Causes
The exact percentage of the prevalence of coronary vascular spasm, otherwise known as Prinzmetal's angina, among the population has not yet been established.
This indicates that there are not many patients with a similar diagnosis. However, due to the similarity of the clinical picture with other forms of coronary artery disease, you should always be aware of the possibility of this problem. The occurrence of heart spasms is based on two key factors:
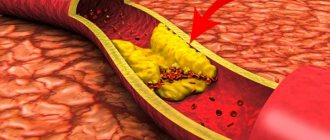
- The presence of atherosclerotic plaques inside the vessel. This appears as accumulations of fatty and inflammatory cells that are deposited in the inner wall of the coronary arteries.
- Spasm. When you are stressed, smoke a lot, or engage in strenuous physical labor, the lumen of the vessels that supply blood to your main “engine” in the body narrows. Given the presence of plaques in the arteries, the supply of oxygen to the muscle fibers of the heart sharply decreases, which provokes the onset of an attack.
These two factors remain key in the development of the disease.
Remember that the spasm rarely lasts longer than 5-10 minutes. This time is not enough for necrosis (infarction, death) of individual muscle fibers to occur, so there is no need to panic. However, a lack of cell nutrition develops with the addition of characteristic symptoms.
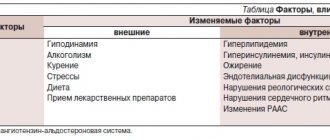
Now I will list the factors that provoke spasm of the heart vessels:
- Age. Traditionally, patients over 45-50 years old suffer from variant angina.
- Floor. Men are more susceptible to various types of IHD.
- Atherosclerotic damage to the blood vessels of the heart and the whole body. The more plaque there is in the arteries (and the thicker it is), the higher the chance of developing typical signs of the disease.
- Smoking. Nicotine is a substance that stimulates arterial spasm throughout the patient’s body. Due to the presence of plaques in the vessels, an attack can occur virtually after every cigarette smoked. It all depends on the severity of the atherosclerotic process.
- Stress. Under the influence of emotional stress, the muscular lining of blood vessels contracts, reducing the delivery of oxygen and nutrients to the heart cells.
How to relieve heart spasms
First of all, it is necessary to make sure that the causes of the pathology lie precisely in the arteries. Heart spasm can be diagnosed by performing a hardware scan. To confirm concerns, you will have to undergo an electrocardiogram (determining the ST interval), daily monitoring or echocardiography.
Bicycle ergometry and laboratory blood samples to identify cardiac troponins and other markers indicating severe myocardial damage would be useful.
Unfortunately, there is no clear answer to the question of how to relieve cardiac muscle spasm. Therapy is selected individually, taking into account the physical characteristics of the patient and the presence of concomitant diseases. People at risk are advised to carry nitroglycerin with them. If pain occurs in the chest area, you should take this drug in the form of a tablet or a diluted alcohol solution. Usually unpleasant symptoms disappear after a few minutes.
Heart spasms can be the first sign of a dangerous vascular disease. If there are irremovable negative factors (bad heredity, age), a cardiologist or arrhythmologist can prescribe preventive treatment. The most commonly prescribed drugs are anti-ischemic drugs, calcium channel blockers, antioxidants, and anti-sclerotic substances.
What to do if heart spasm becomes a symptom of a serious illness? Surgical treatment is recommended when dangerous arterial defects are identified and when pharmacological effects are low.
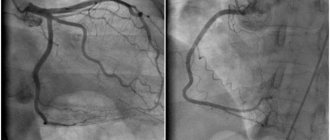
- Angioplasty is an operation using a special catheter that expands the lumen of the ducts.
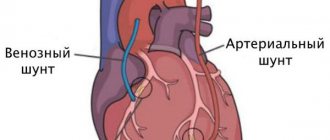
- Coronary bypass surgery is the restoration of blood flow by implanting a “bypass branch” of the circulatory system.
Today, the stenting method is increasingly used. If cardiac spasm occurs due to weakness of the vessel walls, then a special tubular mesh is installed in it, which ensures blood flow.
Symptoms
Some patients I have worked with have believed that symptoms are the same for everyone. That is why I had to explain to them that manifestations can vary depending on the individual characteristics of the body. Of course, a number of general points can still be identified.
The clinical picture of variant angina, the cause of which is precisely a sharp decrease in the diameter of the coronary vessels, is in many ways reminiscent of traditional angina pectoris. Most forms of IHD are similar to each other. My task, as a doctor, remains the differential diagnosis of pathological conditions. The approach to treatment directly depends on this.
Complaints with which people turn to me or another cardiologist for help:
- Pressing pain in the heart area, which can spread to the left arm, neck, jaw. I often hear it compared to a twisting, cramping sensation in the chest. Sometimes patients indicate a burning sensation, which may go away on its own within 5-10 minutes.
- Increased heart rate. Against the background of pain, the heart rate increases. Recently, a woman said that, in addition to chest discomfort, her “heart wanted to jump out of her mouth.” Agree, this is a very eloquent description.
- Dyspnea. A sign that can sometimes be the only clinical manifestation of the pathology.
- Cold sweat. The symptom occurs in severe forms of the disease.
- Nausea, vomiting, confusion are rare but common companions of variant angina.
It will be useful for you to know that variant angina is not associated with physical activity. Most forms of IHD are characterized by an increase in pain during active walking, heavy lifting, and the like. With Prinzmetal's angina, sensations occur spontaneously, often at the same time of day. 55-65% of attacks occur in the early morning hours.
Signs of cardiovascular diseases
There are a number of clinical manifestations that suggest pathology associated with the functioning of the cardiovascular system.
Pain and discomfort in the chest
Pain is the most common symptom indicating a disorder in the normal functioning of the heart. The nature of chest pain varies: from mild squeezing (numbness, burning) to severe acute squeezing.
Angina is characterized by compressive pain in the heart radiating to the arm, neck, and shoulder blade with a gradually increasing amplitude. The attack is provoked by physical activity, emotional stress, and resolves after taking nitrosorbide.
Severe intense chest pain that does not go away after taking nitroglycerin, accompanied by sweating, palpitations and fear of death, may indicate the development of acute myocardial infarction. One of the causes of a heart attack is damage to the coronary arteries by atherosclerosis. The pain of a heart attack can be so sharp that a person may lose consciousness with the development of painful shock: blood pressure drops, pale skin appears, and cold sweat appears.
Excruciating pain in the chest, radiating to the back of the head, back, and sometimes to the groin area, is a symptom indicating an aortic dissection or aneurysm.
A dull aching pain in the heart area without a tendency to radiate, against a background of elevated temperature, of varying intensity: sometimes intensifies, sometimes weakens - indicates inflammation of the heart sac - pericarditis. The pain intensifies with movement, coughing, or pressing on the chest.
Signs of pulmonary embolism depend on the location and size of the clot. A person experiences chest pain that radiates to the jaw, shoulder, neck, and arm. Weakness, tachycardia, cough, shortness of breath occur. Hemoptysis may occur.
A short stabbing or dull pain in the heart area, occurring regardless of physical activity, without disturbance of breathing or heartbeat, is typical for patients suffering from cardiac neurosis. In the clinical picture of neurosis, in addition to cardiovascular disorders, signs appear that indicate a functional disorder of the nervous system: weakness, increased fatigue, absent-mindedness, poor sleep, tremors of the extremities.
Palpitations and a feeling of irregular heartbeat
Rapid heartbeat is not always a sign of heart disease; it can be physiological in nature, for example, after exercise, emotional excitement or after eating a large amount of food.
On the other hand, tachycardia as a symptom appears in the early stages of the disease. When there are heart rhythm disturbances - arrhythmias, a person has a feeling that the heart either “jumps out” of the chest or freezes for a certain period of time.
A disruption of the heart rhythm can occur in the form of a sharp non-simultaneous excitation of different muscle fibers of the myocardium, and this causes the cessation of the orderly contraction of the heart muscle - atrial fibrillation.
Supraventricular tachycardia is characterized by attacks of rapid heartbeat that can last from a few seconds to several days. Prolonged attacks are accompanied by weakness, sweating, fainting, increased intestinal motility, and excessive urination.
Ventricular tachycardia is less common and leads to disruption of the blood supply to organs and heart failure.
With heart block, irregular contractions, loss of individual heart impulses, and a significant slowing of the pulse are observed - bradycardia. Due to a decrease in cardiac output, signs of ischemia develop: drop in pressure, dizziness, fainting.
Dyspnea
A feeling of shortness of breath or shortness of breath occurs with heart failure, when the heart is not able to work at full capacity and does not pump the required amount of blood through the blood vessels. Heart failure can be the result of atherosclerotic vascular disease (deposition of fatty plaques on the inner wall of the arteries), acute myocardial infarction, heart defects, and high blood pressure. In the initial stages, shortness of breath is a concern only after physical exertion; as the pathological process progresses, it appears even at rest.
Severe shortness of breath is accompanied by rapid heartbeat, acrocyanosis - blue discoloration of the skin of the nose, lips, and fingers. The patient cannot lie down, takes a forced position (half-sitting), his legs are cold. With the development of pulmonary edema, a severe cough and foamy sputum mixed with blood appear.
Cardiac dyspnea should be distinguished from shortness of breath of a psychogenic nature (anxiety, fear, panic attacks).
Edema
The appearance of edema is a manifestation of venous stagnation in the systemic circulation. They first appear in the afternoon on the feet and ankles. After a night's sleep, swelling usually subsides.
Further accumulation of fluid in the body leads to the appearance of edema in the hips, lower back and abdominal wall.
As the edematous syndrome progresses, fluid begins to accumulate in the abdominal cavity, and the volume of the abdomen increases. The patient complains of heaviness in the abdomen, especially in the right hypochondrium due to liver stasis and hypertrophy.
If blood circulation in the abdominal cavity is impaired, dyspeptic disorders occur in the form of poor appetite, nausea, vomiting, intestinal spasms, flatulence, and stool disorders (alternating diarrhea with constipation). Kidney function may deteriorate and diuresis may decrease.
In especially severe cases, swelling can spread to the subcutaneous tissue of the chest, arms and face. The hands become numb, and symptoms of paresthesia (crawling sensations) develop.
Change in skin color
Pale skin often accompanies vasospasm, some heart defects (aortic valve insufficiency), and severe forms of rheumatic carditis.
Cyanosis (blueness) of the lips, nose, cheeks, earlobes, fingers of the extremities - the result of prolonged tissue hypoxia is observed in advanced stages of pulmonary heart failure. The cause of cyanosis is darkening of the blood due to slower blood flow and insufficient oxygen saturation of the blood in the pulmonary circulation as a result of stagnation. Dark blood, shining through the skin and giving them a bluish tint.
Headaches and dizziness
These symptoms are often present in diseases associated with damage to the cardiovascular system. The main reason for this reaction of the body is insufficient blood supply to the brain structures. Oxygen deficiency causes hypoxia; in addition, brain cells suffer from intoxication with decay products formed during the metabolic process, which are not taken up by blood from the brain in time.
Jumps in blood pressure can cause headaches or attacks of dizziness. Long-term hypertension causes irreversible structural changes in the myocardium (hypertrophy), in which the heart muscle quickly wears out and cannot cope with its work. Against this background, heart failure develops when the pumping function of the myocardium is disrupted and the blood supply to all organs and systems of the body deteriorates.
Inflammatory diseases of the cardiovascular system
These include: myocarditis, endocarditis, pericarditis.
Myocarditis is inflammation of the muscular lining of the heart. Caused by various infectious agents. Manifested by pain in the heart, shortness of breath, swelling, palpitations, arrhythmias. As complications, it can cause heart failure or vascular thromboembolism.
Endocarditis is inflammation of the inner lining of the heart. The consequence of the inflammatory process is the formation of heart defects. Symptoms are determined by the type and stage of the disease.
Pericarditis is damage to the outer lining of the heart. Typical signs are constant chest pain, cough with dry pericarditis. The appearance of effusion between the layers of the pericardium (exudative pericarditis) is an unfavorable sign, as complications such as suppuration of the exudate or cardiac tamponade are possible.
Diagnostic methods
To diagnose variant angina, according to modern recommendations and protocols, I use an integrated approach to assessing the patient’s condition. Much in the process of identifying the underlying disease depends on the quality of the first conversation with the patient.
The key features that allow me to diagnose coronary artery spasm are:
- Episodic symptoms that are not associated with physical activity. Patients may suffer from chest pain in the morning, but go to the gym in the afternoon and do a full range of exercises.
- The appearance of discomfort at approximately the same time of day.
- The short duration of the attack, which goes away on its own with further normalization of the person’s condition.
To confirm the appropriate diagnosis, I always additionally prescribe a number of instrumental and laboratory tests.
Instrumental
Traditionally, the first step is to record an ECG. This method allows you to assess the electrical function of the heart, which changes against the background of various forms of coronary artery disease. It is important to note that there may not be any abnormalities on the ECG outside of an attack. This speaks in favor of spasm of the coronary arteries. However, for the reliability of the study, it is necessary to “catch” the patient during the period of pain, which is sometimes extremely difficult, given the night attacks. The film will record ST segment elevation, which is typical of decreased myocardial blood supply.
For the convenience of the patient and to simplify my task, I use Holter monitoring. The technique involves round-the-clock recording of an ECG in a specific patient with further interpretation of the results. With the help of this study, I can easily determine the time of the episode of coronary artery spasm.
Additional Methods
To fully assess the patient’s condition, the following procedures are also used:
- Angiography of cardiac vessels. The essence of the method is to visualize the patient’s coronary arteries on the monitor after introducing a contrast agent into the bloodstream. This allows me to pinpoint the location of the spasm. However, again, you need to “catch” the patient at the moment of the attack.
- Echocardiography. The technique is based on ultrasound examination of the heart. On the screen you can see the cavities of the organ, and I evaluate its functional activity. With Prinzmetal's angina, no special pathological changes occur.
- Test with dosed load. You are asked to exercise on a stationary bike or treadmill in a controlled environment. At this time, an ECG is recorded, pressure is measured and the general condition is assessed. If pain occurs in the heart, the procedure is stopped. However, with variant angina, patients traditionally tolerate the load well.
Based on the results of diagnostic procedures, individual treatment is selected.
How dangerous is this?
The prognosis for patients with coronary artery spasm is relatively good. The pathology does not cause critical damage to the myocardium, but in the absence of adequate treatment, the risk of developing disturbances in the rhythmic activity of the heart remains. This problem can cause a significant deterioration in the patient’s condition or even death.
Therefore, it is important to consult a doctor in time. Compliance with his recommendations in 90% of cases contributes to the complete elimination of the clinical picture and stabilization of a person’s well-being with a return to normal life.
Expert advice
The simplest and most effective advice that I give to all patients is to quit smoking. Nicotine causes a sharp vascular spasm, provoking a worsening of the disease. In some cases, eliminating tobacco may be sufficient to minimize symptoms. It is important to understand that the more negative factors simultaneously affecting you, the higher the chance of developing heart spasms. You cannot change your gender and age. However, the basic desire to quit smoking and the initiation of adequate therapy contributes to the complete elimination of the unpleasant symptoms of this disease.
Heart spasms - possible causes
The sources of the pathological condition characterized by problems with the functioning of the heart muscle have not been fully studied. Young women and adolescents are more often at risk. It should also be noted that there is an increased risk of an attack for people suffering from blood disorders (poor clotting).
In addition to capillary angina, spasm of the heart vessels can be caused by:
- vascular changes resulting from syphilis, rheumatoid diseases;
- various infections and allergic reactions to external irritants;
- some diseases of the gastrointestinal tract.
A separate group can be divided into a cause such as atherosclerosis. The disease negatively affects the patency through the coronary arteries, thereby significantly increasing the likelihood of cardiovascular spasm.
Clinical case
A 46-year-old man came to our clinic with complaints of pressing pain in the chest, which arose at rest, mainly at night, and spread to his left arm.
The patient suffers from the problem for 3 months. During the day the symptoms disappear. Exercising in the gym does not aggravate the patient's condition. The disease is associated with stress. The man smokes 1.5 packs of cigarettes per day and suffers from hypertension (160/100 mmHg). ECG at rest without abnormalities. We decided to use Holter monitoring. At three o'clock in the morning an ischemic attack lasting 4 minutes was recorded.
In the morning, when the ECG was re-registered, no pathological changes were detected. Other laboratory and instrumental tests are normal. The patient was diagnosed with IHD. Vasospastic angina, atherosclerosis of the coronary arteries. Arterial hypertension stage II, degree 2, risk. I was prescribed Amlodipine (10 mg orally once a day), Nitroglycerin (1 tablet under the tongue during an attack), Aspirin (75 mg once a day), Rosuvastatin (20 mg per day), lifestyle correction - quitting smoking, minimizing stress. When re-examined 2 weeks later, the patient noted a complete absence of new attacks of chest pain. Feels good, exercise tolerance without restrictions.
I will be glad if this article was useful. Share your experience about episodes of compressive pain in the heart in the comments: how you saved yourself and what helps better. Our experts will help you understand the situation.
Prevention of angina
It is important to understand that spasm of the heart muscle can cause myocardial infarction. Probably everyone knows that such an attack often becomes fatal. What to do and how to avoid danger?
People at risk due to congenital pathologies and age will have to take special medications that support general health.
If no irremovable provoking factors are found, then you just need to give up bad habits (especially smoking), normalize your weight if necessary, and limit your consumption of fatty and starchy foods. Periodic physical activity (walks in the fresh air, active sports) and monitoring of your psycho-emotional state will not be superfluous.