Atherosclerosis of the neck vessels is a systemic disease, the cause of which is directly related to the formation of atherosclerotic plaques on the inner surface of the vessels and arteries. This pathology underlies the development of cerebral circulation disorders and the development of its chronic insufficiency.
Atherosclerosis of the carotid arteries and vessels of the cervical spine significantly increases the risk of severe complications, including death. Such complications threaten the patient when he ignores therapeutic measures.
Definition:
Atherosclerosis of the carotid arteries is a disease accompanied by narrowing of the vascular lumen of the carotid arteries. As a result of such processes, the required amount of arterial blood does not reach the brain and tissues of the head. Partial or complete blockage of these vessels can cause a brain stroke, which leads to disability or even death of the patient.
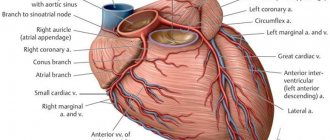
The carotid arteries are paired blood vessels located under the skin on either side of the neck. Normally, healthy carotid arteries are flexible and have a smooth surface. If you place your fingers on the skin under your lower jaw on either side of your Adam's apple, you may feel the carotid arteries pulsate. Your carotid arteries carry oxygen- and nutrient-rich blood to the cerebral cortex and other vital brain structures that control body functions. Neck vasoconstriction occurs when the carotid arteries become blocked by fatty, waxy deposits called plaque. The accumulation of plaque in these arteries leads to disruption of blood supply to the brain and increases the risk of stroke, as with atherosclerosis of the BCA, which we wrote about earlier.
Causes
The carotid arteries become hardened and narrowed over time due to the constant deposition of plaque, which can restrict blood flow. Plaques are composed of a buildup of cholesterol, calcium, fibrous tissue and other cell breakdown products that are deposited at sites of microscopic damage to the arteries and lead to the formation of a blood clot (thrombus). This process is called atherosclerosis.
Factors that contribute to the development of carotid atherosclerosis and increase the risk of plaque formation and disease development include:
- High blood pressure. Excessive pressure on artery walls weakens them and makes them more susceptible to damage.
- Smoking. Nicotine irritates the lining inside the artery, increasing heart rate and blood pressure levels.
- Age. As we age, arteries become less elastic and more susceptible to damage.
- Increased blood fat levels. High levels of low-density lipoprotein (the so-called “bad” cholesterol) and high levels of triglycerides (blood fats) stimulate plaque formation.
- Diabetes. Diabetes affects not only the ability to process glucose properly, but also the ability to process fat efficiently, increasing the risk of high blood pressure and the development of atherosclerosis.
- Obesity. Excess weight contributes to increased blood pressure, the development of atherosclerosis and diabetes.
- Heredity. If you have atherosclerosis or signs of cardiac ischemia in your relatives, your risk of developing these diseases increases.
- Lack of physical activity. Low physical activity contributes to the development of a number of diseases, including hypertension, diabetes and obesity.
When these risk factors combine, it significantly increases your risk of developing the disease. If you have these factors, make an appointment with your doctor. Your doctor will order a test to evaluate the health of your arteries and recommend treatment and lifestyle changes to reduce your risk of stroke.
Symptoms
Because carotid atherosclerosis develops slowly and is often asymptomatic, the first manifestation of this disease may be a stroke or transient ischemic attack (TIA), sometimes called a mini-stroke. TIA causes stenosis of the carotid arteries: they are accompanied by headaches, short-term loss of vision and speech impairment, numbness of half the body and limbs.
A stroke or TIA is a medical emergency. If you or a loved one shows signs or symptoms of a stroke, call emergency medical services immediately. Do not try to get to the hospital on your own. Warning signs and symptoms include:
- Sudden numbness or weakness in the face and limbs, often on only one side of the body
- Loss of ability to move limbs
- Impaired speech and understanding of the meaning of someone else's speech
- Sudden loss of vision in one or both eyes
- Dizziness or loss of balance
- Sudden severe headache without a specific cause
Complications
The most serious complication of carotid atherosclerosis is stroke. The increased risk of stroke in patients with carotid artery disease is due to the following factors:
- Decreased blood flow. Carotid arteries with atherosclerosis often narrow to such an extent that they do not provide sufficient blood flow to the brain.
- Plaque rupture. There is a risk that part of the plaque will break off and penetrate the small arteries of the brain (cerebral arteries). A fragment lodged in one of these small arteries will block it. This will impede blood flow to the area of the brain that is supplied by this artery.
- Thrombosis. Some plaques are prone to cracking and forming an uneven surface on the artery wall. The body reacts to these changes as if it were damaged and sends platelets to this place - blood cells that participate in the process of blood clotting. A blood clot may form that is large enough to block or slow blood flow through the carotid or cerebral artery, causing a stroke.
A stroke causes permanent brain damage and muscle weakness, and in severe cases, death.
Risk factors
- smoking (the most dangerous factor);
- hyperlipoproteinemia (total cholesterol > 5 mmol/l, LDL > 3 mmol/l, Lp(a) > 50 mg/dl);
- arterial hypertension (high blood pressure) (systolic blood pressure > 140 mm Hg; diastolic blood pressure > 90 mm Hg);
- diabetes;
- obesity;
- physical inactivity (sedentary lifestyle).
Without correction of risk factors, in the presence of a predisposition to atherosclerosis, cholesterol deposits gradually increase in the walls of the arteries. For clinical manifestations of atherosclerosis, a narrowing of any large artery by more than 50% is necessary. It is at this stage that patients most often seek medical help. Plaques in the carotid arteries are most often located in the cervical segment of the artery, over a short distance. The key point in determining the severity of damage to the internal carotid artery is the percentage of narrowing (stenosis) of its lumen, in relation to the normal lumen located behind the plaque. Numerous studies have proven that stenosis of the internal carotid artery by more than 70% increases the risk of ischemic stroke by 5 times, compared with a lesser degree of stenosis. The brain receives its main blood supply from two internal carotid and two vertebral arteries. Stenosis of the artery by more than 70% leads to a change in the local parameters of the blood flow - they can be compared with the flow of river water in places where the channel narrows - seething, turbulence, chaotic impacts of blood into the vessel wall lead to microthrombosis, trauma to the vessel wall, destruction of unstable plaques and its detachment particles. Particles of plaques and blood clots freely located in the bloodstream are called emboli. Following the bloodstream, the embolus gets stuck in smaller branches located in the brain, causing ischemia of areas of the brain and leading to its death.
Symptoms of atherosclerotic plaques in the carotid artery
The presence of atherosclerotic plaques in the vessels supplying the brain is often difficult to suspect, because complaints are varied and inconsistent. In addition, for clear symptoms to appear, there must be pronounced narrowing of the arteries. It is necessary to suspect the presence of atherosclerosis of the carotid arteries in the presence of risk factors, as well as diseases of the heart and blood vessels of the lower extremities. Currently, the main symptoms are considered to be the presence of small and large ischemic strokes, as well as general cerebral symptoms.
- Transient ischemic attacks (TIA)
occur when small fragments of an atherosclerotic plaque break off and enter small vessels of the brain, causing brain death in a small area. In this case, transient paralysis of the arms and/or legs (from several minutes to several hours), speech impairment, transient or sudden blindness in one eye, memory loss, dizziness, and fainting are possible. The presence of a TIA is a serious sign of a high risk of developing a severe stroke in the near future and requires immediate medical attention.
- Acute ischemic cerebrovascular accident (ACVA)
– a consequence of acute blockage of a large branch of the internal carotid artery, which led to the death of neurons and loss of some functions in the brain. In a third of all cases, a stroke leads to death. In most all cases, severe disability after a stroke forever changes the life of a person and his relatives.
- Chronic cerebrovascular insufficiency
– a decrease in blood flow to the brain due to narrowing of the arteries, forcing brain cells to be in constant tension of all intracellular systems and intercellular connections. Symptoms are non-specific, they can be noise in the head, dizziness, flashing “spots” before the eyes, unsteadiness when walking, etc.
Surgery to remove plaque from the internal carotid artery (eversion carotid endarterectomy)
Unfortunately, there are no drugs yet that can “dissolve” or eliminate plaques in blood vessels. Modern drugs can only stop the growth of atherosclerotic plaques and reduce the likelihood of blood clots. The main and only effective treatment for narrowing of the arteries is surgery. Numerous studies involving many countries have indisputably proven the effectiveness of preventive surgical methods in preventing stroke. It is important to understand that surgical intervention is performed if there are strict indications for surgery, and does not replace the treatment of systemic atherosclerosis.
One of the ways to eliminate stenosis of the internal carotid artery is the operation of eversion carotid endarterectomy.
- Under the safest anesthesia (usually a local anesthetic), a small incision (4-6 cm) is made in the neck in the area of the carotid artery.
- Under threefold magnification, with the help of special instruments, the arteries are separated from the surrounding structures (nerves, veins).
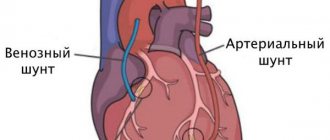
- The resistance of the brain to temporary compression of the carotid artery is checked using several techniques. If there is the slightest suspicion that the brain will not be able to withstand clamping of the carotid artery, a special temporary shunt is installed to ensure blood supply to the area of the operated artery. The arteries are pinched.
- The internal carotid artery is dissected transversely and the outer layer of the artery is everted from the plaque like removing a stocking from a leg, after which the atherosclerotic plaque is removed from the vessel along with the inner layer.
- All plaque remnants freely lying in the lumen of the vessel are carefully removed and the outer layer of the artery is returned to its previous position.
- The integrity of the vessel is restored with a continuous suture. The threads used for sutures are thinner than 1/10 mm and are non-absorbable.
- Once the suture is completed, air is released from the artery and blood flow is restored. After checking the sutures for tightness and the absence of sources of bleeding, the wound is sutured layer-by-layer with a cosmetic suture.
Throughout the operation, the patient remains conscious, and verbal and eye contact is always maintained. The duration of the entire operation is 1-2 hours; in the postoperative period, long-term observation and treatment in the intensive care unit is not required. The perioperative protocol at our institution allows patients to be discharged the next day after surgery, which has a beneficial effect on early rehabilitation and prevents the occurrence of infectious complications.
Diagnostic methods
- Medical checkup. A “whooshing” sound (murmur) above the carotid artery in the neck when auscultated indicates a narrowing of the carotid artery. Your doctor will examine your physical and mental health, such as muscle strength, memory, and speech function. To begin treatment for arterial stenosis, one examination is not enough: instrumental examination methods will help to assess the condition.
- Ultrasonography. A non-invasive method for detecting atherosclerosis of the carotid arteries is Doppler ultrasound. This test evaluates blood flow, pressure, and constriction of a blood vessel by recording high-frequency sound waves (ultrasound) bouncing off red blood cells.
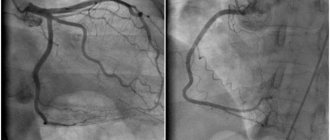
- Computed tomographic angiography (CTA). This imaging test uses a contrast agent to highlight the carotid arteries in the images. A contrast agent is injected into a blood vessel. Once it enters the carotid arteries, a computed tomography (CT) scanner takes X-rays of the neck and brain from different viewing angles.
- Computed tomography (CT) of the head. This imaging method allows you to examine brain tissue without the introduction of contrast agents and exclude the presence of bleeding and other disorders.
- Magnetic resonance angiography (MRA). Like CTA, this imaging test uses a contrast agent (without iodine) to highlight the arteries in the neck and brain. A magnetic field and radio waves are used to create three-dimensional cross-sectional images.
- Magnetic resonance imaging (MRI). This imaging technique looks at brain tissue to help detect early signs of stroke or other problems.
- Angiography of cerebral vessels. This traditional invasive method is rarely used because this examination increases the risk of stroke. As with cardiac angiography, during the procedure a contrast agent is injected using a catheter placed directly into the carotid arteries. Then x-rays are taken.
Our specialists
Zhuravleva Nadezhda Vladimirovna
Head of the center for diagnosis and treatment of myasthenia gravis.
The doctor is a neurologist of the highest category. Physiotherapist. Experience: 16 years.
Derevianko Leonid Sergeevich
Head of the Center for Diagnostics and Treatment of Sleep Disorders.
The doctor is a neurologist of the highest category. Vertebrologist. Somnologist. Epileptologist. Botulinum therapist. Physiotherapist. Experience: 23 years.
Drozdova Lyubov Vladimirovna
The doctor is a neurologist. Vertebroneurologist. Ozone therapist. Physiotherapist. Experience: 17 years.
Bezgina Elena Vladimirovna
The doctor is a neurologist of the highest category. Botulinum therapist. Physiotherapist. Experience: 24 years.
Palagin Maxim Anatolievich
The doctor is a neurologist. Somnologist. Epileptologist. Botulinum therapist. Physiotherapist. Experience: 6 years.
Temina Lyudmila Borisovna
Pediatric neurologist of the highest category. Candidate of Medical Sciences.
Experience: 46 years.
Romanova Tatyana Alexandrovna
Pediatric neurologist. Experience: 24 years.
Mizonov Sergey Vladimirovich
The doctor is a neurologist. Chiropractor. Osteopath. Physiotherapist. Experience: 8 years.
Treatment methods
What treatment methods can reduce the risk of complications due to atherosclerosis of the carotid arteries? In the early stages, drug therapy is effective: for cerebral vascular diseases, medications that reduce blood viscosity and lower cholesterol levels are prescribed. If the vascular lumen is blocked to a significant extent, the solution may be surgical intervention:
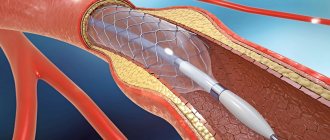
- angioplasty and stenting of the carotid arteries are modern and painless ways to restore the vascular lumen and normalize blood flow in atherosclerosis.
- Carotid endarterectomy is an operation to remove plaque from the carotid artery, performed under anesthesia through a small incision in the neck.
Read more about methods of treating atherosclerosis of the carotid arteries in the following publication.
Surgical prevention of ischemic stroke
When the carotid artery is significantly narrowed by atherosclerotic plaque, carotid endarterectomy is usually used. A surgical operation that involves opening the lumen of the affected carotid artery and removing atherosclerotic plaque from it. This procedure is well established and provides long-term positive results in the form of prevention of ischemic stroke for many years. Carries minimal risk in most patients. The stay in the clinic is usually 24-48 hours.
Most patients experience mild discomfort and are able to return to normal activities after treatment after a short recovery period (7-14 days).
As an alternative to surgical treatment, intravascular (endovascular) technique is used. Balloon angioplasty with stenting. Currently, international studies are evaluating the effectiveness of this technique for the treatment of carotid artery atherosclerosis. This procedure is performed in conjunction with angiography under local anesthesia through a puncture in the groin.
The essence of the procedure is the intravascular placement of a special catheter with a balloon to the site of narrowing of the carotid artery. When the balloon is inflated in the lumen of the carotid artery, the narrowed area is widened. To consolidate the effect, stenting of the dilated carotid artery is performed by installing an internal stent (frame) of the vessel. The recovery period after angioplasty with stenting is also very short.