The article was published on p. 49-52
Isolated pulmonary artery stenosis (ISPA) is a congenital anomaly characterized by obstruction of the right ventricular outflow tract and disruption of the blood outflow pathways from it into the pulmonary circulation. According to ICD-10, Q 25.6 “Pulmonary artery stenosis” is distinguished. The first descriptions of the vice belong to JB De Senac (1749) and GB Morgagni (1761).
The frequency of ISHA, according to sectional and clinical data, among all congenital heart defects (CHD) ranges from 2.4 to 12%.
Clinic
Pulmonary artery stenosis can be valvular (90% of ISPA cases), subvalvular (infundibular) and supravalvular. Hemodynamic disturbances in ISLA that cause clinical manifestations are as follows:
- an obstacle to the ejection of blood from the right ventricle;
- increased pressure in the right ventricle;
- change in the structure of the cardiac cycle towards lengthening the ejection period;
- gradient (difference) of systolic pressure between the right ventricle and the pulmonary artery;
— hypertrophy of the right ventricle with a decrease in its volume;
- increased diastolic pressure in the right ventricle;
- increased systolic pressure in the right atrium;
- hypertrophy and dilatation of the right atrium, often dilatation of the oval window and discharge from the right atrium to the left and the appearance of cyanosis.
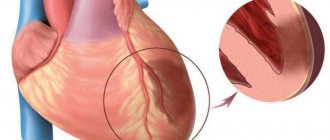
Relative insufficiency of coronary circulation of the sharply hypertrophied myocardium of the right ventricle, being the cause of pain in the heart, leads to the development of sclerotic processes and a progressive decrease in its contractile function. The right ventricle ceases to cope with the increased load, cardiac output decreases, circulatory hypoxia and cyanosis increase. The clinical picture of the defect depends on the degree of stenosis, compensatory hypertrophy, failure of the right ventricle of the heart, and the state of pulmonary blood flow in the pulmonary circulation. The clinical picture varies from asymptomatic forms to severe manifestations with severe shortness of breath at the slightest physical exertion, angina-type heart pain and cyanosis.
Why does pathology occur?
During the development of the fetus in the early stages of the mother's womb, instead of the main vessels of the heart, there is an arterial tract. Later it will form the aorta and pulmonary artery. Narrowing of the pulmonary artery occurs due to two mechanisms of congenital pathology:
- The tract is incorrectly divided into 2 halves. The partition goes to the side and takes part of the volume on the right. At the same time, it loses connection with the plate separating the atria and ventricles. This explains the frequent association of pulmonary artery stenosis with another defect - non-closure of the interventricular septum.
- The fusion of the flaps of the valve itself, closing the outlet hole.
Among the abnormal combinations, combinations of a narrowed pulmonary artery and a patent ductus botallus are observed.
Considering that valvular stenosis is a congenital pathological heart disease, specialists often diagnose pulmonary artery stenosis in newborns. The first signs of the pathological process can be detected already in the fetus; the reasons for the appearance of dysfunction at the intrauterine level are as follows:
Hereditary predisposition in parents at the genetic level to complex congenital heart disease and large vessels. Genetics on the mother’s side plays a major role in possible deviations from the norm in the formation of the fetal cardiac system.
- Gross violations of the pregnancy regime by the mother, especially in the first trimester. Such disorders include: drugs, antibiotics, psychoactive substances used by the mother. In the first trimester, the formation of systems and organs in the fetus occurs, including the cardiovascular system.
- Viral pathologies in a pregnant woman that can harm the fetus: rubella, herpes, mononucleosis.
- X-ray and other types of ionizing effects on the fetus during the period of pregnancy by the mother.
Early neonatal and postnatal diagnosis
In the first months of life, ISLA is often mild. With mild and moderate stenosis, the child has no complaints, his development is not affected, and cyanosis is not observed. Severe stenosis in newborns from the first hours of life is manifested by cyanosis and circulatory failure. The appearance of cyanosis in ISLA indicates the opening of the oval window and the presence of venous-arterial discharge of blood. Auscultation reveals a rough systolic murmur with a maximum in the II–III intercostal spaces along the left edge of the sternum and a weakening or absence of a second sound in the pulmonary artery.
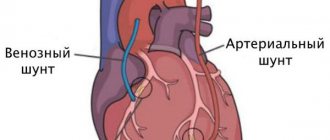
X-ray reveals significant cardiomegaly with severely depleted pulmonary blood flow. ECG: right gram, signs of hypertrophy of the right ventricle and right atrium. The degree of right ventricular overload increases as right ventricular pressure increases. When performing FCG, a high-frequency systolic rhomboid murmur is recorded, occupying the entire systole. The noise is separated from the first tone. The second sound above the pulmonary artery is widely and fixedly split, the pulmonary component is significantly weakened (Fig. 1).
On EchoCG: narrowing at the level of the valves or subvalvular space (Fig. 2, 3), hypertrophy of the myocardium of the anterior wall of the right ventricle and interventricular septum, enlargement of the right atrium cavity, etc.
The criteria for postnatal diagnosis are as follows:
I. Clinical:
- with severe stenosis, complaints of fatigue, shortness of breath on exertion, dizziness, fainting, stabbing or intense squeezing pain in the heart area during physical activity;
— pallor of the skin, cyanosis is not typical, its appearance during exercise (cyanosis of the lips) is often associated with the presence of an open oval window;
- at school age, the child is noticeably lagging behind in physical development, signs of chronic hypoxia (“drumsticks”, “watch glasses”);
- cardiac hump, systolic tremors in the II–IV intercostal spaces to the left of the sternum, cardiac impulse, epigastric pulsation can be detected (due to hypertrophy of the right ventricle);
- increase in the size of the heart in diameter;
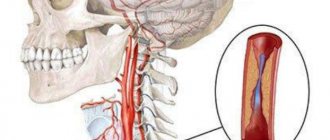
- significant weakening of the second sound over the pulmonary artery, intense, rough, prolonged (at 2/3 of systole) systolic murmur along the left edge of the sternum with a maximum in the 2nd intercostal space or, with infundibular stenosis, in the 3rd–4th intercostal spaces, increasing towards mid-systole and not covering both heart sounds. The noise radiates to the left collarbone, to the vessels of the neck, to the back between the middle of the left shoulder blade and the spine.
II. Paraclinical:
- X-ray: a protruding arch of the pulmonary artery, the boundaries of the heart are usually not expanded, with severe stenosis a decrease in pulmonary vascularization is detected, with the development of right ventricular failure an enlargement of the right ventricle and right atrium is determined (Fig. 4);
— ECG: deviation of the EOS to the right, signs of severe hypertrophy of the right ventricle and right atrium, downward shift of the ST interval and a negative T wave in the right precordial leads (indicates an extreme degree of overload);
— EchoCG: determines pulmonary artery stenosis and details its anatomical variant.
Differential diagnosis should be carried out with atrial septal defect, ventricular septal defect, tetralogy of Fallot, Ebstein's anomaly.
Pulmonary stenosis in newborns
In newborns, a severe (critical) form of stenosis causes heart failure and a bluish tint to the skin, and a pronounced heart murmur raises suspicion.
The pressure gradient can disappear over time and be compensated by the internal forces of the body, however, the condition of the resulting post-stenotic aneurysmal dilatations of small vessels can be complicated by thrombosis and arteritis , causing pulmonary hemorrhages. Severe stenoses can lead to death, both in infancy and in subsequent periods of life.
Treatment
Patients with mild to moderate stenosis (gradient less than 25 mm Hg) do not require drug correction. Digoxin is contraindicated for them. In all cases, antibacterial prophylaxis for infective endocarditis is recommended. If right ventricular failure with cyanosis develops, oxygen therapy and the administration of prostaglandin E1 are prescribed until surgical correction of the defect is performed.
The optimal age for the operation is primary school age; the results of the operation when correcting a defect are worse at the age of under three years and over 25 years. For emergency indications in cases of severe stenosis, surgical intervention can be performed in the first months of the child’s life. Patients requiring surgical treatment in the neonatal period due to a pronounced pressure gradient (50–60 mm Hg), right ventricular myocardial hypertrophy and cyanosis can undergo balloon valve repair. According to the literature, the results of this operation are excellent, with only rare complications noted. Management of patients with severe pulmonary artery stenosis depends on the anatomical structure of the right ventricle (size of the ventricle, diameter of the valve opening, presence of sinusoidal communications with the coronary arteries). These patients are indicated for reconstructive surgery.
General information about heart defects in children
Heart disease
- a violation of the anatomical structure of the walls or valves of the heart, as well as the blood vessels that enter or exit it. Cardiac function and hemodynamics in the entire circulatory system are impaired.
Depending on the reasons for development, there are congenital
and
acquired vices
.
It is believed that congenital ones appear during the first weeks of pregnancy during the “initial formation” of future life. The reasons for the development of defects have not been studied reliably, but they predispose to them:
- genetic diseases (50% of children with Down syndrome suffer from this disorder);
- diabetes mellitus in a pregnant woman;
- bad habits of the expectant mother (half of children with fetal alcohol syndrome (FAS) have heart defects);
- infections (a mother who has had rubella in the first trimester will almost always have a child with severe pathology);
- taking medications prohibited for pregnant women;
- phenylketonuria in an expectant mother.
However, heart disease does not always develop from birth. It can manifest itself as a complication of diseases suffered in childhood (rheumatism, influenza, tonsillitis) in severe forms. This disorder is called an acquired defect.
hearts.
Forecast
Children with successful balloon valve repair have a favorable prognosis for life. Patients with a dysplastic pulmonary valve, often found in Noonan syndrome, have less favorable outcomes. Patients with successful balloon repair rarely require reoperation, unlike patients with right ventricular hypoplasia. The survival rate for such children is 60%. Mild to moderate pulmonary stenosis usually does not progress, and children have a favorable prognosis. In patients with severe stenosis, the defect progresses with age. The average life expectancy in the natural course of the defect is 25 years. After surgery, restenosis and valvular insufficiency of the pulmonary artery are possible. Long-term good results after surgical treatment were recorded in 84.3% of patients.
Classification
Depending on the location of the narrowing, there are:
- valvular stenosis is the most common case when the pulmonary valve itself is subject to pathological changes; its valves can be underdeveloped, fused together by commissures, and even have the appearance of a membrane with a hole in the center, ranging in size from 1-1.5 mm to normal;
- supravalvular - in which the trunk of the pulmonary artery is narrowed above the location of the valve;
- subvalvular (infundibular) – in this case, excessive growth of muscle tissue or fibrous structures in the area of the outflow tract of the right ventricle has occurred, preventing the blood flow from entering the pulmonary artery;
- peripheral - caused by a narrowing of the branches of the pulmonary artery that bring blood to the right or left lung.
According to the nature of the severity, the disease can be mild (asymptomatic), moderate-severe and critical.
Diagnosis of heart defects in children
During the initial examination, a pediatrician, neonatologist or pediatric cardiologist conducts an examination and auscultation of possible heart murmurs. The presence of swelling, shortness of breath, heart rhythm disturbances, and problems with physical or intellectual development are checked. Based on the results of the inspection, the question of the necessary examination is decided.
Cardiac echocardiography (EchoCG) – combines cardiac ultrasound and cardiogram. The method determines the rhythmogram and structural changes in the heart. EchoCG is an informative method.
Radiology shows the actual size of the heart, its chambers and the relationship of the organ to the size of the chest.
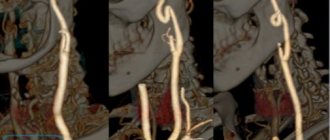
Coronary angiography – a catheter is inserted through the veins or arteries in the arm, groin, or neck (vein only) and reaches the heart. Then a contrast agent is passed through it. This method determines the contractile function of the heart.
Medical equipment uses expert-class equipment from world-famous manufacturers.
The task of the Children's Medical Department is to provide a full range of medical care from prevention to treatment, when symptoms of a defect appear from birth to 18 years.
In our children's department, appointments are conducted by doctors who have undergone special training to identify health problems in children and infants, taking into account all age-related characteristics.
Pediatric doctors at the Paracelsus Clinic work according to the principles of evidence-based medicine (international protocols drawn up on the basis of clinical trials). This minimizes the likelihood of a false diagnosis.
Parents play a big role in the early diagnosis of heart defects in children. The direction in which the preliminary examination will be carried out depends on how closely the parents monitor the health of their child and how correctly they can describe his condition to the doctor.