The term “Coronary heart disease” includes a group of diseases:
- myocardial infarction
- atherosclerotic cardiosclerosis
- angina pectoris.
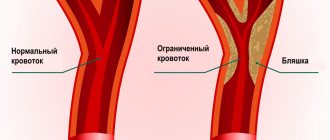
Angina pectoris (synonymous with angina pectoris) is characterized by attacks of sharp chest pain and discomfort in the chest due to lack of blood supply to a certain area of the heart. The severity of the attacks varies, and in rare cases it ends in death. The main cause of the disease is atherosclerosis of the coronary arteries of the heart.
To make an accurate diagnosis, a number of other diseases that may manifest as pain in the heart area should be excluded: spinal osteochondrosis, herpes zoster, diseases of the esophagus and stomach, lung diseases, cardioneurosis, pericarditis.
Types of angina
There are the following types of disease, which depend on the clinical picture:
Angina pectoris
One of the main manifestations of IHD. As a result of a discrepancy between the myocardial need for oxygen and its delivery through arteries narrowed due to atherosclerosis, myocardial ischemia occurs, which is manifested by chest pain or shortness of breath and severe fatigue during exercise.
Stable exertional angina is divided into four functional classes. Functional classes of angina are designed for accurate diagnosis and include a wide variety of clinical information (eg, easy walking on level ground and brisk climbing of stairs).
Variant (spontaneous) angina
Characterized by unpredictable appearance, i.e. pain may also occur at rest. It does not occur as a response of the heart to emotional and physical stress and differs from angina pectoris in that it is usually based on spasm of the coronary arteries of the heart, and not just atherosclerotic damage.
Unstable angina
Requires immediate hospitalization, there is a high probability of developing myocardial infarction.
Types of pain in the heart area
Depending on the specific cause, the patient is bothered by pain in the heart area of various types. They can be isolated, but are more often accompanied by other symptoms that also need to be paid attention to. Based on the type of pain and its location, duration and accompanying complaints, one or another pathology can be suspected.
- Acute coronary syndrome occurs as a result of sudden blockage of a coronary artery (or its branch). This blockage causes unstable angina or the development of myocardial infarction, depending on the location and extent of the blockage. People with acute coronary syndrome usually experience pressure or sharp chest pain, shortness of breath, and fatigue.
- Aortic dissection. Over time, uncontrolled high blood pressure can weaken the wall of the heart's main artery (aorta). It will thin until it eventually ruptures, causing aortic dissection, which is a medical emergency. Aortic dissection usually causes sudden, severe, sharp pain in the chest, neck, throat, or jaw and often a feeling of pressure in the chest that radiates backwards.
- Heart valve damage. The heart has four chambers. The upper and lower chambers are connected by valves with gates that open and close to allow blood to flow in only one direction. If the valves are affected, the flaps become hardened, fused, or leak and do not function properly. The consequences of these valve problems can cause chest pain in the heart area.
- Myocarditis and pericarditis. Chest pain can also be caused by irritation and swelling of the heart (myocarditis) or its outer lining (pericarditis). Inflammation can be caused by infection or as a consequence of a heart attack or heart surgery. Pain from myocarditis or pericarditis is usually sharp, burning and localized in the center of the chest, in the sternum. Typical pain in the heart area when inhaling, against a background of coughing, or when moving. Sometimes it decreases if the patient sits or leans forward.
- Hypertrophic cardiomyopathy (HCM). This is a thickening of part of the heart. When a person has this condition, the heart has to work harder to pump blood in and out of the heart, which can cause dull or aching pain in the chest. They can intensify with stress.
Symptoms
Main symptoms include:
- acute chest pain radiating from the left (or right) side to the lower jaw, arm, shoulder blade
- shortness of breath
- feeling of suffocation and lack of air
- feeling of fear, anxiety
- increased pain in the left chest area when trying to take a deep breath
- increased sweating
- tachycardia
- deviation of blood pressure from normal (low or high).
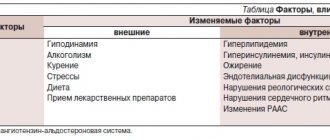
The main factors in the development of the disease that cause symptoms of angina pectoris include
- age (usually after 40 years)
- gender (men develop CHD on average 10 years earlier than women)
- hereditary factor.
An important role in the formation of the disease is played by excess body weight, a history of diseases such as diabetes, arterial hypertension, increased blood clotting, metabolic syndrome, emotional lability, lack of physical activity, smoking and alcoholism.
Short-term attacks of compression (squeezing) in the chest or behind the sternum
Igor, Vologda
October 6, 2020
Good evening dear doctors! Tell. Two months ago I was renovating a children's room, the work had to do with the ceiling. After finishing the work, after some time, I sat down to have dinner and began to experience short-term attacks of compression (squeezing) in the chest or behind the sternum. The attacks were distinguished by their short duration. That is, he squeezed (squeezed), held for 10 seconds and released. At the same time, at the moment of compression, I felt that it was difficult to breathe. Then, after 5 minutes, it squeezed again, or after giving up, it held up again for 10 seconds and released. And so 3 or 4 times with intervals of 5-10 minutes. At the same time, my blood pressure rose to 160 over 90 and my pulse increased greatly to 100 beats per minute. Of course, I got scared and walked around the apartment in a panic and called an ambulance. Upon arrival of the ambulance, they did a cardiogram, discovered a non-subjugal block of the right bundle branch and gave me nitroglycerin. But I don’t remember whether he helped me or not. Because on the way to the hospital I still felt uneasy. At the hospital I was given tests and a troponin test 2.5 hours after the attack. Troponin showed a 0.000 indicator. They did an ECG again, then the cardiologist said that all the indicators were normal and it was not the heart. Perhaps this is how cervical-thoracic osteochondrosis manifested itself. And they sent me home. Then for two weeks nothing hurt, there were no attacks. And two weeks later, closer to autumn, I began to feel pain in my head and severe pain in my neck. Such attacks as pinching. At the same time, the pressure and pulse jumped accordingly. I have an initial form of cervical osteochondrosis and a developed form of thoracic osteochondrosis. Plus scoliosis with tendencies towards kyphosis. I had these symptoms for a month, the neurologist prescribed me anti-inflammatory drugs and all the necessary medications, and it seemed to feel better. But from time to time there is pain in the chest in the middle, and when changing movements the pain intensifies. Also on the back side of the spine, it’s as if a stake has been driven in. But there is no pressure anymore. But with pain, the pulse increases. Also, migiprisiupy with breathlessness are rare and now but very short-lived. A second or two. At the same time, I now feel pain in the back of the thoracic spine. Previously, before the attack, I also had such feelings of constriction and not being able to breathe, but not pronounced. Squeeze 3-5 seconds once and release. In such cases, sweat pressure had not previously risen, but the pulse did rise. These sensations especially manifest themselves when I sit in one position for a long time. But now I have developed a real panic, maybe this attack was related to the heart? Or maybe angina? I don’t know what to do anymore, I’ve had everything examined. Depression is already developing under the pressed topic. I also read a lot on the Internet. Everything looks like angina pectoris there. ECG and echocardiogram are almost normal. There is a tendency to hypertrophy of the false. But with my height 187 and weight 110 they said this is the norm. There is a slight prolapse of the microcircuit with 0-1 registration. Tell me what is happening to me?
The question is closed
pressure
dear doctor
feelings of compression
Diagnostics
In diagnosing angina, a balanced and competent approach is necessary, because with unstable angina, the patient's condition may worsen until the development of myocardial infarction. Each study must be substantiated.
- ECG
- 24-hour ECG monitoring
- bicycle ergometry or treadmill (stress test with simultaneous ECG recording)
- EchoCG
- stress echocardiography
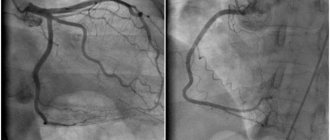
- coronary angiography
- myocardial scintigraphy
At the EXPERT Clinic, cardiologists are also functional diagnostics doctors. They will weigh all the risks before conducting the examination.
Why does my heart hurt at night?
The connection between physical activity and an attack of angina is obvious. In response to the load, the pulse becomes faster, the heart vessels contract and the heart receives less blood, and with it oxygen, which is signaled by the appearance of squeezing and pressing pain in the chest. It is logical to assume that in a calm state, the delivery of oxygen to the heart muscle does not cause problems. Why then does “angina pectoris” come to lovers of passive recreation? Let's figure out what worries the heart in a dream.
An atypical type of angina was first noticed by American cardiologist Myron Prinzmetal in 1959. He described attacks of compressive chest pain at rest that caused temporary changes in the ECG, and called it “variant.” Later, the term was changed more than once: into Prinzmetal’s angina, angiospastic (from the Greek “angeion” - vessel), spontaneous (sudden), resting angina. Prinzmetal named the provocateur of the attack as a spasm (narrowing) of the large cardiac arteries, causing prolonged and intense pain in the chest. The attacks more often occurred at night or early in the morning and were accompanied by increased heart rate, arrhythmia, a drop in blood pressure, and even fainting.
Causes of night "noose"
The culprit of an unexpected spasm is often (not always!) atherosclerosis. In line to get the disease at a young age are heavy smokers, “malicious” untreated hypertensive patients, those with stomach ulcers, cholecystitis and even allergies. The connection between such different diseases is logical, given that they all disrupt the functioning of the autonomic nervous system, which is responsible for the constriction and dilation of blood vessels. Sometimes attacks of atypical angina occur from hypothermia or at the peak of emotions (release of stress hormones). But the most unpredictable variant of the course of the disease is the appearance of an attack for no reason.
Roller coaster that threatens lives
The differences between atypical angina and typical angina are in the strength, duration of the attack, which occurs at rest, and the accompanying vegetative manifestations (fast pulse, rhythm disturbances, including life-threatening ones, increased sweating, a feeling of trembling in the body). The time period when the attack occurs is also important. As a rule, the disease chooses the night-time hours, when the peak activity of the autonomic nervous system (and with it the unexpected surge of adrenaline) is maximum. During this period, the vessels are as relaxed as possible, which makes it difficult for them to adequately resist adrenaline.
What all attacks of atypical angina have in common is a sudden onset. The pain is most often pressing, cutting or burning, lasting 5-15 minutes (sometimes up to 30 minutes). Sometimes the attacks are serial in nature, occurring every 2-15 minutes. Outside of these attacks there may be no complaints at all. At the peak of chest pain, the adrenaline surge is similar in sensations to riding a roller coaster: the skin turns pale, becomes covered with sweat, the pulse quickens, headaches, nausea, and severe weakness occur as a result of changes in blood pressure (from 100/60 to 200/110 mm Hg! ). A rapid drop in pressure can result in fainting.
Rhythm disturbances often complement the pain syndrome at the time of an attack. In the best case, these are extrasystoles (and ventricular ones) or blockades of cardiac impulse conduction, in the worst case, life-threatening ventricular tachycardia or ventricular flutter. The latter, like an extensive myocardial infarction (a sharp vascular spasm completely blocks the access of blood and oxygen to the heart), complicated by a cardiac aneurysm, are fraught with sudden death.
The likelihood of complications developing is frightening in its unpredictability. An increase in the frequency and duration of attacks always worsens the prognosis. Damage to the heart vessels by atherosclerosis adds fuel to the fire, increasing the likelihood of sudden death to 25% per year. Clean heart vessels reduce this risk to 0.5% per year.
How to prove that angina is atypical
The main diagnostic sign of Prinzmetal's angina is changes in the ECG during a painful attack, which indicate ischemia of the heart muscle. As soon as the pain goes away, the tape shows the full normal. Alas, catching such changes on a standard ECG means sitting at the bedside of such a patient and painstakingly guarding his sleep. It is much easier to prove that the cause of the attack is a narrowing of the vessel, using Holter monitoring using an ECG (transient episodes of ischemia at night) or at the time of special provocative tests that cause a sharp narrowing of the heart vessels. But the “gold standard” of classical angina and its complications - stress tests (bicycle ergometry, treadmill test) and coronary angiography, on the contrary, will not detect serious disorders.
How to help a spasmodic vessel during an attack
Since pain when the lumen of a vessel narrows is always intense and long-lasting, the first step is to call an ambulance.
When providing emergency care to such a patient, one should not forget about the high risk of developing myocardial infarction:
- provide the patient with rest (optionally, sit him up in bed) and access to fresh air,
- take nitroglycerin under the tongue (tablets or capsules 0.5 mg; spray 10 g),
- Chew aspirin (not enteric form) or acetylsalicylic acid (0.5 mg tablets).
A specific drug for relieving vascular spasm is nifedipine 10 mg, taken sublingually. True, it should be taken with caution due to side effects (redness of the face, neck, increased heart rate, rhythm disturbances), so it would be better to ask a doctor about it.
Finally, a light massage of the face, back of the head, neck, shoulders, left half of the chest and knee joints will help to relieve the tension from the raging vegetative storm.
How to prevent vascular spasm in the future
It is better to treat Prinzmetal's angina in a hospital, and with tablets, and not with a surgeon's knife. To minimize the likelihood of another attack, it is advisable to eliminate the factors that provoke it: quit smoking and alcohol, normalize sleep, work and rest patterns, deal with “bad” cholesterol, engage in cardio training and, of course, take pills. The latter also dilate blood vessels, especially at night. These include the so-called calcium antagonists - amlodipine, cardillopine, norvasc, kalchek), verapamil or diltiazem. The first of them are best taken at night, the second - in the first half of the day or 2 times.
To ensure proper rest for the heart vessels, beta blockers are added to amlodipine.
Atypical angina definitely sets such a patient apart from the crowd of typical or “classic” ones. Alas, one fact remains unchanged - the risk of developing myocardial infarction. We should not forget that in an effort to save the heart from death, even non-standard approaches are sometimes acceptable.
Author: cardiologist at the clinic
Irina Lutik
Treatment
The goals of treatment are to improve the prognosis (prevent heart attack) and eliminate symptoms of the disease. Non-medicinal (sports, diet), medicinal (tablets and drip infusions) and surgical treatment methods are used.
At the EXPERT Clinic, patients have the opportunity to receive a full consultation with a cardiologist on lifestyle changes and modification of risk factors. If necessary, treatment in a day hospital under the supervision of experienced medical personnel is possible.
Recommendations
To prevent angina attacks you must:
- quit smoking
- control cholesterol levels, if necessary, eat a low-fat diet
- perform a dosed and doctor-selected set of physical exercises
- avoid stress
- lead a healthy lifestyle
A balanced diet, dosed physical activity and regular monitoring by a qualified doctor can save a patient with angina pectoris from heart surgery.
FAQ
How to avoid angina pectoris?
To avoid angina pectoris, it is necessary to prevent the development of atherosclerosis if possible, because in the vast majority of cases it is the cause of angina. As is known, many factors directly influence the formation of atherosclerotic plaques. Gender, age, heredity are predisposing factors that cannot be changed, but other factors can be controlled and even prevented:
- high blood pressure
- smoking
- high cholesterol
- overweight
- diabetes
- low physical activity
- stress
Changing these factors is in your hands!
Is it possible to completely recover from angina?
Angina pectoris, as a rule, occurs as a result of damage to the coronary arteries supplying blood to the myocardium by atherosclerosis, and this is a chronic incurable process. However, with a properly selected treatment regimen, it is possible to ensure that long-term remission occurs and angina attacks will not bother you. Also, at present, if necessary, it is possible to install a stent into the narrowed lumen of the vessel to restore blood circulation, or MCS/CABG surgery is a surgical intervention that restores the blood flow of the heart below the site of the narrowing of the vessel. In this surgical procedure, another path for blood flow is created around the narrowing site to the part of the heart that is not supplied with blood.
Where does it hurt during an angina attack?
Characteristic of angina is paroxysmal pain behind the sternum, in the center of the chest. The pain is of a compressive, pressing nature, more often associated with physical or psycho-emotional stress and goes away when it stops. The pain may radiate to the left arm, shoulder blade, lower jaw and collarbone. If nitrates are used, the effect on angina is not delayed, it develops immediately, within 1-2 minutes.
Are there ways to cope with an angina attack without medications?
Since many people experience angina attacks during physical activity, sometimes simply stopping the activity (walking, etc.) and resting can lead to the cessation of pain. However, people suffering from angina pectoris should always have nitroglycerin or nitrospray with them in order to relieve an attack of pain within one to two minutes. You should not delay the time before taking nitroglycerin, since pain is a manifestation of myocardial ischemia (insufficient blood supply), and if it persists, then foci of necrosis may occur in the myocardium (myocardial cells may die). If angina attacks become more frequent, you should urgently consult a cardiologist.
What medications will help with an attack of angina?
An attack of angina must be stopped as soon as possible from the moment of its occurrence, because prolonged ischemia will lead to the development of necrosis, i.e. myocardial infarction. If an attack occurs for the first time in your life, call an ambulance. You can take a nitroglycerin tablet on your own or use a nitro spray under the tongue. The effect will occur within 1-2 minutes and does not last long, 10-15 minutes. It is better to take the drug while sitting or lying down, as a short-term decrease in blood pressure, dizziness, headache, tinnitus may occur - these symptoms are safe and are a consequence of the action of nitroglycerin. If pain returns, you can take nitroglycerin again, because it does not accumulate in the body; multiple doses of the drug are possible during the day (up to 6 tablets per day). If your blood pressure is high, you need to lower it to normal levels.
All patients who have suffered an attack of angina pectoris need to have an ECG performed and a decision by a cardiologist on hospitalization.
Why is it necessary to quit smoking? How does smoking worsen angina?
If you smoke and have angina, the best thing you can do to help your heart is to quit smoking!
Studies have shown that the mortality rate in those patients with angina who quit smoking decreased by 2 times compared to those who continued to smoke. Why? Angina is based on a lack of oxygen in the heart muscle, and smoking increases the level of carbon dioxide in the blood, and it displaces oxygen in the blood. This leads to oxygen starvation of the heart muscle. Smoking also increases blood viscosity. Smoking increases the frequency and aggravation of angina attacks and greatly increases the risk of myocardial infarction. Quitting smoking eliminates the adverse effects of nicotine on the coronary arteries, and angina attacks disappear or become less frequent.
Important: replacing cigarettes with cigars and pipe tobacco, switching to cigarettes with less tar and nicotine do not reduce cardiovascular risk!
Contrary to popular belief, abruptly quitting smoking is not harmful; overcoming this bad habit has an undeniable positive effect, regardless of smoking experience.
You need to be prepared for the fact that sometimes depression and irritability occur when quitting smoking, in which case you can seek help from a psychotherapist.
I suffer from angina pectoris, but I dream of losing excess weight. What physical activities are acceptable for people with such problems?
For people suffering from angina, 30–45 minutes of physical activity per day is recommended. The best choice is walking (preferably at a brisk pace) or Nordic walking with ski poles, cycling, swimming. It is important that the exercises do not cause pain, palpitations, or shortness of breath. When practicing swimming or water aerobics, you should remember that cold water can provoke angina attacks, so the water temperature in the pool should be comfortable for you. It is better to do water aerobics under the supervision of a trainer and according to a program specially adapted for people with cardiac problems. In this case, the loads should increase very gradually. However, to lose weight, you need not only physical activity, but also proper nutrition; a nutritionist will help you choose the right menu during your consultation.
Can you have angina if there is no pain?
Unfortunately yes. For example, with diabetes mellitus, diabetic polyneuropathy develops, and the patient may not feel pain, this is the so-called silent ischemia. This condition is dangerous because the patient does not take action in time, and myocardial infarction will develop. In some cases, shortness of breath during exercise can be considered equivalent to pain, so you can suspect the presence of angina pectoris and come for examination to a cardiologist.
Pressing chest pain due to non-cardiac problems
Other diseases that have nothing to do with the heart can masquerade as cardiovascular pathologies. For example:
- mental disorders;
- osteochondrosis, localized in the cervical or thoracic region;
- thoracic radiculitis;
- intervertebral hernia;
- digestive tract problems;
- pulmonary diseases;
- some skin diseases (herpes zoster);
- inflammation of intercostal cartilaginous tissues (Tietze syndrome);
- hormonal imbalances.
How do cardiac pain differ from non-cardiac pain? Cardiac ailments are accompanied by arrhythmias, white or bluish tint of the skin, shortness of breath, dizziness, fainting, attacks of nausea or vomiting, spreading of pain to the left forearm, back or lower jaw.
Mental disorders
- Depression.
A long-term nervous disorder characterized by apathy, lack of interest in life, indifference to oneself and the people around you. It can be caused by severe emotional shock. Pain in the heart can last for a long time and does not stop even at rest. They can radiate to the left side of the body, moving to the neck and shoulders.
- Vegetovascular dystonia.
One of the signs of the disease is frequent panic attacks. These are sudden and severe attacks of fear and panic, which are often unfounded. Compressive pain in the heart area is complemented by excessive sweating, tachycardia, weakness, chills, rapid breathing, high blood pressure, and tremor of the extremities.
- The presence of various phobias in a person.
Some people are afraid of closed or open spaces, others are afraid to be at heights, in the dark or in society. Cardiophobia is a constant fear of discovering that you have heart disease. Often experiences entail stimulation of the nervous system and pressing pain in the chest area.
- Hypochondria.
This is another type of neurosis in which a person is constantly looking for various diseases and pathologies. He imagines something that is not really there. Pain occurs when experiencing.
- Cardioneurosis.
A condition that can be called false angina. All symptoms are similar. A distinctive feature is difficulties during swallowing movements (as if a lump is stuck in the throat). Cardioneurosis is easily eliminated with sedatives; Nitroglycerin does not help.
Physical illnesses
- Osteochondrosis.
This disease manifests itself as pressing pain between the shoulder blades, which extends to the heart, arms, shoulders, and neck. A tingling sensation is often felt in the skin. Pain appears when a person makes sudden movements with his head or arms. Discomfort is also felt in a long static position. At night the condition may worsen. Read more about how not to confuse osteochondrosis with heart problems here.
- Thoracic radiculitis.
This disease belongs to the peripheral nervous system disorders. The pain is pressing, can be constant or occur in the form of attacks. Localized in the intercostal space, passes to the thoracic region. Painful sensations become stronger with light pressure on the ribs, as well as during sneezing, coughing or movement.
- Intervertebral hernia.
The cartilage between the spinal discs can age and degrade. In this case, pinched nerves occur, which leads to acute, pinching pain in the chest, when it is difficult to inhale and exhale. The symptoms are very similar to angina pectoris. There is muscle weakness, arms and back go numb, and “goosebumps crawl” on the skin. The pain is paroxysmal in nature.
- Digestive tract problems.
When the abdomen is bloated, accumulated gases begin to compress the internal organs. In this case, pressing pain appears in the thoracic region. It is cramping in nature. This symptom is difficult to confuse with a heart sign, since it is accompanied by digestive disorders: heaviness in the stomach, rumbling, heartburn or belching.
- Heartburn.
This symptom can cause discomfort in the heart area. The pain usually occurs while eating, bending or lying down. There are other manifestations: a burning sensation in the chest, belching with a taste of acid.
- Pulmonary diseases.
Pleurisy. Inflammatory process of the pulmonary membranes that line the organ from the inside. Chest pain is pressing, sharp, increases when coughing or taking a deep breath. The pain decreases slightly if you lie on your right side and do not move. In this case, you need to breathe shallowly. In this state, you may feel chills and sweat.
- Pulmonary embolism.
Acute pain occurs, similar to pre-infarction pain. In addition, you may notice blueness or excessive pallor of the face, difficulty breathing, severe weakness that ends in fainting, weak pulse, and hemoptysis. The cause of the pathology is the formation of a blood clot that blocks the movement of blood in the pulmonary arteries.
- Shingles.
The disease is caused by the herpes virus. A rash spreads across the skin, often localized to the ribs. The nerve endings in this place are affected by infection, so a rise in temperature is possible.
- Tietze syndrome.
Inflammation of the cartilage of the intercostal space. This process is accompanied by severe, sudden pain in the chest area, which becomes more intense when pressing on the rib.
Treatment history
Case No. 1
Kirill, 57 years old. Experienced smoker, hypertensive (“working” pressure 150/95 mmHg). Five years ago, according to the patient, he had problems with his heart and blood pressure, was examined, took prescribed medications for six months, then stopped taking them on his own. During the visit to the clinic, attacks of chest pain appeared during physical activity, which went away when the exercise stopped. At the doctor’s appointment, blood pressure is 170/100 mmHg, rapid pulse is 90 beats per minute. The patient was examined - an increase in the level of “bad” cholesterol was detected, ECG and ultrasound of the heart without signs of ischemia, and ischemia was recorded on the 24-hour ECG monitor at the time of significant physical activity, i.e. there is angina pectoris. The patient was given a treatment regimen for angina pectoris, which resulted in normalization of blood pressure and cholesterol levels within 3 months, and a significant increase in exercise tolerance. With the help of a psychotherapist, the patient decided to quit smoking and took up Nordic walking with a gradual increase in loads under the supervision of a cardiologist. Over the past year, angina attacks have not bothered me. It is recommended to continue taking medications and undergo regular preventive examinations.
Thanks to cooperation with doctors and the desire to feel better, the patient was able to change his lifestyle, prevent complications of the disease and prolong his life for many years.
Causes
Extrasystole of the heart can be caused by a number of reasons, which can be divided into two sources.
The first and most basic is diseases of the cardiovascular system. Extrasystole can occur against the background of disturbances in the functioning of the heart, which are accompanied by organic damage to the myocardium. The second block is external:
- pathology of the thyroid gland;
- electrolyte disturbances;
- external influences. For example, being in a stuffy room where there is a lack of oxygen;
- excessive caffeine consumption. This factor causes tachycardia.