. Blood clots can enter the arteries of vital organs, such as the brain, and clog them - increasing the risk of thromboembolism.
Indications for referral to MSE for patients with implanted pacemakers:
1. To extend the duration of VUT in cases of effective pacemaker implantation and a favorable clinical and labor prognosis with: - the presence of complications in the postoperative period (pleurisy, pericarditis, etc.); - heart rhythm disturbances of moderate severity (for example, ventricular extrasystole more than 6-8 per minute, parasystole, etc.), requiring active and long-term drug therapy; — presence of signs of the initial stage of heart failure; disorders of psychological adaptation to ECS requiring psychotherapeutic correction.
2. To determine the disability group for persons of working age: - the presence of absolute medical contraindications to the continuation of the previous professional activity and the need, in connection with this, to transfer to another job with a reduction in volume, qualifications or a change in profession; — ineffectiveness of PEX, as a result of which attacks of NSR and conduction persist, which is accompanied by significant dysfunction of the cardiovascular system; — presence of complications of PEX requiring long-term treatment; - absolute dependence of the patient on PEX; - worsening of the underlying disease.
3. Re-examination of disabled people with PEX.
What is ITU?
Medical and social examination (MSE) is an examination at the state level of a person’s needs for social protection, for which the degree of restrictions in the activity of vital organs is assessed, which led to persistent impairment of the functions of the whole organism.
Patients are referred to MSE by treatment and preventive institutions that are subordinate to the Ministry of Health. Medical and social expert commissions created on the basis of the same state medical institutions take part in determining disability. The commission is headed by the chief physician, who is approved for the position by the head of the health department of the city administration.
Video: Rules for referral to ITU
Contraindicated working conditions (absolute):
1. Work associated with being in conditions of strong static charges, magnetic fields and pronounced effects of microwave fields. 2. Work related to electrolytes and under conditions of exposure to strong induction of thermal and light radiation from stoves and radiators. 3. Work related to the maintenance of existing powerful electrical installations. 4. Work in conditions of severe vibration. 5. Work associated with constant or episodic significant physical stress throughout the entire working day, at a prescribed pace, and in a forced body position. 6. Work associated with potential danger to others due to its sudden cessation by patients.
Patients should be considered able to work if they are effectively treated with a permanent pacemaker: the disappearance of previously existing PSR and conductivity, significant or complete regression of HF phenomena, and the absence of complications in the postoperative period. As a result, in such patients, after 1.5-2 months, the quality of life improves, a normal psychological reaction is established, the required level of physical activity is achieved, and they can resume their professional activities in professions of mental or light physical labor. A necessary condition for the restoration of working capacity is the patient’s independence from the pacemaker: the emergence of his own heart rhythm after suppression of the pacemaker.
Disability criteria
Group III: after the operation, there is an improvement in the general condition of the patients, but they have: a) a positive VEM test; b) moderate disorders of the circulatory system; c) the presence of a persistent psychopathological reaction to pacemaker implantation with personality changes; d) the need for employment in non-contraindicated working conditions, with a decrease in the volume of production activities, qualifications or a change in profession.
Group II: ineffectiveness of surgical treatment using the PEX method: a) previous NSR and conductivity are preserved; b) interference of ECS and own rhythms; c) pronounced manifestations of coronary and heart failure (angina pectoris class III—IV, heart failure stage IIB—III); d) absolute dependence on the ECS.
What examinations do you need to undergo before ITU?
Patients referred for medical and social examination must first undergo a series of studies, including the following types of diagnostics:
- Electrocardiography in a calm state.
- Echocardiography or integral rheography.
- Bicycle ergometry with a threshold power of about 75 W.
- Holter (24-hour) monitoring of cardiac activity.
- X-ray of the chest organs.
- Advisory opinion of doctors of a narrow specialty (psychotherapist).