The meaning of the ancient Greek roots from which the term “chorioretinitis” is derived is as follows. The choroid is a network of blood vessels in the posterior wall of the eyeball that nourishes the retinal (retinal) tissue; The ending “-itis” in medical terminology always indicates inflammation. Thus, chorioretinitis is an inflammatory process that extends to both the retina and its vascular system. According to the type of course, chorioretinitis is divided into acute and chronic; by genesis (origin) - congenital and acquired.
Diagnostics
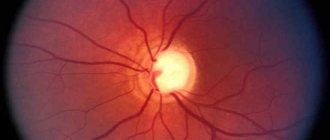
During ophthalmoscopy, you can detect retinal opacities in the macular area, which have a round or oval shape. The size of the opacification is 0.5-2 times the diameter of the optic nerve head. Usually the lesion protrudes slightly forward, and the vessels along its edge bend. The border of the lesion is emphasized using a light reflex.
The cloudiness can be expressed in varying degrees (from slight to intense gray). The defect is not always located in the foveal zone; it can be located paramacularly or eccentrically.
After a few months or days, the disease enters the second stage. This is called the precipitate stage. At this time, visual acuity can gradually recover, but the relative scotoma remains. There are no more retinal opacities in the fundus area, only gray-white small-pointed spots called precipitates remain.
At the third stage of chorioretinitis, metamorphopsia and central scotoma disappear, and visual acuity is restored. Both retinal edema and precipitates sometimes resolve without a trace, but dyspigmentation usually persists. The macula becomes mottled due to small clumps of pigment, areas of discoloration, and yellowish flat defects.
The process may involve one or both eyes, sometimes it has a recurrent course, and therefore the prognosis may be unfavorable. During an outpatient examination, it is quite difficult to identify signs of central serous chorioretinitis, since it has scanty symptoms. In this case, special examination techniques (ophthalmoscopy, biomicroscopy, fluorescein angiography) come to the rescue.
Differential diagnosis should be carried out with retrobulbar neuritis, juvenile macular degeneration, as well as other diseases. Characteristic features of central serous chorioretinitis include: widening of the optical section of the retina, the presence of transudate between the retina and the pigment epithelium, and small defects in the basal lamina. Fluorescein angiography reveals pinpoint dye leakage (so-called fluorescent flags).
Symptoms
The clinical picture of chorioretinitis significantly depends on the location of the inflammatory focus. Thus, central chorioretinitis is characterized by predominant damage to the macula (“macula”, the most light-sensitive and specialized area of the retina, responsible for the clarity of the central field of vision), equatorial and peripheral. There are also several options based on the nature of the focality: focal, multifocal (disseminated, divided into several separate foci) and diffuse, involving the entire retinal tissue without clear focal boundaries. Acute chorioretinitis can last up to three months, chronic chorioretinitis has a tendency to frequent relapses.
The content of subjective complaints is also determined by the localization of the inflammatory process. Thus, peripheral chorioretinitis often does not manifest itself at the level of subjective sensations at all - and in this case it is diagnosed by chance, during a consultation for another reason or during a medical examination. Macular chorioretinitis, on the contrary, manifests itself with multiple and varied visual disturbances: “fog before the eyes”, scotomas (blind or dark areas in the visual field), photopsia (illusory sparks or flashes of light), a noticeable decrease in the acuity and quality of vision. “Night blindness” is quite typical, as well as a distorted perception of the size and shape of objects observed by the patient.
Symptoms of this kind, no matter what the final diagnosis turns out to be, require immediate attention to an ophthalmologist.
Treatment
Treatment of the disease is usually complex; it must take into account the etiology of the pathology. Treatment that involves blocking defects in the basal lamina using laser coagulation is considered pathogenetic. After this manipulation, retinal edema disappears after 4-10 days. Additionally, medications are used that normalize the permeability of blood vessels and capillaries (Aevit, Ascorutin), dehydrating drugs (hypertonic solution of glucose, sodium chloride, glycerin, fonurite), vasodilating agents (nicotinamide, no-spa). To stimulate trophic processes, vitamins, ATP, cocarboxylase, and heparin are used. For retinal edema, corticosteroids are used in the form of a retrobulbar injection.
By contacting the Moscow Eye Clinic, each patient can be sure that some of the best Russian specialists will be responsible for the results of treatment. The high reputation of the clinic and thousands of grateful patients will certainly add to your confidence in the right choice. The most modern equipment for the diagnosis and treatment of eye diseases and an individual approach to the problems of each patient are a guarantee of high treatment results at the Moscow Eye Clinic. We provide diagnostics and treatment for children over 4 years of age and adults.
Chorioretinitis: causes
Among the causes of chorioretinitis, the following conditions can be identified, which are mainly associated with general diseases of the body:
- Infectious diseases (tuberculosis, syphilis, herpes, cytomegalovirus infection, toxoplasmosis), including local ones (ENT organs, oral cavity)
- Exposure to radiation
- Toxins (with prolonged hemophthalmia, destroyed blood cells can be toxic)
- Allergy
- Autoimmune disorders
- Sarcoidosis
- Immunodeficiencies (in HIV carriers, weakened people, during recovery after long-term treatment)
- Penetrating eye injuries.
Our doctors who will solve your vision problems:
Fomenko Natalia Ivanovna
Chief physician of the clinic, ophthalmologist of the highest category, ophthalmic surgeon. Surgical treatment of cataracts, glaucoma and other eye diseases.
Yakovleva Yulia Valerievna Refractive surgeon, specialist in laser vision correction (LASIK, Femto-LASIK) for myopia, farsightedness and astigmatism.
Gigineishvili Darejan Nugzarevna Retinologist, retina specialist, conducts diagnostics and laser treatment of retinal diseases (dystrophies, ruptures, hemorrhages).
You can find out the cost of a particular procedure or make an appointment at the Moscow Eye Clinic by calling in Moscow 8 (499) 322-36-36 (daily from 9:00 to 21:00) or using the ONLINE REGISTRATION FORM.
Causes
The main factors under the influence of which the retinal-vascular complex can become inflamed include:
- local and systemic infections caused by bacterial or viral pathogens (toxoplasmosis, herpes, and many others); the most common local primary sources of chorioretinitis are untreated infectious foci in adjacent organs - the nasopharynx and oral cavity;
- radiation (radiation) injury;
- intoxication, incl. products of decay of one’s own tissues (in particular, long-term non-resorbable blood after intraocular hemorrhage);
- allergic reactions;
- autoimmune disorders and diseases;
- immune deficiency (AIDS, exhaustion of various origins, recovery period after a major operation, etc.);
- ophthalmotrauma.
Symptoms of chorioretinitis
Regardless of the type of chorioretinitis diagnosed, all patients exhibit the following symptoms:
- The quality of vision is greatly reduced (this happens abruptly and for no particular reason);
- the patient sees a large number of black dots before his eyes;
- a person sees as if a plastic bag was covered from above the eye;
- disorientation in space (a person thinks that he is moving in one direction, but is actually heading in the opposite direction);
- decreased visual acuity with the onset of darkness (sometimes it is even impossible to distinguish one object from another);
- blind spots appear in a person’s field of vision;
- the visibility of colors is impaired (the patient cannot distinguish between them);
- the patient cannot understand what shape and size the object is;
- more acute stages are characterized by the fact that most objects are seen by a person as one large black spot.
Prevention of chorioretinitis
To reduce the risk of developing chorioretinitis, each person must adhere to several rules of prevention, which are as follows:
- treat infectious diseases in a timely manner (especially acute respiratory viral infections);
- in case of a sharp decrease in vision, immediately consult an ophthalmologist;
- do not stay in the cold for a long time;
- compliance with personal hygiene rules (especially hand washing);
- undergo routine medical examinations annually.
In particular, you need to visit the dentist regularly. Advanced caries can provoke inflammatory and purulent processes in the oral cavity, which can subsequently spread to the visual structures.
The prognosis of chorioretinitis with timely diagnosis and adequate treatment is favorable in most cases.
Diagnosis of chorioretinitis
To make a diagnosis of chorioretinitis, the patient will need to undergo a comprehensive examination, which will consist of both laboratory and instrumental methods.
Laboratory tests are necessary to identify the pathogen and determine its sensitivity to various antibiotics (Bacterial culture of the conjunctiva).
Also, blood tests make it possible to determine at what stage the disease is currently located, and with what intensity it is occurring. Laboratory diagnostics also allows you to determine the presence of autoimmune diseases (enzyme immunoassay). In addition to laboratory diagnostics, the patient will have to be examined by additional specialists who may prescribe the following procedures:
- Visometry
(allows you to determine a person’s level of vision and determine how much it has decreased). - Determination of intraocular pressure (IOP).
It is relevant only in cases where a severe and acute degree of the disease is diagnosed; it is during this period that the pressure will exceed the norm. - Gonioscopy
(makes it possible to detect the presence of pus or fluid in the anterior chamber of the eyeball). - Ophthalmoscopy
(detects inflammatory processes, minor hemorrhages, atrophy, and also evaluates macular pigmentation) is a routine procedure at every visit to the ophthalmologist. It is with such an examination that any changes in the functionality of the human visual system can be detected. - Fluorescein angiography
(diagnoses abnormalities in the vascular system of the eye). - Perimetry
(determines the level of a person’s field of vision).
{banner_gorizontalnyy2}
Based on the results of tests and studies, a diagnosis is made, and further tactics for treating the disease are outlined.
Possible complications of chorioretinitis
Complications of chorioretinitis can occur both with improper treatment and during the rehabilitation period after surgery on the eye, these include:
- retinal detachment;
- retinal vein blockage;
- neovascular membrane;
- repeated hemorrhages in the eyeball;
- complete loss of vision;
- inability to navigate in space and terrain;
- confusion of colors and shapes.
Some unpleasant symptoms may gradually decrease over time, and after a couple of months a person’s ability to navigate the area and distinguish colors and shapes is normalized.
If, after treatment, the initial symptoms reappear, then you will urgently need to visit an ophthalmologist to exclude a recurrence of the inflammatory process in the eyeball.
Chorioretinitis: treatment
Treatment of chorioretinitis is carried out exclusively in a hospital setting, under the constant supervision of doctors and with the control of procedures. Therapy includes:
- Hormonal treatment
- Taking antibiotics
- Nonsteroidal anti-inflammatory drugs
- Injection courses (parabulbar, intramuscular, intravenous)
- Treatment of the underlying cause of the disease (for example, AIDS).
Dr. Belikova's eye clinic does not provide inpatient treatment, however, if chorioretinitis is suspected, you will be immediately prescribed treatment and given the necessary recommendations. Establishing an accurate diagnosis, identifying the cause of the disease, the stage of its development are the first and main steps towards recovery.