In defibrillation, the shock is delivered randomly in relation to the phase of the cardiac cycle. As a matter of common sense, the use of defibrillation should be limited to cardiopulmonary resuscitation. But situations are different. And sometimes defibrillation has to be used for the same indications as cardioversion. In this case, there is always a risk of developing ventricular fibrillation (about 0.4%). Repeated defibrillation, which must be carried out as soon as possible, usually restores the rhythm.
A defibrillator is a device that generates an electrical impulse of the required duration and power (measured in Joules). Based on the pulse shape, defibrillators are divided into monophasic and biphasic. The latter are considered the most effective. Medical advice: If you do not know what type of device your defibrillator is, consider it monophasic.
What it is?
Cardioversion is the resumption of heart rhythm during atrial fibrillation and other arrhythmias.
There are: medicinal, electric pulse and planned, as well as unscheduled. Anticoagulant therapy should be carried out during emergency cardioversion (IV Heparin) and always before planned cardioversion (Warfarin, Rivaroxaban three weeks before the procedure). The main forms of atrial fibrillation and the need for cardioversion for them:
- Paroxysmal – characterized by repeated episodes of flickering lasting no more than 48 hours, restoration of sinus rhythm occurs spontaneously.
- Persistent - one or more paroxysms are recorded that last more than seven days, the rhythm returns to normal after drug or electrical pulse cardioversion.
- Long-term persistent - lasts for more than a year by the time a decision is made about the need to resume the normal rhythm.
- Constant – rhythm restoration is not planned or is contraindicated.
- Silent - asymptomatic, manifests itself as complications of arrhythmia (ischemic stroke, tachycardiomyopathy) or is diagnosed accidentally.
Heart rhythm disturbances (arrhythmias)
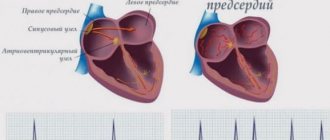
The heart is an incredibly complex organ. Its task is to collect the blood flowing to the heart through the veins and throw this blood into the arteries so that all cells of the body receive their share of nutrients and oxygen. Reacting to an increase in the nutritional needs of any organ or the whole organism, it increases the release of blood into the arteries. The heart consists of four chambers - two atria and two ventricles. In a healthy heart, the atria contract first, expelling the blood that entered them from the veins. Blood enters the ventricles of the heart. Contraction of the ventricles (systole) pushes blood into the arteries. In the right atrium, blood collects from the veins of the whole body, then it enters the right ventricle, from there it is released into the arteries of the lungs. In the lungs, the blood is enriched with oxygen, gives off carbon dioxide and is collected in the pulmonary veins. From there, the blood enters the left atrium, then into the left ventricle, and from there into the arteries of the body. The coordination of the heart is ensured by a special conduction system of the heart. These are specialized cells that produce and conduct electrical impulses that direct the coordinated contraction of the heart muscle. The impulse that triggers the contraction of the heart is produced in the right atrium, in the so-called sinus node (pacemaker). It is this node that is responsible for the fact that the heart contracts at a frequency of 60-90 beats per minute. The signal then spreads to the remaining atria, causing them to contract, and then to the ventricles. Disturbances in this system lead to heart rhythm disturbances (arrhythmias).
What are the types of arrhythmias?
Heart contractions follow each other at regular intervals. If this sequence is disrupted, the patient is said to have an arrhythmia. Depending on where the disturbances occur, all arrhythmias are divided into atrial (or supraventricular) and ventricular. Arrhythmia is not an independent disease, but a sign (symptom) of some disease. Therefore, the occurrence of arrhythmia requires mandatory examination by a cardiologist. The patient can detect the presence of arrhythmia himself. To do this, you need to learn to find and count the pulse.
Heart function (rhythms)
If the pulse rate exceeds 90 beats per minute, they speak of tachycardia. The heart rate may increase during physical or emotional stress (this is a normal reaction of a healthy heart). An increase in body temperature causes tachycardia. It is believed that an increase in body temperature by 1 degree leads to an increase in heart rate by 10 beats. Tachycardia can be a sign of many diseases, but it can also be a normal variant. Some types of tachycardia require special antiarrhythmic treatment. If the pulse rate is less than 60 beats per minute, they speak of bradycardia. Bradycardia can occur in absolutely healthy people. It is usually observed in athletes. Moderate bradycardia creates favorable conditions for the blood supply to the heart muscle. This is due to the fact that blood can only flow to it when it is in a state of relaxation (i.e. between contractions). The faster the rhythm, the more blood is needed to replenish the energy costs of the heart muscle, and the relaxation period becomes shorter. Therefore, some medications (for example, atenolol or anaprilin) that can slow down the rhythm (extend the period of relaxation) improve blood supply to the heart muscle. If bradycardia appears suddenly, if the slowdown in rhythm is accompanied by dizziness or loss of consciousness, consult a doctor immediately. You should also consult a doctor if your heart rate is less than 50 per minute and there are no other unfavorable signs. In some forms of bradycardia, it is necessary to implant a special device - a pacemaker. This device takes over control of the heart rhythm when its own pacemaker (sinus node) fails to cope with its task.
Extrasystole
If a premature contraction is woven into the correct rhythm of heart contractions, they speak of extrasystole. According to the place from which the electrical impulse emanates, leading to premature contraction, all extrasystoles are divided into atrial and ventricular. Even an absolutely healthy person can experience extrasystoles several times a day. However, their appearance is a reason to consult a cardiologist. Like all arrhythmias, extrasystole is not an independent disease, but only a sign of some disease. The examination will be aimed at finding the cause of the arrhythmia. Atrial fibrillation is the most common arrhythmia
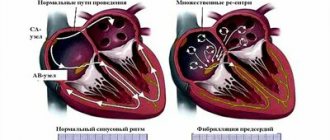
What is atrial fibrillation
Atrial fibrillation is a type of rhythm disorder in which the atria are excluded from the coordinated work of the heart. An electrical impulse runs at high frequency through the atria, causing chaotic contraction of muscle fibers (fibrillation). Therefore, atrial fibrillation is also sometimes called atrial fibrillation. Some impulses break through to the ventricles, which contract due to this in an incorrect, irregular rhythm. The absence of the correct rhythm is the main sign of atrial fibrillation. Sometimes it is not possible to identify the cause of atrial fibrillation, then they talk about its idiopathic form. Most often, atrial fibrillation is a sign of heart disease, coronary heart disease, arterial hypertension, etc. Not only cardiovascular diseases can lead to atrial fibrillation. Common causes include diseases of the thyroid gland, lungs, acute and chronic poisoning (for example, alcohol) and many other diseases. It is important that for success in the treatment of atrial fibrillation, it is necessary not only to correctly prescribe special antiarrhythmic drugs, but also to correct its cause.
Manifestations (symptoms) of atrial fibrillation
The most common manifestation of atrial fibrillation is a feeling of palpitations. It is due to the fact that the average ventricular rhythm during atrial fibrillation usually increases and can reach 130-150 beats per minute. Interruptions in the functioning of the heart are often felt, sometimes a sharp feeling of lack of air, pain in the heart area, and dizziness. Approximately 1 in 10 patients does not feel the appearance of atrial fibrillation at all.
Types of atrial fibrillation
Long-term atrial fibrillation is called permanent. If it occurs paroxysmally, they speak of the paroxysmal form. Atrial fibrillation with a high heart rate is called tachysystolic, with a normal frequency - normosystolic and with a low frequency - bradysystolic form.
Is it necessary to treat atrial fibrillation?
According to various estimates, from 1.5 to 5% of humanity suffers from this type of arrhythmia. This is the most common type of arrhythmia requiring treatment. The appearance of atrial fibrillation (if left untreated) significantly (5-7 times) increases the risk of stroke and pulmonary embolism. The likelihood of developing heart failure also increases. Additional factors such as age and the presence of severe concomitant diseases further increase the risk of stroke and heart failure in patients with atrial fibrillation. Therefore, atrial fibrillation must be treated without fail.
Restoring the correct heart rhythm
The goal of treatment for a patient suffering from atrial fibrillation is, if possible, the restoration of the sinus (correct) heart rhythm and its subsequent maintenance. There are several ways to restore the correct rhythm. The first - the simplest - can be tried by the patient himself. The method is based on the possibility of stimulating the vagus, a nerve that slows down the heart rate. You need to take a deep breath. Then hold your nose and mouth tightly and try to exhale forcefully. This method can also stop other attacks of palpitations. Unfortunately, this method does not help all patients. The most common is restoring the heart rhythm with the help of medications. These medications are called antiarrhythmics. Typically, medications are administered intravenously. However, in some cases, the patient himself can take a previously selected medicine, which stops the attack of atrial fibrillation. Unfortunately, there are no special signs to determine which medicine will be more effective. In practice, you have to try several medications before choosing the drug that is most suitable for the patient. In some cases, when an attack of atrial fibrillation cannot be treated with medications, if it has existed for a long time, there is an immediate threat to the patient’s life, so-called electrical cardioversion is used to restore the rhythm. The patient falls asleep for a short time (1-2 minutes), then a special synchronized (i.e. applied at a certain phase of the cardiac cycle) electric current discharge restores the heart rhythm. The method has several disadvantages - the need to put the patient to sleep, the need for special equipment to carry out the procedure. In addition, this procedure must be performed in a hospital that has highly trained personnel. But there are also significant advantages. Thus, the rhythm is restored in almost all cases (unlike drugs, which restore the rhythm only in 60-80%). This method is the safest, since any medicine has side effects. If they appear, then it takes time for the medicine to leave the blood. Taking these advantages into account, special devices sewn under the skin - cardioverters - were created that detect atrial fibrillation and stop it. However, these devices are not yet widely used. After the rhythm is restored, it is necessary to maintain it. It is necessary to treat the disease that led to atrial fibrillation and eliminate the factors that provoke the attack. If attacks are rare, then sometimes special antiarrhythmic therapy is abstained. However, most often you have to take medicine to prevent the attack from developing. Sometimes, for frequent attacks that are difficult for patients to tolerate, surgical treatment has to be used.
Maintaining a normal heart rate when rhythm cannot be restored
In some cases, it is necessary to refuse to restore the normal rhythm. Usually in this case the patient has a so-called permanent form of atrial fibrillation. The main therapeutic measures are to maintain a normal heart rate and prevent complications.
Prevention of complications of atrial fibrillation
Since the main complications of atrial fibrillation are stroke and heart failure, their prevention should also be carried out in a patient with atrial fibrillation. The method of such prevention is chosen by your doctor.
Recommendations for a patient with atrial fibrillation
Try to find out and tell your doctor what precedes the next attack of atrial fibrillation. This may be unusual physical activity, increased blood pressure, taking any medications, drinking alcohol, exacerbation of lung disease, etc. Learn to count your pulse (or ask your doctor to teach you) and recognize whether you have atrial fibrillation or whether your heart rhythm is correct. If the attack does not go away on its own within 2-3 hours, does not go away with regular medications, or causes discomfort, pain, or shortness of breath, consult a doctor. The sooner from the moment the attack begins to treat it, the easier it is to restore the correct rhythm. Be sure to have your latest (or several recent) electrocardiograms with you. They may be needed for comparison in an emergency. Do not rely on your memory; have a sheet of paper with you with the name and dosage of the medications you are taking. This may be very important if you are being given a new medicine because many of the substances interact with each other. If you are taking phenylin or syncumar - medications that reduce prothrombin levels and prevent stroke and thromboembolism - do not forget to consult your doctor if:
- signs of bleeding appeared (nosebleeds, blood on the gums when biting, bruises began to appear)
- if you start taking new medications or change the dosage of previously taken medications
- if the diet has changed (for example, a new season has begun)
- if you have a cold, if you have an upset stomach, or any new illness. If you are planning any surgery or tooth extraction, tell your doctor that you are taking these medications.
Examination of a patient with arrhythmias
In order to properly treat arrhythmia, it is necessary to undergo a special examination. It consists of two parts. The first is the identification of the arrhythmia itself, the conditions for its occurrence and cessation. The second is the search for the disease that led to the arrhythmia. To detect an arrhythmia, it must be registered. To do this, an electrocardiogram is recorded. The desired arrhythmia is not always detected on a regular ECG. Therefore, the next step is to record an electrocardiogram over a long period of time (usually a day), then, using a special computer, the recording is deciphered. This examination method is called 24-hour Holter ECG monitoring. In some clinics, patients are given special devices to take home that allow them to transmit an ECG to their doctor if necessary. This method also allows you to record rare rhythm disturbances. Physical activity often provokes arrhythmias, so exercise testing is sometimes used to measure the level of acceptable physical activity and evaluate the preventive effect of antiarrhythmic drugs.
Use for atrial fibrillation
Indications for rhythm restoration:
- Patients with a first-time episode who have not spontaneously returned to sinus rhythm within 48 hours.
- People with arrhythmia caused by acute pathology (pneumonia, hyperthyroidism, alcohol consumption).
- Patients after resuming an adequate rhythm, if there is a choice of a method to maintain a normal heartbeat.
Drug cardioversion
Many episodes of arrhythmia stop spontaneously in the first hours or days after its onset. In patients with a persistent form or with unstable hemodynamics, despite a normal pulse, it is recommended to perform bolus (direct) administration of antiarrhythmic drugs. In some cases, outpatient patients undergo drug cardioversion for atrial fibrillation using the “pill in the pocket” principle.
To carry out pharmacological restoration of rhythm, several drugs can be used:
- Amiodarone (potassium and sodium channel blocker) is administered at a dose of 5 mg per kg of body weight intravenously over an hour, then the dose is 50 mg/hour. until the total dose reaches 1.2 mg per day (the rhythm is restored within 24 hours).
- “Flecainide” (class ІC antiarrhythmic drug) – 2 mg/kg, IV over 10 minutes. or 200-300 mg orally tableted. The drug is used in patients with a paroxysmal form and is not prescribed to patients with a persistent form. Resumption of sinus rhythm occurs within 6 hours. It can cause prolongation of the QRS complex and QT interval, as well as atrial flutter.
- “Ibutilin” (class III antiarrhythmic drug) – 1 mg IV drip, administered for 10 minutes, then pause for 10 minutes, then repeat. Rhythm restoration occurs quickly: within an hour. It stops flutter better than fibrillation. Can prolong QT and cause torsade de pointes.
- “Propafenone” (class ІC antiarrhythmic drug) – 2 mg per kg body weight intravenously, administered over 10 minutes. The normal rhythm is restored within 2 hours. Take 450-600 mg orally according to the instructions (the rhythm returns to normal within 6 hours - the “pill in your pocket” strategy).
- “Vernakalant” – 3 mg/kg IV for 10 minutes. The second infusion at a dose of 2 mg/kg IV over 10 minutes. after a pause of 15 minutes.
If the patient does not have organic damage to the heart, or it is minor, Flecainide and Propafenone can be used. In other cases, Amiodarone is more often used.
Electrical cardioversion
The antifibrillatory ability of electrical cardioversion in atrial fibrillation is caused by the depolarization of a “critical” number of cells, which occurs after the discharge and leads to the restoration of normal functioning of the sinus node. The most common method is external (transthoracic) cardioversion. The electrodes are placed: the first - above the apex of the heart, the second - under the right collarbone or under the left scapula. Considering the presence of pain and fear of the patient, general anesthesia, IV analgesia and sedation are used during the procedure.
Indications for the procedure:
- Lack of effect of drug antiarrhythmic therapy.
- Intolerance to antiarrhythmic drugs.
- Progressive heart failure due to tachyarrhythmia, symptoms of circulatory disorders.
- An indication in the medical history of the good effect of electrical pulse cardioversion in the treatment of tachyarrhythmia.
Contraindications to the procedure:
- Possible thrombus in the left atrium.
- Electrolyte imbalance.
- Glycoside intoxication.
- Contraindications to anesthesia from the respiratory system.
- Manifest hyperthyroidism.
- Alcohol intoxication.
- Acute infection.
- Decompensated heart failure.
- Documented SSU without IVR.
- Continuously relapsing AF.
Preparation includes, in addition to anticoagulant therapy, transesophageal echocardiography, multislice computed tomography.
Which discharge to use and how to perform it?
For fibrillation, use the first shock of 100 Joules. If the arrhythmia persists, then with each subsequent one the energy is increased by 50-100 J, to a maximum of 360 J. The interval between attempts should be minimal and is needed to assess the effectiveness of defibrillation.
Defibrillation
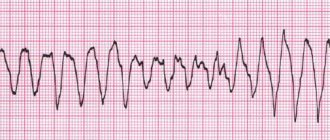
It is performed for the following rhythm disturbances. When performing cardiopulmonary resuscitation, defibrillation for these rhythm disturbances should be performed as early as possible. If more than 3 minutes have passed since the fatal cardiac arrhythmia, defibrillation should be preceded by chest compressions.
Children: initial power approximately 2 J/kg body weight, repeated defibrillation - 4 J/kg body weight.
Contraindications: refusal of resuscitation measures.
| Indications for defibrillation and recommended initial shock power for adult patients: | |||
| Type of arrhythmia | Pulse power in joules (J) | ||
| monophasic | biphasic | ||
| Ventricular fibrillation | 360 J or maximum power | 150-200 J | |
| Polymorphic ventricular tachycardia | 360 J or maximum power | 150-200 J | |
| Pulseless ventricular tachycardia | 360 J or maximum power | 150-200 J | |
Efficacy and prognosis
Pharmacological cardioversion for atrial fibrillation is effective only in 40-70% of cases, while electropulse cardioversion is effective in 90% of patients. After defibrillation, the patient should be monitored until recovery from sedation, and the rhythm should be assessed using an ECG, since complications are possible. It is difficult to predict how long the correct pulse will remain, since in many patients it does not last more than a year.
Surgical tactics are also used. Among them: radiofrequency, laser, microwave, ultrasound ablation, operation “Maze”, cryodestruction. Their cost is high, but their effectiveness and, most importantly, safety are the best. for Cardiovascular Surgery im. A. N. Bakuleva, Moscow.
Treatment options
There are two treatment tactics: monitoring the rhythm or frequency of the heart. The cardiologist determines how to treat arrhythmia and what to take individually, depending on the case.
Control of the rhythm of contractions - restoration of sinus, that is, normal, heart rhythm. It is achieved by taking antiarrhythmic drugs or electrical stimulation of the heart - cardioversion. Antiarrhythmic drugs have a positive effect on the electrical conductivity of the heart, thereby reducing the likelihood of repeated failures.
They may also prescribe ablation - the impact of radiofrequency pulses on the arrhythmic area of the heart.
Ablation treatment can be successful in 70% of cases or more: it depends on the severity and nature of the lesion, the duration of the arrhythmia, and the size of the heart cavities. Risks associated with the procedure are rare.
Monitoring your ventricular rate helps eliminate heart palpitations and the risk of heart failure. This method is used in cases where it has not been possible to restore a normal heart rhythm, or the patient does not show symptoms.
Frequency control is carried out in several ways:
- reduce the spread of electrical impulses from the atria to the ventricles with the help of drugs,
- ablation is performed to eliminate the delay in pulse propagation,
- a pacemaker is installed to simulate an electrical impulse.
Methods for restoring sinus rhythm
Electrical cardioversion.
Many experts believe that it is more effective than medication and does not cause proarrhythmia, therefore it is more preferable. Electrical cardioversion is a synchronized electrical shock (the use of shocks synchronized with the cardiac cycle). Cardioversion and defibrillation are often combined under the umbrella term “electropulse therapy” (EPT). The main method of EIT is external (transthoracic) electrodefibrillation or cardioversion, during which electrodes are placed on the chest. There is also a method of internal (pericardial) cardioversion: electrodes are directly in contact with the heart. For patients with resistance to transthoracic electrical discharges and severe supraventricular tachyarrhythmias, the transesophageal EIT method is used (one electrode is inserted into the esophagus at the level of the atria, the other is fixed in the area of cardiac dullness).
Pharmacological cardioversion.
The use of such drugs based on active ingredients such as propafenone (“Propanorm”), amiodarone, ibutilide, dofetilide and flecainide allows restoration of sinus rhythm in 60% of patients.
Draw your attention to! This article is not a call for self-medication. It is written and published to improve the reader's knowledge about his own health and understanding of the treatment regimen prescribed by the doctor. If you experience similar symptoms, be sure to seek help from a doctor. Remember: self-medication can harm you.