Angina pectoris (angina pectoris) is a sharp pain or discomfort in the chest area. The reason for this is a lack of blood supply to certain areas of the heart. Angina pectoris is noted as a leading symptom in coronary heart disease (CHD), which develops due to blockage or narrowing of the blood vessels of the heart. All patients experience approximately the same sensations - pressing or squeezing pain behind the chest, which often radiates to the arm, shoulder, jaw or neck. The pain usually does not last more than 5 minutes and disappears after taking certain medications or relieving tension. However, the duration of the attack is purely individual; some patients experienced pain from 30 seconds to 30 minutes.
What it is
Coronary insufficiency (CI) is a condition in which blood flow through the coronary (coronary) arteries does not meet the energy needs of the heart. In this case, myocardial ischemia occurs - damage to heart cells due to lack of oxygen and nutrients. Ischemia is a local process that occurs in the place of the myocardium (heart muscle) where its nutrition has been disrupted. The process of deterioration of blood flow itself is most often explained by a narrowing of the lumen of the blood-bearing vessel. Globally this can happen for 2 reasons:
- obstruction (blockage) of the artery lumen;
- spasm due to contraction of the vessel walls.
A combination of these reasons is also possible.
In this case, a person cannot notice any changes in his condition until the level of stenosis (narrowing of the lumen of the artery) reaches critical values. Or until the need of the heart for nutrition makes the stenosis significant. When these conditions are met, ischemia develops in the area of the heart muscle—an attack of angina, myocardial infarction, or even sudden cardiac death occurs. Thus, we can say that clinically coronary insufficiency manifests itself in various forms of coronary heart disease (CHD).
According to research, the number of patients with coronary artery disease in Russia exceeds 7.5 million people - this is a very high figure. Moreover, the prevalence among people of retirement age is 16% higher than among people of working age. That is, the incidence of the disease progresses with age. Men get sick earlier and more often than women.
Causes
Coronary insufficiency most often occurs due to obstruction or spasm of the coronary vessels of the heart or their branches. Let's take a closer look at each of these cases, as well as several more rare situations.
The image is a coronary angiography of the heart vessels. Source: Image by Mario Ohibsky from Pixabay
Artery obstruction
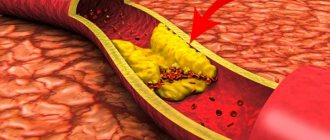
The most important and common cause of coronary insufficiency is atherosclerosis of the coronary arteries. Atherosclerotic plaques protrude into the lumen of the vessel and obstruct blood flow. In this case, chronic coronary insufficiency develops, which most often makes itself felt by attacks of angina pectoris.
Atherosclerotic plaques can also break off or contribute to damage to the inner surface of the vessel and thus provoke thrombosis, which will cause acute coronary insufficiency. Its most common manifestation is myocardial infarction. More information about atherosclerosis can be found here.
Artery spasm
Coronary insufficiency also occurs due to a sharp and prolonged spasm of the coronary arteries. Severe stress, mental and physical overload can lead to this. Often the listed factors complement the existing atherosclerotic lesion of the vessel, which results in angina pectoris or myocardial infarction. However, purely spastic coronary insufficiency is also possible.
Other reasons
There are other, more rare, causes of impaired blood supply to the myocardium:
- Congenital anomalies of the coronary vessels;
- Hypertrophic cardiomyopathy is a condition in which the existing vessels are not enough to meet the needs of the enlarged myocardium (a consequence of hypertension);
- Neoplasms in the chest, compressing blood vessels from the outside (tumor).
Risk factors
Some factors increase the risk of coronary artery disease:
- Male gender and age over 45 years are factors that cannot be adjusted in any way.
- Smoking affects both the development of atherosclerosis and the processes of thrombus formation. Cigarette smoke contains nicotine and carbon monoxide, which have a negative effect on the functioning of the cardiovascular system.
- Low physical activity, a sedentary lifestyle, excess weight and obesity contribute to thrombosis, atherosclerosis, and hypertension, which can lead to coronary insufficiency.
- Eating large amounts of food high in fat and cholesterol contributes to atherosclerosis.
- Chronic stress provokes prolonged spasm of the coronary arteries.
- Heredity - the risk of developing pathology is higher if relatives have it.
Expert advice
The simplest and most effective advice that I give to all patients is to quit smoking. Nicotine causes a sharp vascular spasm, provoking a worsening of the disease. In some cases, eliminating tobacco may be sufficient to minimize symptoms. It is important to understand that the more negative factors simultaneously affecting you, the higher the chance of developing heart spasms. You cannot change your gender and age. However, the basic desire to quit smoking and the initiation of adequate therapy contributes to the complete elimination of the unpleasant symptoms of this disease.
Symptoms
Symptoms of coronary artery disease may vary from case to case. It is also not uncommon for patients to feel nothing strange about their condition until one day, for example, a myocardial infarction occurs.
Among the most characteristic symptoms of coronary insufficiency are:
Angina pain is a pressing, squeezing, burning pain behind the sternum lasting up to 10 minutes. Often appear during physical activity. May begin behind the sternum and then spread to the neck, back, shoulders, arms, jaws;
- Dizziness;
- Cold sweat;
- Pain in the stomach;
- Shortness of breath, especially with exertion;
- Sleep disorders;
- Weakness.
Important! If you notice such symptoms, especially against the background of unusual physical activity, you should immediately call an ambulance. This should also be done if angina has already been diagnosed, but the symptoms are not relieved by nitroglycerin and last longer than 15 minutes.
Source: Pavel Danilyuk: Pexels
The listed symptoms are characteristic of a chronic (reversible) version of coronary insufficiency, which manifests itself as angina pectoris. In the acute (irreversible) version, the described symptoms are more pronounced and last much longer - up to several days (with myocardial infarction). The pain is not relieved by nitroglycerin and can be so severe that it is necessary to resort to narcotic drugs.
Despite the fact that the main symptom of a heart attack is most often severe chest pain (80% of cases), there are other manifestations of the disease:
- Cough and shortness of breath;
- Sharp pain in the upper abdomen;
- Symptoms of brain damage.
An asymptomatic form of myocardial infarction is rare. The area of damage in the heart is not so extensive, and changes are recorded instrumentally after the fact.
Angina symptoms and prognosis
The pathology is characterized by:
- pressing and burning pain in the heart;
- attacks of rapid heartbeat;
- cyclical occurrence of pain syndrome.
Additional signs of pathology include:
- arrhythmia;
- increased blood pressure;
- pale skin;
- fainting.
In some cases, the patient experiences nausea.
All symptoms are not specific. It is important to conduct a complete examination. Only after this the doctor will be able to make an accurate diagnosis.
The prognosis for the pathology depends entirely on its form, the presence of concomitant diseases and the general condition of the patient. It is almost impossible to completely eliminate every symptom. Because of this, patients are registered with a doctor all their lives.
Important!
The disease can cause complications such as:
- severe arrhythmias;
- acute myocardial infarction;
- sudden death.
Chronic form
A typical manifestation of chronic coronary insufficiency is angina. Most often it is caused by atherosclerotic damage to the coronary arteries of the heart, which causes a narrowing of their lumen. During physical activity, the myocardium requires more blood, while the permeability of the artery is reduced - ischemia occurs with characteristic symptoms.
When attacks are predictable and repeated in response to a load of the same severity, they speak of a stable version of angina. Its course is relatively favorable and can be easily controlled. There are other options:
- Unstable angina is a form of angina in which a plaque in a coronary vessel undergoes ulceration, a thrombus gradually grows in the lumen, causing attacks to constantly progress and ultimately lead to myocardial infarction.
- Prinzmetal's angina (vasospastic angina) - occurs as a result of a sudden spasm of the coronary arteries.
We wrote about angina in more detail here.
Until this point, we were talking mostly about absolute coronary insufficiency, when the direct cause of the pathological condition was pathological processes in the coronary vessels. But there is also a relative form that occurs against the background of hypertrophic cardiomyopathy, which was discussed in the causes of coronary insufficiency. During this process, the myocardium increases in size due to the increased load, while new vessels do not appear. In this case, ischemia of poorly supplied areas also develops.
How dangerous is this?
The prognosis for patients with coronary artery spasm is relatively good. The pathology does not cause critical damage to the myocardium, but in the absence of adequate treatment, the risk of developing disturbances in the rhythmic activity of the heart remains. This problem can cause a significant deterioration in the patient’s condition or even death.
Therefore, it is important to consult a doctor in time. Compliance with his recommendations in 90% of cases contributes to the complete elimination of the clinical picture and stabilization of a person’s well-being with a return to normal life.
Sudden coronary death
Sudden coronary death (SCD) is said to occur when a person dies within no more than 6 hours against the background of apparent well-being due to a cardinal malfunction of the heart. At the same time, the patient loses consciousness and falls.
As a rule, the immediate cause of VCS is ventricular tachycardia and ventricular fibrillation. These are severe rhythm disturbances in which the efficiency of myocardial contraction decreases so much that blood does not flow to vital organs in sufficient volume.
WHO recommends at least 150 minutes of physical activity per week to help reduce the risk of VCS. Source: Mario Ohibsky from Pixabay
However, these arrhythmias are most often preceded by a severe attack of acute coronary insufficiency. Extensive myocardial damage as a result of this attack not only in itself reduces the contractility of the ventricles of the heart, but also contributes to the occurrence of arrhythmias.
Sometimes death can be prevented with timely assistance, but this is more typical for sudden cardiac death of an arrhythmogenic nature. In this case, the developing arrhythmia is of paramount importance, and coronary causes are secondary. Patients with diabetes are at increased risk of VCS.
Important! If you see a person suddenly lose consciousness, you should call an ambulance and, if you have the appropriate skills, perform primary resuscitation measures. Cardiopulmonary resuscitation should be resorted to if you do not detect a pulse and/or breathing in the victim.
Despite this threat in patients with coronary insufficiency, with well-chosen treatment and strict adherence to doctor’s orders, the likelihood of VCS becomes significantly lower. It is also important to seek medical help in a timely manner. It is known that several weeks before an attack, patients sometimes complain of pain in the chest, worsening mood, and fatigue. This means that some treatment measures can be taken before an attack occurs.
Causes and symptoms of VSD
Adolescents and women are at risk for developing vegetative-vascular dystonia. In men, VSD rarely occurs as an independent syndrome; dystonia is usually associated with other diseases. The causes of the pathology are most often unknown, but its appearance is associated with the following provoking factors:
- stress – constant nervous tension causes the release of stress hormones, which stimulate the autonomic nervous system;
- hormonal changes - physiologically in women during the menstrual cycle, with the onset of pregnancy, menopause, the concentration of sex steroids changes, which indirectly affect the functioning of the nervous system;
- maturation of the nervous system – in adolescents leads to pronounced signs of VSD;
- bad habits - smoking, drinking alcohol, caffeinated drinks cause disturbances in the functioning of blood vessels and the conduction of nerve impulses.
The first symptoms of vegetative dystonia may appear in childhood. They are associated with heredity and characteristics of pregnancy. If the expectant mother suffers from vegetative-vascular dystonia, smokes, and has been diagnosed with arterial hypertension, then the risk of pathology in the child increases significantly. The health of the baby is negatively affected by intrauterine hypoxia, disruption of feto-placental blood flow, as well as the stress experienced by the pregnant woman. Acute fetal hypoxia during childbirth can also lead to the formation of VSD at an early age.
The formation of vegetative-vascular dystonia in adults can be associated with osteochondrosis, head injuries, and poor nutrition. Prolonged life in poor environmental conditions and work in hazardous industries also leads to VSD. Weather-dependent people also often experience dystonia.
Symptoms of autonomic dysfunction are varied; doctors identify more than 40 signs of the disease, but not all of them occur in one patient. Usually this is a combination of 4-5 constant symptoms and several additional ones. Depending on the manifestations of the cardiovascular system, there are three types of vegetative-vascular dystonia:
- cardiac - not accompanied by pressure surges, it is characterized by pain in the heart area or interruptions in its work;
- hypertensive type - a person suffers from high blood pressure, which is accompanied by panic attacks, chills, and increased physical activity;
- hypotensive type – characterized by low blood pressure, which is maintained at 100/50-90/45 mm Hg. Additional concerns include weakness, drowsiness, and dizziness.
Signs of dystonia include periodic shortness of breath, a feeling of shortness of breath, or a sensation of spasm in the throat. Many people complain to the doctor about pain in the heart, a feeling of increased heartbeat, pressure in the chest, interruptions in the heart, but it is rarely possible to record them using an ECG. Symptoms of autonomic dysfunction include decreased appetite, heartburn, flatulence and other digestive disorders. The disease manifests itself in the form of frequent urination or urinary retention, chills and cold extremities, and increased sweating. Many people complain of weather sensitivity, sleep disturbances, mood swings and irritability. In women with VSD, the menstrual cycle may be disrupted or symptoms of premenstrual syndrome may appear 1-2 weeks before menstruation.
The severity of signs of vegetative-vascular dystonia may vary. Depending on the frequency of symptoms, the following types of disease are distinguished:
- paroxysmal – attacks of vegetative-vascular dystonia periodically appear;
- permanent - the symptoms of dystonia are constant, usually mild, but can intensify under the influence of provoking factors;
- mixed - includes characteristics of the two previous types;
- latent type - signs of the disease appear only after severe stress, the rest of the time the symptoms do not bother.
Vegetative-vascular dystonia, if prolonged without treatment, can lead to disturbances in the functioning of the heart. People who are overweight, eat poorly, and suffer from physical inactivity have an increased risk of developing coronary heart disease and hypertension. In women aged 45-50 years, VSD aggravates the course of menopause.
Diagnostics
Signs of coronary insufficiency can be suspected independently by detecting symptoms of angina pectoris, although an asymptomatic course up to myocardial infarction is not uncommon.
The following diagnostic methods are used in clinical practice:
- Coronary angiography is the gold standard in diagnosing cardiac vascular pathology; it allows one to visualize narrowing of the lumen in the coronary arteries and their obstruction. The technique is invasive - a catheter for administering a contrast agent is placed through the radial or femoral artery, so the study is performed in the operating room under local anesthesia.
- Optical coherence tomography of the coronary arteries is one of the new and accurate methods for visualizing problem areas in the coronary vessels of the heart. The method is also invasive and is performed in a similar manner to coronary angiography.
- Various types of echocardiography (Echo-CG) allow visualization of areas of the myocardium with impaired contractility, as well as many associated disorders.
- Myocardial scintigraphy - allows you to identify areas of the myocardium with impaired blood circulation, for which special radionuclides are used.
- Stress tests (treadmill test, bicycle ergometry) - procedures allow you to evaluate ECG changes indicating myocardial ischemia during physical activity.
Blood samples are also examined, paying attention to:
- Lipidogram - determination of cholesterol and the ratio of lipids in the blood to identify predisposition to coronary artery disease.
- Blood glucose - to exclude diabetes mellitus.
- Determination of the level of red blood cells and hemoglobin - to exclude iron deficiency anemia.
- Biochemical markers - study the levels of various enzymes that may indicate a heart attack.
Important: elevated blood cholesterol levels can significantly increase the risk of atherosclerotic plaques. They can become one of the causes of coronary insufficiency. Cholesterol may be too high due to a high intake of low-density lipoprotein (LDL) and low intake of high-density lipoprotein (HDL). A nutritionist will help you adjust your diet so that there are more “good”, low-density foods than “bad” foods.
Diagnostic methods
To diagnose variant angina, according to modern recommendations and protocols, I use an integrated approach to assessing the patient’s condition. Much in the process of identifying the underlying disease depends on the quality of the first conversation with the patient.
The key features that allow me to diagnose coronary artery spasm are:
- Episodic symptoms that are not associated with physical activity. Patients may suffer from chest pain in the morning, but go to the gym in the afternoon and do a full range of exercises.
- The appearance of discomfort at approximately the same time of day.
- The short duration of the attack, which goes away on its own with further normalization of the person’s condition.
To confirm the appropriate diagnosis, I always additionally prescribe a number of instrumental and laboratory tests.
Instrumental
Traditionally, the first step is to record an ECG. This method allows you to assess the electrical function of the heart, which changes against the background of various forms of coronary artery disease. It is important to note that there may not be any abnormalities on the ECG outside of an attack. This speaks in favor of spasm of the coronary arteries. However, for the reliability of the study, it is necessary to “catch” the patient during the period of pain, which is sometimes extremely difficult, given the night attacks. The film will record ST segment elevation, which is typical of decreased myocardial blood supply.
For the convenience of the patient and to simplify my task, I use Holter monitoring. The technique involves round-the-clock recording of an ECG in a specific patient with further interpretation of the results. With the help of this study, I can easily determine the time of the episode of coronary artery spasm.
Additional Methods
To fully assess the patient’s condition, the following procedures are also used:
- Angiography of cardiac vessels. The essence of the method is to visualize the patient’s coronary arteries on the monitor after introducing a contrast agent into the bloodstream. This allows me to pinpoint the location of the spasm. However, again, you need to “catch” the patient at the moment of the attack.
- Echocardiography. The technique is based on ultrasound examination of the heart. On the screen you can see the cavities of the organ, and I evaluate its functional activity. With Prinzmetal's angina, no special pathological changes occur.
- Test with dosed load. You are asked to exercise on a stationary bike or treadmill in a controlled environment. At this time, an ECG is recorded, pressure is measured and the general condition is assessed. If pain occurs in the heart, the procedure is stopped. However, with variant angina, patients traditionally tolerate the load well.
Based on the results of diagnostic procedures, individual treatment is selected.
Treatment
When prescribing treatment, a cholesterol-lowering diet, moderate regular physical activity and weight loss are first recommended. If you have bad habits, you need to get rid of them. This is called lifestyle modification. Do not underestimate the benefits of such recommendations; in this case, they largely determine the success of treatment and the prevention of future complications.
Source: Michal Jarmoluk from Pixabay
Drug treatment
Drug treatment includes several groups of drugs:
- Beta blockers and calcium antagonists - these two groups reduce myocardial oxygen consumption and promote dilation of coronary vessels. These drugs are also effective for common concomitant conditions (hypertension and arrhythmias).
- Statins are drugs that help normalize the lipid profile of the blood. Prevents the growth of atherosclerotic plaques.
- Antiplatelet drugs - reduce the risk of coronary artery thrombosis by preventing blood clotting.
- Nitrates - this group of drugs eliminates the symptoms of angina attacks.
Surgery
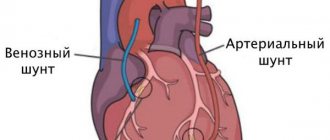
Surgical treatment is resorted to when the level of blood flow disturbance in the coronary arteries becomes critical and cannot be compensated for with medication. In this case, we are talking about two operations: coronary artery bypass grafting (CABG) and coronary artery stenting.
Coronary artery bypass grafting is an open operation in which access to the heart is achieved through opening the chest. The idea is to restore blood flow in the coronary artery after the site of narrowing. This is accomplished by connecting the affected artery and a healthy large vessel through another vessel, forming a kind of “bypass bridge” for the flow of blood. The necessary connecting vessel (shunt) can be taken from the lower leg, forearm and other places.
It is important to know that the rehabilitation period is long due to the long fusion of the sternum. Although the operation is complex, it has been practiced in Russia for a long time and, as a rule, goes well.
Coronary artery stenting is a minimally invasive operation in which a narrowed section of a coronary artery is expanded from the inside using a special metal mesh. The heart is most often accessed through the femoral artery of the leg. This surgical intervention is easy and has virtually no recovery period.
Prevention
Prevention of coronary insufficiency essentially comes down to preventing the development of atherosclerosis and avoiding chronic stress. The importance of preventive measures increases greatly with age. Here's what you can do to significantly reduce the risk of progression and development of severe consequences of the pathology:
- Regular blood tests for lipid levels and cholesterol levels;
- Reducing the consumption of fatty foods;
- Regular moderate physical activity - at least 150 minutes per week;
- Getting rid of bad habits;
- Timely consultation with a doctor if appropriate cardiac symptoms appear;
- Minimizing stressful situations.
Clinical case
A 46-year-old man came to our clinic with complaints of pressing pain in the chest, which arose at rest, mainly at night, and spread to his left arm.
The patient suffers from the problem for 3 months. During the day the symptoms disappear. Exercising in the gym does not aggravate the patient's condition. The disease is associated with stress. The man smokes 1.5 packs of cigarettes per day and suffers from hypertension (160/100 mmHg). ECG at rest without abnormalities. We decided to use Holter monitoring. At three o'clock in the morning an ischemic attack lasting 4 minutes was recorded.
In the morning, when the ECG was re-registered, no pathological changes were detected. Other laboratory and instrumental tests are normal. The patient was diagnosed with IHD. Vasospastic angina, atherosclerosis of the coronary arteries. Arterial hypertension stage II, degree 2, risk. I was prescribed Amlodipine (10 mg orally once a day), Nitroglycerin (1 tablet under the tongue during an attack), Aspirin (75 mg once a day), Rosuvastatin (20 mg per day), lifestyle correction - quitting smoking, minimizing stress. When re-examined 2 weeks later, the patient noted a complete absence of new attacks of chest pain. Feels good, exercise tolerance without restrictions.
I will be glad if this article was useful. Share your experience about episodes of compressive pain in the heart in the comments: how you saved yourself and what helps better. Our experts will help you understand the situation.
Sources
- Coronary Heart Disease - nhlbi.nih.gov.
- Cardiovascular Therapy and Prevention, 2016; 15(2): 93–99 https://dx.doi.org/10.15829/1728-8800-2016-2-93-99.
- Kurdgelia T. M., Kislitsina O. N., Bazarsadaeva T. S. Sudden cardiac death: epidemiology, risk factors and prevention // BMIK. 2014. No. 3.
- Guide to faculty therapy: textbook / S. A. Boldueva, I. V. Arkharov, E. L. Belyaeva, E. G. Bykova, T. V. Ermolova, M. I. Ivanova, I. A. Leonova, A. P. Makhnov, N. S. Shvets, O. Yu. Chizhova; edited by S. A. Boldueva. — 3rd ed., add. and processed - St. Petersburg: Publishing house of North-Western State Medical University named after. I. I. Mechnikova, 2021. - p. 6-32; 64-76.
- Picard F., Sayah N., Spagnoli V., Adjedj J., Varenne O. Vasospastic angina: A literature review of current evidence. //Arch Cardiovasc Dis - 2021 - Vol.112 - No. 1 - p.44-55