Why is this necessary?
If you have suffered deep vein thrombosis of the lower or upper extremities, your doctor will most likely prescribe you indirect anticoagulants.
The main drug in this group today, both here and abroad, is warfarin. In our country, another drug of this group is used quite widely - phenylin. Other coumarin drugs (acenocoumarol, marcumar, marivan) can be used. The recommendations given are mostly applicable to any anticoagulant. The purpose of this medication is to prevent blood clots from recurring, which could cause your condition to worsen or cause life-threatening complications. The risk of recurrence of thrombosis is quite high during the first year after the first episode of the disease, therefore, taking into account various factors, warfarin is prescribed for a period of 2 to 12 months. In rare cases, longer therapy is performed. Indirect anticoagulants have no effect on an already formed blood clot.
To determine the duration of treatment, special (including genetic) blood tests are sometimes required to identify an increased tendency to blood clots.
A very large number of patients around the world receive the treatment you have prescribed. It is used not only in phlebology, but also in such areas of medicine as vascular surgery. In addition to deep vein thrombosis, the basis for prescribing anticoagulant therapy is often previous heart attacks, cardiac arrhythmias, valve and peripheral vessel replacement, and much more.
Warfarin or Aspirin Cardio – which is better?
Manufacturer: Bayer, Germany
Release form: film-coated tablets
Active ingredient: Acetylsalicylic acid
Synonyms: Thrombo ACC, Thrombopol, CardiASK, ASC Cardio
Warfarin analogue Aspirin Cardio is an original German drug that has an antiplatelet effect by blocking the enzyme cyclooxygenase-1, and thus preventing platelet aggregation.
The analogue of Aspirin Cardio is used mainly for prophylactic purposes to prevent cerebrovascular accidents, stroke, acute myocardial infarction, and complications after vascular surgery.
One of the indications for the use of the Aspirin Cardio analogue is stable and unstable angina.
The active ingredient Acetylsalicylic acid in doses of 500 mg has an analgesic, antipyretic and anti-inflammatory effect.
How to monitor treatment
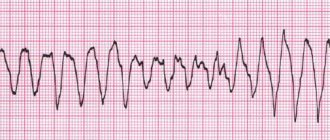
Carrying out antithrombotic (anticoagulant) therapy can save your life and health, but requires increased attention and mandatory compliance with the doctor’s recommendations. Warfarin is a drug that reduces the ability of blood to clot, so its excess can lead to hemorrhagic complications, i.e. to bleeding. To avoid complications, the required dose of warfarin is monitored using a blood test called INR (International Normalized Ratio). This may sometimes be referred to as INR in laboratory responses. During the entire period of taking warfarin, the INR should be in the range of 2.0 - 3.0. If the INR is less than 2.0, then blood clotting is not reduced and thrombotic complications are possible. If the INR is more than 4.0, hemorrhagic complications are very real. An increase in INR from 2.5 to 4.0 indicates the need to reduce the dose of the drug, but usually does not pose a direct threat. For some diseases, the required upper limit of INR is 4.0 - 4.4.
In the absence of the ability to determine INR, monitoring by prothrombin time (PT) is acceptable, but this method is much less reliable. No other blood tests are needed to calculate your warfarin dose. To identify the side effects of the drug, a general blood test, urine test and some biochemical tests are periodically prescribed.
Warfarin or Phenilin
, Ukraine
Release form: tablets
Active ingredient: Phenindione
Warfarin analog Phenilin is an indirect anticoagulant that blocks the enzyme K-vitamin reductase. It is used for the treatment and prevention of thrombosis and embolism, for prosthetic heart valves.
Doses are selected based on laboratory tests.
The disadvantage of the Phenilin analogue is the requirement for constant monitoring of not only prothrombin time and INR, but also regular analysis of coagulograms, thromboelastograms and platelet counts.
How to take the drug
Warfarin is available in 2.5 milligram tablets. Most often, the “starting” and “maintenance” doses of the drug are 5 milligrams (2 tablets) per day. In many cases, for more “fine” adjustments, you will change the dose of the medicine that you take not per day, but per week. This may require either dividing the tablet in half or taking different numbers of tablets on different days. To make it easier to monitor your treatment, you may be given a special account book, or you can keep a notebook with a treatment diary, where it is useful to note the doses of warfarin, INR level, and other laboratory data.
Warfarin is taken in the entire daily dose at one time, preferably at 17:00 - 19:00. Take the tablets with water. It is not recommended to take it with food, but can be taken on an empty stomach. Phenyline is usually taken in 2 doses.
Answers on questions
How to replace Warfarin for atrial fibrillation
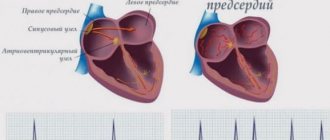
With atrial fibrillation or atrial fibrillation, the risk of blood clots increases; to prevent this phenomenon, Warfarin analogues and substitutes are prescribed - direct or indirect anticoagulants.
When is it better to take Warfarin - morning or evening?
The time of day does not matter when taking Warfarin. It is important to take regularly, at the same time.
Warfarin - direct or indirect anticoagulant
The drug belongs to the group of indirect anticoagulants, since it does not act directly on thrombin, but as a vitamin K antagonist.
Warfarin dose selection
The most difficult and responsible stage. “Loading” initial doses of warfarin (more than 5 mg) are not recommended.
Dose selection can be carried out both with and without the use of low molecular weight heparins (Fraxiparine, Clexane), both in the hospital and on an outpatient basis. The selection period on average takes from 1 to 2 weeks, but in some cases it increases to 2 months. At this time, you will need frequent INR determinations, up to 2 - 3 times a week or daily. Each time, after receiving the next test result, your doctor will determine a change in the dose of the medication and the date of the next test.
If in several tests in a row the INR remains in the range of 2.0 - 2.5, this means that the dose of warfarin has been adjusted. Further monitoring of treatment will be much easier.
Warfarin or Thrombo ACC – which is better?
Manufacturer: Lannacher, Austria
Release form: film-coated tablets
Active ingredient: Acetylsalicylic acid
Synonyms: Aspirin Cardio, Thrombopol, CardiASK
To thin the blood, Warfarin can be replaced with the Austrian drug Trombo ACC, which contains acetylsalicylic acid in 50 and 100 mg doses. In these tiny doses it has antiplatelet properties.
An analogue of Thrombo ACC can be freely purchased without a doctor’s prescription and taken 1 tablet daily for the prevention of heart attack, stroke, and other diseases accompanied by increased thrombus formation.
An analogue of Thrombo ACC is also prescribed after vascular surgery.
To prevent the negative effects of acid on the stomach, Trombo ACC tablets are coated with a special enteric coating. Therefore, they should not be chewed or divided in half.
Monitoring the dose of warfarin
If the dose of the drug is selected, less frequent monitoring is sufficient - first once every 2 weeks, then once a month. The frequency of additional studies is determined separately. The need for an extraordinary determination of the INR may arise in a number of cases, which we will discuss below. If in any doubt, ask your doctor for advice.
Currently, there are portable devices for self-determination of INR (similar to systems for monitoring blood sugar levels in patients with diabetes), but their cost is very high and, in most cases of deep vein thrombosis, purchasing them is impractical.
What may affect treatment
- Any concomitant diseases (including “colds” or exacerbation of chronic diseases)
- The use of drugs that affect the blood coagulation system. This is especially true for a large class of drugs that includes aspirin. It also includes many drugs prescribed as anti-inflammatory and painkillers (diclofenac, ibuprofen, ketoprofen, etc.). As a mild analgesic during treatment with warfarin, it is better to use paracetamol in normal dosages. In any case, the need for a new medication and the duration of its use must be agreed with the attending physician. When warfarin and aspirin are prescribed simultaneously, the INR is maintained in the range of 2.0 - 2.5.
- The use of drugs that affect the absorption, excretion and metabolism of warfarin. Most often, it is necessary to take into account the prescription of broad-spectrum antibiotics and oral antidiabetic agents. However, taking any new medicine may change how warfarin works. If concomitant treatment is necessary, additional INR analysis is usually prescribed at the beginning and end of therapy.
- Diet changes.
Warfarin acts on blood clotting through vitamin K, which is found in varying amounts in food.
There is no need to avoid foods high in vitamin K! Nutrition should be complete. You just need to make sure that there is no significant change in their proportion in the diet, for example, depending on the season. If you significantly increase your intake of foods rich in vitamin K while on a stable dose of warfarin, this may greatly weaken its effect and lead to thromboembolic complications.
The maximum amount of vitamin K (3000 - 6000 mcg/kg) is found in dark green leafy vegetables and herbs (spinach, parsley, green cabbage), and in green tea up to 7000 mcg/kg; intermediate amounts (1000 - 2000 mcg/kg) - in plants with paler leaves (white cabbage, lettuce, broccoli, Brussels sprouts). A significant amount of the vitamin is found in legumes, mayonnaise (due to vegetable oils), and green tea. Fats and oils contain varying amounts of vitamin K (300 - 1000 mcg/kg), more of it in soybean, rapeseed, and olive oils. The content of vitamin K in dairy, meat, bakery products, mushrooms, vegetables and fruits, black tea, coffee is low (no more than 100 mcg/kg). Regular consumption of berries and cranberry juice may increase the effect of warfarin.
Small doses of alcohol with normal liver function do not affect anticoagulant therapy, but alcohol consumption must be treated with caution.
Taking multivitamins that contain vitamin K may reduce the effect of warfarin.
Anticoagulant therapy for atrial fibrillation
Lecture by Doctor of Medical Sciences Alexey Nikolaevich Turov, given as part of the XXX Internet Session.
Oksana Mikhailovna Drapkina, executive director of the Internet Session, secretary of the interdepartmental council on therapy of the Russian Academy of Medical Sciences:
“Now I am pleased to give the floor to our friend, Doctor of Medical Sciences Alexey Nikolaevich Turov.
Alexey Nikolaevich represents the E. N. Meshalkin Research Institute from Novosibirsk. This is not his first performance. We are in direct contact with Novosibirsk.
"Anticoagulant therapy for atrial fibrillation (AF)."
Alexey Nikolaevich Turov, Doctor of Medical Sciences:
— Good morning, dear colleagues.
This post will address a very important issue. We all remember the saying that patients do not die from AF, they die from its complications. When we talk about AF, we constantly associate it with the risk of strokes, which increases by about 5-6 times.
3 million people around the world suffer a stroke related to AF every year. Stroke associated with AF is particularly severe and is associated with a higher incidence of disability.
A stroke that occurs in a patient with AF occurs with more clinical symptoms, more often causes disability and is more likely to be fatal during the first month after the stroke.
I would especially like to emphasize the last phrase. It is absolutely established that the risk of stroke in patients with AF is the same, regardless of its form. Paroxysmal or permanent form - we must protect the patient from stroke in exactly the same way. These patients are at equal risk.
In most cases, the risk of stroke in patients with AF can be prevented with appropriate anticoagulant therapy. The current gold standard is the use of Warfarin.
The largest meta-analysis of 29 studies involving more than 28 thousand patients shows that the use of Warfarin reduces the risk of stroke by 64%. It also reduced mortality from all causes by 24% compared to placebo.
All of the studies presented here demonstrated the superiority of Warfarin over Acetylsalicylicacid in preventing strokes in patients with AF. But Aspirin also reduces the risk of strokes, less significantly than Warfarin, but by 19% compared to placebo.
02:52
We are faced with a question. How to stratify patients. Which patient should I prescribe Warfarin, which patient should I prescribe Aspirin. At present the situation is very clear. Current Recommendations require the use of Aspirin or Warfarin, depending on the presence of risk factors for stroke.
Risk factors. We now have an excellent tool for such stratification. This is the “CHA2DS2 - VASC” scale. The scale is very simple once you understand that each letter on the scale represents a specific risk factor.
The first letter is congestive heart failure. H – arterial hypertension (AH). A – age over 75 years. D – diabetes. S – previous stroke. V – vascular pathology (not only venous, but also arterial pathology). A – atherosclerosis in general. Then age from 65 to 75 years.
For the first time, female gender has become a risk factor for strokes in patients with AF. This is the latest introduction to the Recommendations that were one or two years old.
If we are talking about a patient, an 82-year-old man with hypertension and a history of stroke, then for the share of stroke we get 2 points, for the share of age over 75 years another 2 points. One point for AG. It turns out that this patient has a risk of stroke, which is equal to 5 points. Currently, assessing the risk of stroke is an extremely simple task.
What modern Recommendations tell us about further treatment of the patient depending on the risk of stroke. If a patient scores 0 on this scale, he is not at risk of stroke. This means that he may receive either Aspirin, or (please note) he may not receive anything.
Current Guidelines allow us not to prescribe antithrombotic therapy if the patient has a score of 0 on this scale. If a patient has one point, he can receive either Warfarin or Aspirin, but Warfarin is better. If a patient has a score of 2 or more, he should definitely receive only Warfarin.
Thus, modern Recommendations minimize the role of Aspirin. For the first time, the proportion of patients who may not receive any antithrombotic therapy is increasing. The proportion of patients who should receive Warfarin is significantly increasing. In fact, the presence of even one risk factor is the basis for prescribing Warfarin.
05:55
The benefits of Warfarin vary depending on the risk of stroke. The more points a patient has on the CHA2DS2 - VASC scale, the greater the advantage of Warfarin. On the contrary, if the patient has zero points on the CHA2DS2 - VASC scale, that is, he has no risk, then Warfarin has no benefits.
We now prescribe antithrombotic therapy regardless of the form and severity of atrial fibrillation. We need to be very clear about this at this time. Whether it is a paroxysmal or chronic form, these patients have an absolutely equal risk of thromboembolic complications.
Let's imagine two virtual patients. This is a 63-year-old man who has an ischemic history, suffered a myocardial infarction (MI), coronary artery bypass grafting (CABG), has chronic AF for 7 years, and left atrial dilatation.
A young woman who has a cardiological bouquet - hypertension, diabetes mellitus (DM) and rare attacks of AF. Not so long ago, we would have prescribed Warfarin to a man because he had chronic AF. The woman would be prescribed Aspirin because she is paroxysmal.
What therapy should we prescribe now? A man receives only one point on the “CHA2DS2 - VASC” scale. He does not have congestive heart failure and is old enough (over 65 years) for this to be a risk factor. But he has vascular pathology - MI and vascular surgery. It is due to this that he receives one point. This means he can receive Aspirin.
A woman receives 3 points for female gender, hypertension and diabetes. Thus, she must receive Warfarin. Despite the fact that the woman has rare paroxysms of AF, and the man has chronic AF and dilatation of the left atrium (a rather severe cardiac pathology) and even cardiac surgery.
08:08
Once again, I would like to emphasize that we should prescribe antithrombotic therapy according to risk factors, and not according to the severity of the arrhythmia.
There are two twos in this scale, that is, two factors receive two points on the “CHA2DS2 - VASC” scale. These are age over 75 years and a previous stroke. Patients who have at least one of these factors must necessarily receive Warfarin. These are factors that require the mandatory prescription of Warfarin.
In addition to the CHA2DS2 - VASC scale, arrhythmologists identify two more indications for the use of Warfarin. This is the presence of a thrombus in the left atrial appendage currently or in history and prolonged paroxysms of AF that last more than a day.
In this case, if the patient is in the hospital, and he is already taking Warfarin with a well-selected INR, then he can undergo both drug and electrical cardioversion at any time. That day, the next, within a week.
In this case, nothing limits doctors. There is no need to wait 3-4 weeks for the prescription, saturation with indirect anticoagulants, if this patient was admitted to the hospital while taking Aspirin.
Thus, modern Recommendations leave the palm to Warfarin. According to these Guidelines, most patients with AF should currently receive Warfarin. About a quarter of patients should receive Aspirin.
A quarter of patients with AF may currently receive no treatment unless they have CHA2DS2-VASC risk factors.
According to statistical studies conducted in the last two years, the situation in our country is different. 75% of patients receive various forms of Aspirin. Only 21% of patients receive Warfarin. Unjustifiably low percentage.
10:31
Warfarin is the gold standard of anticoagulant therapy. At the same time, a lot of claims are made against him. In particular, unpredictable response to therapy. Slow development and termination of the effect, which significantly impairs the process of titrating its dose. This is the need for constant monitoring of the anticoagulant effect.
Interaction with many foods, the need to follow a diet. Interaction with many drugs. Resistance to Warfarin is very common. As a result, dosage adjustments are required quite often.
The main complaint is the narrow therapeutic window. We should keep the INR in the range of two to three. If we go below two, we increase the patient's risk. If we raise the INR above three, we increase the patient's risk of intracranial hemorrhage and hemorrhagic stroke.
Warfarin has a fairly narrow therapeutic range. This study analyzed the last seven studies on Warfarin. Only 66% of patients in these studies maintained the correct therapeutic INR range. These are patients who participated in studies, that is, with strict control and constant monitoring.
In routine clinical practice, less than half of patients have correct, adequate INR values. If we talk about Russian reality, no more than 38% of our patients take Warfarin correctly.
Analysis of the study shows that on average, only 51% of the time throughout the study, patients receiving Warfarin were in the correct INR range. Half the time they were in the study, they had abnormal INR values, meaning they were at risk of hemorrhagic or ischemic stroke.
Doctors are reluctant to prescribe Warfarin. It is not prescribed to all patients, but to those who require it according to the risk scale. This is shown by both American and European registers. Only 50% to 65% of patients receive warfarin in the population who should receive it.
13:25
The risk of hemorrhagic complications is of great importance. Many studies (Active and Bafta) show that Warfarin has comparable risks of hemorrhage compared to Aspirin in older people and the Clopidogrel/Aspirin combination.
At the same time, we have a clear bleeding scale “HAS-BLED”. Factors involved include hypertension, liver or kidney failure, previous stroke, history of bleeding, INR instability, age over 65 years, and chronic use of medications or alcohol.
There is one risk score for each of these factors. Thus, the patient can score a maximum of 9 risk points. A value of three or higher is considered a significant risk of bleeding.
Those risk factors that indicate to us the risk of ischemic stroke indirectly increase the risk of bleeding. When we diagnose and predict a high risk of thromboembolic complications in a patient and increase anticoagulant therapy, we thereby increase his risk of hemorrhagic complications. They are usually much more severe than ischemic complications.
Recently, new anticoagulants have appeared. Moreover, those that affect not only the vitamin K antagonist factors, but also directly the tenth and second factors. These are Rivaroxaban, Apixaban, Dabigatran and Ximelagatran.
The greatest interest currently is “Dabigatranetexilate”. This is a new low-molecular-weight direct thrombin inhibitor, which is registered in Russia under the name Pradaxa. This is a prodrug that turns into a medicine already in the human body. It has a short half-life and low bioavailability (only 6.5%).
But at the same time, it has a rapid development of effect and, most importantly, a straightforward pharmacokinetic effect. This means a predictable and stable effect. It is very important that there is low interaction with drugs and low interaction with food.
The greatest joy for our patients is that routine laboratory monitoring of the hemostatic system is not required.
16:22
The RE-LY study opened the red carpet for this drug. It involved a huge number of patients (18 thousand) with AF. They had more than one risk factor for ischemic stroke. Patients who, according to all canons, should have received Warfarin.
At the same time, a third of patients received Warfarin. A third of patients received Dabigatran at a dose of 110 mg twice a day. A third of patients received Dabigatran at a dose of 150 mg twice a day.
Dabigatran at a dose of 150 mg reduced the risk of ischemic stroke and any other systemic embolism by 35% compared to Warfarin.
Subanalysis. Dabigatran at a dose of 110 mg had an advantage over Warfarin only in patients of a very high risk category who had a CHA2DS2 - VASC scale of 3-6 points. Dabigatran at a dose of 150 mg had an advantage over Warfarin, regardless of the risk factors of these patients.
Dabigatran also reduced mortality from cardiovascular complications by 15%. The big finding was that Dabigatran reduced the risk of hemorrhagic stroke by 69% and 74%, respectively, compared with Warfarin.
The risk of major bleeding also decreased, but in relation to Dabigatran 110 mg. The frequency of life-threatening bleeding also decreased by 20% and 33%, respectively.
Thus, Dabigatran at a dose of 150 mg had a more pronounced anticoagulation effect compared to Warfarin and significantly protected the patient from strokes, systemic embolism, and reduced mortality compared to Warfarin. Dabigatran at a dose of 110 mg caused fewer hemorrhagic complications compared to Warfarin.
18:21
Thus, Dabigatran at a dose of 150 mg was more effective than Warfarin. Dabigatran at a dose of 110 mg was safer than Warfarin.
If we talk about secondary endpoints, such as non-hemorrhagic complications, mortality, then the advantage of Dabigatran depended on the stability of INR control.
(Slide show).
The indicator indicated here determines the percentage of the patient being in the correct INR range. If the patient has a well-controlled INR on Warfarin, then Dabigatran has virtually no clinical advantages over Warfarin, except for convenience. This drug does not require INR monitoring.
If a patient’s INR is difficult to control, then as the lability of the indicator increases, the value of Dabigatran and its contribution to mortality and stroke prevention increases. Based on this study, in 2010–2011, Dabigatran was included in the Recommendations for the management of patients with strokes and AF as an alternative to Warfarin.
2011 recommendations from the United American Heart Association. Dabigatran is an effective alternative to Warfarin for the prevention of stroke and systemic thromboembolism.
Let's take a little break from pharmacotherapy. It turns out that we have a systemic anticoagulation effect. We systematically thin the blood in the body only to prevent the formation of blood clots in one small area.
The left atrial appendage is responsible for 95–97% of thrombogenic emboli that enter the cerebral vessels. There have been attempts to locally influence the left atrial appendage and close it, starting with surgical clipping technology.
Currently, the most interesting approach is catheter occlusion of the left atrial appendage. There are two devices. These are the Watchman occluder and the Amplatzer occluder. The ear is occluded and then subjected to sclerosis.
20:57
OccluderWatchman. The procedure is performed in a cath lab under local anesthesia. The size of the occluder is selected depending on the dimensions, which are determined according to transesophageal ultrasound, so that the occluder has the maximum occluding effect of the ear.
After occlusion, after a few weeks, epithelialization of the occluder occurs on both sides. The ear is then filled with blood clots, organized and sclerosed.
Several studies have been devoted to auricular occluders. The largest study, Protect, involved patients with AF. They had more than one point on the “CHA2DS2 - VASC” scale. Auricular occluders were compared with the gold standard, that is, Warfarin.
Patients in the control group constantly received Warfarin. After installation of ear occluders, patients stopped taking Warfarin after 40 days and switched to Clopidogrel. After 180 days, anticoagulation therapy was completely abandoned.
As a result, implantation of auricular occluders reduced the risk of primary outcomes (stroke, all-cause mortality and systemic embolism) by 38% compared to taking warfarin (compared to the gold standard).
Mortality from all causes decreased by 19% compared with Warfarin. The risk of all strokes (both ischemic and hemorrhagic) decreased by 29%. There were a large number of hemorrhagic strokes in the Warfarin group.
If we look at the “curves” of complications, we will see that at the beginning there were significantly more complications in the occluder group. The greatest number of complications occurred on the first day of the study, that is, on the day of surgery.
However, with further observation, after several years, the number of complications equalized and became comparable, reliably indistinguishable. In the occluder group, the risk of complications did not increase, but in the Warfarin group, there was an accumulation of hemorrhagic complications.
23:18
Thus, the ear occluder can be completely considered as an alternative to Warfarin. The indications are the ineffectiveness of the use of Warfarin. Complications from taking Warfarin. The risk of bleeding with the use of Warfarin, especially in elderly and senile patients.
Inability to choose the right dose. Inability to consistently maintain INR. Organizational difficulties in controlling INR, which is especially important for patients in remote areas of our country. Refusal of patients (especially young ones) from lifelong use of this rather aggressive toxic drug.
As a result, approximately 15% of AFs can be assessed as candidates for auricular occlusion.
These four approaches are currently alternatives to Warfarin. Watchman occluders are the technology of the future. This requires budget funding. Apixaban has not yet been registered in Russia.
Dabigatran is the first drug that has shown an advantage over Warfarin. Following this, Apixaban showed an advantage in the Aristotle study. "Rivaroxaban" - in the "Rocket-AF" study.
Why don't we prescribe these drugs everywhere? The problem is mainly financial. If we understand that the majority of patients in need are elderly and senile patients, then it becomes clear to us that these patients will continue to take older drugs.
The problem is that these drugs still require clinical testing. They are just beginning to enter clinical practice. Despite encouraging research data, after Dabigatran was registered worldwide, 505 episodes of major bleeding were reported in the first quarter of 2011.
Over time, clinical practice will put these drugs in their place.
EHRS expert forecast for 2020. Experts believe that in 8 years the leading positions will be occupied by alternative drugs to Warfarin. In particular, Dabigatran and other drugs.
11% of patients will need to receive ear occluders. About the same amount as Warfarin will receive. 16% of patients will continue to take Aspirin. 22% of patients will not require any antithrombotic therapy.
Thank you for your attention.
It is important
Always tell any health care professional you see that you are taking anticoagulants. It is advisable to carry your “account” book or treatment diary with you.
Most dental procedures (except tooth extraction) can be performed without changing your treatment regimen. When removing a tooth, it is usually sufficient to use a tampon with a local hemostatic agent (aminocaproic acid, thrombin sponge).
If you have problems with blood pressure, you need to regularly monitor it and maintain it at a level not higher than 130/80 mmHg.
Warfarin and pregnancy
During pregnancy, taking warfarin is contraindicated. In the event of pregnancy, indirect anticoagulants are immediately discontinued; if further prevention of thrombosis is necessary, heparins are usually used. Therefore, if you suspect pregnancy, refrain from taking the drug until you consult your doctor.
It is possible to use warfarin during breastfeeding. Warfarin is excreted in breast milk in extremely small quantities and does not affect the baby's blood clotting processes, but for complete safety it is recommended to refrain from breastfeeding during the first three days of the mother's treatment with the drug.
pharmachologic effect
Manufacturer: Ozone, Canon Pharma, Russia/Takeda, Denmark
Release form: tablets
Active ingredient: Warfarin
Synonyms: Warfarex, Warfarin Nycomed
Warfarin has an anticoagulant effect due to blocking the synthesis of blood coagulation factors dependent on vitamin K, reducing their content in the blood and slowing down coagulation.
The onset of action usually occurs on the second day of administration, the maximum effect occurs after about a week. After discontinuation of the vitamin-K medication, dependent factors are restored on average within five days.