The heart begins to beat long before we are born. Surprising and even magical, right? However, this means that this organ works longer and harder than others. And not only the quality of our life, but also life itself depends on how carefully we pay attention to his condition!
More than 17 million people die every year from heart and vascular diseases. It has been proven that 80% of premature heart attacks and strokes could be prevented!
Fortunately, most cardiovascular diseases are successfully diagnosed thanks to modern innovative equipment and the professionalism of doctors. And as you know, establishing an accurate diagnosis means taking an important step towards healing.
One of the most informative and safe studies is cardiac echocardiography (EchoCG) or, in other words, ultrasound of the heart.
1 ECHO-KG in "MedicCity"
2 Echocardiography at MedicCity
3 Ultrasound of the heart at MedicCity
The essence of echocardiography
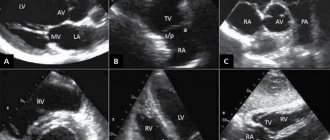
Ultrasound of the heart is the process of studying all the main parameters and structures of this organ using ultrasound.
When exposed to electrical energy, the echocardiograph transducer emits high-frequency sound that travels through the structures of the heart, is reflected from them, captured by the same transducer and transmitted to the computer. He, in turn, analyzes the received data and displays it on the monitor in the form of a two- or three-dimensional image.
In recent years, echocardiography has been increasingly used for preventive purposes, which makes it possible to identify cardiac abnormalities at an early stage.
What does an ultrasound of the heart show:
- heart size;
- integrity, structure and thickness of its walls;
- sizes of the cavities of the atria and ventricles;
- contractility of the heart muscle;
- operation and structure of valves;
- condition of the pulmonary artery and aorta;
- pulmonary artery pressure level (to diagnose pulmonary hypertension, which can occur with pulmonary embolism, for example, when blood clots from the veins of the legs enter the pulmonary artery);
- direction and speed of cardiac blood flow;
- condition of the outer shell, pericardium.
1 ECHO-KG in "MedicCity"
2 Echocardiography at MedicCity
3 Ultrasound of the heart at MedicCity
Establishment of clinical class and verification of diagnosis
Pulmonary function tests can identify obstructive or restrictive changes for the purpose of differential diagnosis of PH and clarify the severity of lung damage. Patients are characterized by a decrease in the diffusion capacity of the lungs for carbon monoxide (40-80% of normal), a slight or moderate decrease in lung volumes, a normal or slightly decreased PaO2, and usually a decreased PaCO2 due to alveolar hyperventilation.
Ventilation-perfusion lung scintigraphy is a screening method to exclude chronic thromboembolism as a cause of pulmonary hypertension. In patients after thromboembolism, perfusion defects are found in the lobar and segmental zones in the absence of ventilation disturbances. Perfusion scintigraphy has historically become one of the first methods for detecting perfusion defects in the pulmonary parenchyma in pulmonary embolism. The images obtained in acute PE and CTEPH differ significantly. Perfusion defects in acute PE are more clearly defined and contrast sharply with normally functioning tissue. In CTEPH, perfusion defects are not clearly defined and often do not correspond to the blood supply area of the large pulmonary artery.
Computed tomography and CT angiopulmonography
The CT picture of chronic thromboembolism can be represented by occlusions and stenoses of the pulmonary arteries, eccentric filling defects due to the presence of blood clots, including recanalized ones. CT angiopulmonography is performed on spiral computed tomographs during the phase of passage of the contrast agent through the pulmonary arterial bed. Among the methodological features, it should be noted that the study must be carried out using at least an 8-spiral tomograph, with a minimum step (no more than 3 mm) and a slice thickness (no more than 1 mm). A thorough scan should cover both lungs completely, from the apices to the phrenic sinuses. Contrast enhancement of the right chambers of the heart and pulmonary arteries should match or exceed the degree of contrast enhancement of the left chambers of the heart and aorta. The second, arterial phase of scanning is recommended for all patients over 40 years of age, especially if there is evidence of arterial thrombosis and coronary artery disease in the anamnesis. Modern software allows you to reconstruct images of the pulmonary arteries in any plane, construct maximum intensity projections and three-dimensional images. In most cases, to clarify the nature of the lesion, it is enough to analyze cross sections using an image viewer, which makes it possible to determine the presence of changes not only in the lobar and segmental branches, but also in a number of subsegmental arteries. Pathological changes, in addition to the presence of “old” thrombotic material, may include local thickening of the vessel wall, narrowing at the mouth of the vessels and along them, occlusions, intravascular structures in the form of membranes and bridges. If changes are detected in several branches of the pulmonary arteries, we can conclude that there is a high probability of thromboembolic nature of PH. It is important to note that the resolution of modern CT scanners is limited and does not allow the determination of very thin membranous and stringy structures in the lumen of the LA, especially if the size of the object does not exceed 2-3 mm. In some cases, calcification of the “old” thrombotic material develops, and CT can be invaluable in determining the location of the calcification. CT makes it possible to detect not only stenotic changes in the vessels of the lungs, but also disturbances in the perfusion of lung tissue by the nature of the contrast of the parenchyma. In some cases, parenchymal enhancement is so uneven that mosaic enhancement is detected on scans. A clearly defined mosaic pattern of segments usually indicates a good prognosis for surgical treatment. Contrasting exclusively in the root zones is not a true mosaic and is often observed in microvascular forms of PH. By providing detailed images of the lung parenchyma, CT allows the diagnosis of other lung diseases. In addition to the state of the arterial bed, CT can provide comprehensive information about all intrathoracic structures, which is important for confirming the diagnosis and developing a surgical treatment plan. Before performing the operation, the condition of the pulmonary parenchyma, bronchial tree, and pulmonary veins should be taken into account.
Angiographic diagnostics
The main objectives of angiographic diagnosis are to determine the severity of pulmonary hypertension, clarify the nature of the lesion in the pulmonary bed through angiopulmonography, and identify/exclude coronary disease. Carrying out catheterization in isolation without high-quality angiopulmonography in a patient with clear signs of CTEPH is inappropriate. This study should provide clear information to doctors to resolve the issue of the patient’s operability and the severity of his condition. Hemodynamic criteria for post-embolic pulmonary hypertension, identified during catheterization of the right heart, are: mean pulmonary artery pressure (PAP) above 25 mm Hg. Art., pulmonary artery wedge pressure (PAWP) ≤ 15 mm Hg. Art., PVR > 2 units. according to Wood (160 dyn. sec cm-5) in the presence of multiple stenotic and/or occlusive lesions of the branches of the pulmonary artery of various calibers.
Who is prescribed echocardiography?
The following are routinely examined:
- infants - if congenital defects are suspected;
- teenagers are a time of intensive growth;
- pregnant women with existing chronic diseases - to decide on the method of childbirth;
- professional athletes - to monitor the state of the cardiovascular system.
An echocardiogram is required if:
- anomalies of the endocardium and valve apparatus:
- heart tumors;
- arrhythmias;
- threat of a heart attack or a heart attack;
- IHD;
- failures of cardiac activity due to various intoxications;
- attacks of angina pectoris;
- pericarditis of various origins;
- hypertension;
- heart failure.
And also in the process of treating heart diseases, before and after cardiac surgery.
Treatment
Standards for the treatment of pulmonary hypertension require a combination of adequate therapy with the use of drugs, implementation of recommendations to reduce symptoms, and surgical methods. Non-drug methods of treating pulmonary hypertension syndrome involve maintaining a water-salt balance, moderate physical activity and oxygen therapy. Doctors at the Yusupov Hospital recommend that patients diagnosed with pulmonary hypertension observe the following restrictions:
- Reduce fluid intake - no more than 1.5 liters per day. Also reduce salt intake;
- Avoid climbing to heights (no more than 1000 meters);
- Avoid fainting, shortness of breath and chest pain, which can be achieved through dosed physical activity.
To treat pulmonary hypertension, drugs are used whose action is aimed at restoring the function of the respiratory and cardiovascular systems. Using medication, specialists are able to reduce the load on the heart, dilate blood vessels and lower blood pressure.
At the Yusupov Hospital, cardiologists prescribe the following pharmacological drugs to patients with pulmonary hypertension:
- Calcium antagonists. They change the heart rate, relax the muscles of the bronchi, reduce spasm of pulmonary vessels, reduce platelet aggregation, increase the stability of the heart muscle;
- Diuretics. Remove excess water from the body, reduce blood pressure;
- ACE inhibitors. Dilate blood vessels, reduce the load on the heart, reduce blood pressure;
- Nitrates;
- Antiplatelet agents. Reduce the ability of red blood cells and platelets to stick together. Prevents them from sticking to the inner lining of blood vessels;
- Direct acting anticoagulants. These drugs prevent the formation of fibrin (a substance in the blood that forms the basis of a blood clot) and also prevent the formation of blood clots (thrombi);
- Indirect anticoagulants. Drugs belonging to this group affect blood clotting and also reduce blood clotting;
- Endothelin receptor antagonists;
- Bronchodilators. These drugs improve ventilation;
- Nitric oxide NO in the form of inhalations - for vasodilation;
- Antibiotics - if there is a bronchopulmonary infection;
- Prostaglandins. Powerful vasodilators that have a whole range of additional effects, such as preventing the adhesion of platelets and red blood cells, slowing down the formation of connective tissue, and reducing damage to endothelial cells.
Severe pulmonary hypertension in adults requires surgical treatment:
- Thromboendarterectomy – removal of blood clots from blood vessels;
- Atrial saptostomy - creating an opening between the atria to reduce pressure;
- Transplantation of the lung and heart complex or just the lung is used in the later stages of the disease and in the presence of other diseases.
To stop the progression and prevent complications of the disease, contact specialists at the Yusupov Hospital in a timely manner.
When is a cardiac ultrasound performed?
Indications for cardiac ultrasound are:
- alarming changes in health (increased or interrupted heartbeat, shortness of breath, swelling, weakness, prolonged fever, chest pain, cases of loss of consciousness);
- changes detected in the last ECG;
- increased blood pressure;
- heart murmurs;
- cardiomyopathy;
- manifestations of coronary heart disease;
- heart defects (congenital, acquired);
- pericardial diseases;
- lung diseases.
Kinds
Doctors distinguish several main types of pulmonary hypertension:
- Primary – a disease of unknown origin, which can be either congenital or acquired. The disease is called “idiopathic pulmonary hypertension.” It is characterized by changes in the pulmonary artery and enlargement of the right ventricle. Primary pulmonary hypertension causes disability for the patient, and if left untreated, leads to death;
- Secondary - develops as a complication of other diseases: congenital and acquired heart defects, HIV infection, connective tissue diseases, bronchial asthma, pathology of the respiratory system. The disease can develop due to blockage of blood vessels by blood clots. In this case, chronic pulmonary hypertension is diagnosed.
Preparation for cardiac echocardiography
Ultrasound of the heart does not require special preparations. On the eve of the procedure, the patient is free to eat as usual and perform normal activities. The only thing that will be asked of him is to give up alcohol, caffeine-containing drinks, and strong tea.
If the patient is constantly taking medications, this must be warned in advance so that the results of the study are not distorted.
For each subsequent ultrasound of the heart, you should take a transcript of the previous one. This will help the doctor see the process over time and draw the right conclusions about your condition.
The examination itself takes from 15 to 30 minutes.
The patient, undressed to the waist, is lying on his back or side. A special gel is applied to his chest, ensuring easier sliding of the sensor over the area under study (the patient does not experience discomfort).
The specialist performing echocardiography has access to any areas of the heart muscle - this is achieved by changing the angle of the sensor.
Sometimes standard ultrasound of the heart does not provide complete information about the functioning of the heart, so other types of echocardiography are used. For example, fat on the chest of an obese person can interfere with the passage of ultrasound waves. In this case, transesophageal echocardiography is indicated. As the name suggests, the ultrasound probe is inserted directly into the esophagus, as close to the left atrium as possible.
And to screen cardiac function under stress, the patient may be prescribed stress echocardiography. This study differs from the usual one in that it is performed with a load on the heart, achieved by physical exercise, special medications or under the influence of electrical impulses. It is used primarily to identify myocardial ischemia and the risk of complications of coronary artery disease, as well as for certain heart defects to confirm the need for surgery.
Symptoms
Pulmonary hypertension does not have pronounced symptoms, so treatment begins in the later stages of the disease. At the onset of the disease, the following symptoms can be detected:
- The appearance of slight shortness of breath at rest or with little physical activity;
- Hoarse voice or dry cough;
- Loss of body weight for no apparent reason;
- Rapid heartbeat, as the disease progresses, pulsation of the jugular vein is clearly noticeable in the patient’s neck;
- Depressed mood and constant feeling of fatigue and weakness;
- Fainting and dizziness, which are a consequence of hypoxia - lack of oxygen.
- In later stages, pulmonary hypertension is manifested by the following symptoms:
- Heart rhythm disturbances - arrhythmia;
- Symptoms of myocardial ischemia and angina attacks, in which the patient is overcome by a feeling of fear, cold sweat appears and pain appears in the chest;
- Hemoptysis and the appearance of blood streaks in the sputum.
At the terminal stage, tissue death occurs due to the formation of blood clots in the arterioles. Hypertensive crises in patients occur at night. Acute heart failure or blockage of the pulmonary artery by a thrombus can be the main causes of death.
Make an appointment
Decoding EchoCG
After the examination, the doctor draws up a conclusion. First, a visual picture with the presumed diagnosis is described. The second part of the study protocol indicates the patient’s individual indicators and their compliance with standards.
Decoding the data obtained is not a final diagnosis, since the study can be done not by a cardiologist, but by an ultrasound diagnostic specialist.
It is the cardiologist, based on the collected medical history, examination results, interpretation of tests and data from all prescribed studies, who can draw accurate conclusions about your condition and prescribe the necessary treatment!
EchoCG norm: what some parameters indicate
There is a range of normal values for one or another cardiac ultrasound indicator for adults (in children the norms are different and directly depend on age).
Thus, along with other important parameters, echocardiography helps to obtain information about the ejection fraction of the heart - this indicator determines the efficiency of the work performed by the heart with each beat.
Ejection fraction (EF) is the percentage of blood volume ejected into the vessels from the heart ventricle during each contraction. If there were 100 ml of blood in the ventricle, and after the heart contracted, 55 ml entered the aorta, it is considered that the ejection fraction was 55%.
When the term ejection fraction is heard, we are usually talking about the left ventricular (LV) ejection fraction, since it is the left ventricle that ejects blood into the systemic circulation.
A healthy heart, even at rest, pumps more than half of the blood from the left ventricle into the vessels with each beat. As the ejection fraction decreases, heart failure develops.
The normal left ventricular ejection fraction for an adult is 55-70%. A value of 40-55% indicates that EF is below normal. An ejection fraction of less than 40% and even lower ejection fractions indicate heart failure in the patient.
- Magazine archive /
- 2012 /
- №17
Medicines to treat pulmonary hypertension
E.A. Ushkalova, N.K. Runikhina, I.M. Novikova
Federal State Budgetary Institution “Scientific Center of Obstetrics, Gynecology and Perinatology named after. IN AND. Kulakov” Ministry of Health and Social Development of Russia
A review is presented on the pharmacotherapy of pulmonary hypertension (PH), which occurs as a result of a progressive increase in pulmonary vascular resistance, which leads to right ventricular failure and premature death. Based on the results of numerous clinical studies, the article analyzes the effectiveness and safety of drugs that are used as primary and maintenance therapy for PH. Maintenance pharmacotherapy includes the use of anticoagulants, cardiac glycosides and diuretics. Drugs for specific therapy for PH include calcium channel blockers, prostacyclin analogues, endothelin receptor inhibitors and phosphodiesterase-5 (PDE-5) inhibitors.
Key words: pharmacotherapy of pulmonary hypertension, right ventricular heart failure, pulmonary hypertension
Pulmonary hypertension (PH) is a syndrome resulting from restricted blood flow through the pulmonary arterial circulation, which leads to increased pulmonary vascular resistance and ultimately to right ventricular heart failure [1]. PH is a fairly rare pathology, occurring with a frequency of 15 per 1 million population [2]. The prognosis for PH is unfavorable, mortality among patients receiving modern therapy is 15% within a year [3], the average survival from the moment of diagnosis is 2.8–5.0 years [4–7].
The choice of therapy for PH is determined by the form and severity of the disease, so the effectiveness of treatment largely depends on the thorough examination of the patient [8, 9]. Treatment should begin only after verification of the diagnosis by catheterization of the right heart and acute tests with vasodilators [10].
Drug therapy for PH is divided into primary and maintenance. Maintenance pharmacotherapy includes the use of anticoagulants, cardiac glycosides and diuretics. It should be noted that the use of maintenance pharmacotherapy is based on a limited evidence base (see table).
. Recommendations for the use of maintenance therapy in patients with PH [15].
Thus, the use of anticoagulants is determined primarily by information about impaired coagulation and fibrinolysis in these patients [11–13], as well as autopsy data on the high prevalence of thrombotic lesions among them [14]. In addition, among patients with PH there are nonspecific risk factors for venous thromboembolism, such as heart failure and limitation of physical activity.
Studies of oral anticoagulants, mainly single-center and retrospective, were conducted for patients with idiopathic PH, hereditary PH and PH caused by the use of anorexigenic drugs [15]. Some studies have shown an improvement in the survival rate of patients with PH [16]. In the International Guidelines for the Treatment of PH, oral anticoagulants are recommended for patients with idiopathic and chronic thromboembolic forms of the disease [1, 15]. Anticoagulant therapy, due to the increased risk of catheter-associated thrombosis, in the absence of contraindications, is also carried out in patients receiving prostacyclin analogues for intravenous administration for a long time.
The recommendation for the use of warfarin in patients with idiopathic PH is based on the results of one prospective and two retrospective observational uncontrolled studies [17].
When prescribing anticoagulants, it is recommended to carefully weigh their potential benefits and the risk of bleeding, especially for patients with portopulmonary PH and severe varicose veins of the esophagus. There is no complete consensus on the target international normalized ratio (INR) when using anticoagulants in patients with PH. In North American countries, it is recommended to maintain an INR of 1.5–2.5; in Europe – 2.0–3.0 [1, 15].
Randomized clinical trials of diuretics for PH have not been conducted. They are recommended for symptomatic therapy in patients with right ventricular failure [15, 18]. Selecting a specific
diuretic drug in international recommendations is left to the discretion of the attending physician [1, 15], in Russian recommendations preference is given to loop diuretics: furosemide (20–120 mg/day), ethacrynic acid (50–100 mg/day), torsemide (5–10 mg/day) [18]. An aldosterone antagonist can be added to the main diuretic drug [1, 18]. To avoid a sharp decrease in circulating blood volume and blood pressure (BP), diuretic doses must be carefully titrated. During treatment, serum electrolyte levels and renal function should be monitored.
The use of cardiotonics, mainly digoxin, is recommended for right ventricular failure and to reduce the ventricular rate in patients with PH with atrial fibrillation or flutter [1]. One study showed that intravenous digoxin in patients with idiopathic PH leads to a moderate increase in cardiac output and a decrease in circulating norepinephrine levels [19], but there are no data on the effect of chronic digoxin use in these patients. Practical experience shows that intravenous dobutamine often leads to improvement of varying duration among patients with end-stage PH, but no clinical studies of dobutamine have been conducted in this category of patients.
Drugs for specific therapy for PH include calcium channel blockers, prostacyclin analogues, endothelin receptor inhibitors and phosphodiesterase-5 (PDE-5) inhibitors. Calcium channel blockers have been used as a treatment for PH since the mid-1980s. The basis for their use was the pathogenetic changes that occur during idiopathic PH: hypertrophy and hyperplasia of smooth muscle cells, vasoconstriction. No RCTs of the effect of drugs in this group have been conducted in patients with PH. In single-center, non-randomized, uncontrolled studies, the use of calcium channel blockers in patients with idiopathic PH was associated with a beneficial effect on survival [20, 21]. However, in recent years, quite a lot of data have been obtained indicating that only a small number of patients with idiopathic PH (10–15%) who had a positive response to an acute vasoreactivity test can benefit from the use of drugs in this group [22].
In PH associated with connective tissue diseases, the role of calcium channel blockers is even more limited by the small number of responders to vasoreactivity tests and poor tolerance of high doses of these drugs [23]. In addition, in most associated forms of PH, including PH associated with connective tissue diseases, HIV infection, portal hypertension, and veno-occlusive disease/pulmonary capillary hemangiomatosis, even patients with a positive response to an acute vasodilator test rarely demonstrate an adequate therapeutic response to long-term therapy with calcium channel blockers [23]. The only exceptions are patients in whom PH is associated with the use of anorexigenic drugs [24].
In patients who have failed vasodilator tests or have had a negative response to these tests, calcium channel blockers are not recommended due to the risk of severe side effects (hypotension, syncope, right ventricular failure) and the low likelihood of effectiveness. The choice of a specific calcium channel blocker depends on the baseline heart rate. In patients with relative bradycardia, preference is recommended to be given to nifedipine and amlodipine, and for tachycardia, diltiazem is recommended. It is recommended to avoid the use of verapamil due to the potential negative inotropic effect. Calcium channel blockers are used in high daily doses: nifedipine – 120–240 mg, diltiazem – 240–720 mg and amlodipine – up to 20 mg/day. However, treatment should be started with a low dose (for example, nifedipine slow-release 30 mg twice daily, diltiazem 60 mg three times daily or amlodipine 2.5 mg/day), and then gradually and cautiously increased to as portable as possible. Factors limiting dose increases are usually systemic hypotension and edema of the lower extremities.
During treatment with calcium channel blockers, their effectiveness and safety should be carefully monitored. The first assessment of the effectiveness of therapy, including catheterization of the right heart, is recommended to be carried out 3–4 months after their appointment [15]. If a patient with a positive response to a test with a vasodilator during treatment with calcium channel blockers cannot achieve improvement (transition to functional class I or II), it is recommended to add drugs of other groups or transfer him to another therapy.
The use of prostacyclin analogues, endothelin receptor antagonists and PDE-5 inhibitors is based on modern ideas about the pathogenesis of PH (according to which there are 3 main therapeutic targets - increasing the effects of prostacyclin and nitric oxide and reducing the effects of endothelin [25]. Beneficial effect of prostacyclin analogues (prostanoids) in PH due to the presence of vasodilator, antiaggregation and antiproliferative properties [15]. The first drug of this group registered for the treatment of PH was epoprostenol. It is intended for intravenous administration, has a rapid effect, reaching stable concentrations in the blood in less than 30 minutes after administration, but has a very short half-life (less than 6 minutes), and therefore must be administered continuously using an infusion pump and central venous catheter.26 The drug remains stable at room temperature for no more than 8 hours, so it must be kept refrigerated. In addition, the disadvantage of epoprostenol is the development of tolerance to it, which requires a constant increase in dose [27]. The effectiveness of epoprostenol for patients with idiopathic PH has been demonstrated in several RCTs and systematic reviews [26–31]. One-, two-, and three-year survival rates with this drug were 87.8%, 76.3, and 62.8%, which significantly exceeded the expected survival rate calculated on the basis of historical controls (58.9%, 46.3, and 35. 4%, respectively) [32]. According to the results of a meta-analysis, the introduction of epoprostenol into medical practice increased the five-year survival rate from 34 to 67% [33].
A factor limiting the use of epoprostenol is its tolerability. Side effects with long-term use of the drug are common. The most common among them are headache, redness of the skin, pain in the lower jaw, diarrhea, nausea, erythematous rash, pain in the back, legs and feet [27]. Sometimes systemic hypotension develops. The frequency and severity of side effects depend on the dose. The maximum tolerated dose for most patients is 20–40 ng/kg/min [29, 32]. In addition, when using the drug, there is a risk of developing serious adverse events associated with the route of administration - improper functioning of the infusion pump, catheter obstruction, infection at the injection site and sepsis. In this regard, the administration of epoprostenol is recommended only in centers with experience with this drug [34].
The tricyclic benzidine derivative of epoprostenol, treprostinil, has a longer half-life (4.5 hours) and satisfactory stability, allowing it to be administered in saline at ambient temperature both intravenously and subcutaneously. When administered intravenously, treprostinil causes fewer side effects than epoprostenol, but comparative studies on the effectiveness of these drugs have not been conducted [35–38]. Subcutaneous administration, carried out using a microinfusion pump and subcutaneous catheters, can significantly reduce the risk of infectious complications compared with intravenous administration [27]. Recently, a dosage form of treprostinil for inhalation administration was registered abroad; the oral form of the drug is at the stage of pre-registration studies. Compared with iloprost (see below), the inhalation form of treprostinil has a number of advantages - less frequent administration, shorter inhalation time, and a more convenient nebulizer to use [39].
The efficacy and safety of subcutaneous treprostinil for patients with functional classes II–IV PH were demonstrated in two placebo-controlled RCTs, including a large double-blind study involving 470 patients [40]. In an open study involving 860 patients with PH, the one-year survival rate with subcutaneous treprostinil was 91%, and the four-year survival rate was 72% [41]. A factor limiting the subcutaneous administration of the drug, especially in pediatrics, is the pain of the injections.
Iloprost, intended for inhalation administration using a nebulizer, is administered 6–9 times a day for 10–15 minutes. Its advantage over injection drugs is a lower incidence of systemic side effects, including a decrease in systemic blood pressure. In general, iloprost is well tolerated, including with long-term use [42], but can cause reactive bronchospasm, especially in children [43].
In a multicenter randomized trial, 3 months of iloprost treatment (a composite endpoint of at least 10% improvement in 6-minute walk test and FC improvement) was significantly superior to placebo [44]. According to the results of a meta-analysis, iloprost is equally effective as the endothelin receptor antagonist bosentan and the PDE5 inhibitor sildenafil, but more often causes serious side effects [45]. The 2-year survival rate with its use was 87% (compared to the expected 63%), the average dose increase over 2 years was 16% [42].
The drug is recommended as a treatment for patients with idiopathic PH of class III and IV. In a number of Asian countries, the oral prostacyclin analogue beraprost is approved for the treatment of PH, but in the USA and Europe its further studies were abandoned due to an unfavorable benefit/risk ratio [34]. Improvement in symptoms, observed in clinical studies only in the first 3–6 months of treatment with beraprost, was accompanied by frequent development of side effects [46]. A longer-acting analogue of beraprost is currently being studied in clinical trials [47].
In general, prostacyclins are considered as the drugs of choice for patients with severe idiopathic PH, but their use in the early stages of the disease also brings significant benefits to patients with mild and moderate forms [48]. Available data suggest that prostacyclin analogues are also effective in PH associated with systemic connective tissue diseases, heart defects and HIV infection [15]. Evidence is accumulating that prostanoid therapy helps normalize C-reactive protein levels, a factor associated with improved long-term outcomes [49].
Endothelin receptor antagonists eliminate the vasoconstrictor and mitogenic effects of endothelin-1 (ET1), which plays an important role in the pathogenesis of PH. Currently, two drugs in this group are used in Europe and North America - bosentan and ambrisentan. A third endothelin receptor antagonist, sitaxentan, was voluntarily withdrawn from the market by the manufacturer in December 2010 due to two cases of fatal hepatotoxicity [50]. Only bosentan is registered in the Russian Federation. It is a “double” antagonist of endothelin receptors ET1 – ETA and ETB. The drug is intended for oral administration and has quite favorable pharmacokinetic properties that allow it to be used 2 times a day.
The effectiveness of bosentan has been demonstrated in clinical studies of patients with idiopathic PH. The use of bosentan led to an increase in exercise tolerance compared to placebo, an improvement in FC, cardiopulmonary hemodynamics and quality of life in patients, as well as a slowdown in disease progression [51–54]. A number of studies have shown a significant improvement in patient survival compared with historical controls [55–57]. In one study, the one- and two-year survival rates for bosentan were 97% and 91%, compared with 91% and 84% for epoprostenol [56]. In addition to the effect on survival, according to an open study, bosentan increased the quality-adjusted life years of patients with PH by 3.49 years compared with historical controls [58]. However, a Cochrane meta-analysis (11 RCTs, 1457 patients) was able to identify only a trend towards a decrease in mortality among patients with PH who received endothelin receptor antagonist drugs, including bosentan [59]. In another meta-analysis (10 RCTs, 1635 patients, including 23.9% with PH associated with connective tissue diseases and 18.2% with congenital heart disease), the predicted survival rate with bosentan was 77.8 % within a year, 67.7% - 2 years and 59.3% - 3 years, which was significantly worse than the above indicators [60]. There is evidence of the effectiveness of bosentan for patients with PH associated with HIV infections [56], congenital heart diseases [61, 62] and connective tissue diseases [63–66]. Bosentan appears to be a promising drug for the treatment of chronic thromboembolic PH [67, 68]. According to the results of a meta-analysis, its use is associated with improvements in hemodynamics and, possibly, exercise tolerance in these patients [69].
The main problem with the use of bosentan is its hepatotoxicity. According to the manufacturer, an increase in the level of hepatic aminotransferases by more than 3 times is observed among 11% of patients receiving the drug [70]. Hepatotoxicity is dose-dependent: in the BREATHE-1 study, the incidence of liver enzyme elevations was 14% with bosentan 250 mg twice daily and 4% with bosentan 125 mg twice daily (3 in the placebo group). %) [63]. An analysis of data from 4994 patients (observation period - 30 months) who took bosentan in real medical practice showed that the frequency of increases in liver enzymes by 3 times compared with the upper limit of normal was 7.6% with its use, the frequency of drug discontinuation for this reason – 3.7% [71].
During the first weeks of treatment with bosentan, a decrease in hemoglobin levels is observed, which stabilizes approximately 12 weeks after the start of therapy [72]. In the BREATHE-5 study, among patients with Eisenmenger syndrome who received the drug, a small statistically insignificant decrease in mixed venous blood saturation was noted, which was not accompanied by the development of adverse clinical events [61].
In 10–19% of patients with PH, bosentan can cause peripheral edema [61, 64, 71, 73]. The mechanism of their development is not entirely clear. In some patients, edema occurs due to worsening right ventricular failure, but it may also be due to vasodilation caused by endothelin receptor antagonists or effects on renal tubular function [74]. Ambrisentan, unlike bosentan, is a selective ETA receptor antagonist and has a longer half-life (9–15 hours), allowing it to be administered once a day. Its effectiveness when taken orally in doses of 2.5 to 10 mg/day in patients with PH is confirmed by the results of RCTs [75, 76]. The use of the drug led to an improvement in the condition of patients according to the results of the 6-minute walk test and assessment on the Borg Individual Perception of Exertion Scale, improvement in LH FC, hemodynamic parameters and quality of life of patients.
Ambrisentan causes hepatotoxic reactions less frequently than bosentan [77]. In some clinical studies, the incidence was less than 1%, but in these studies the incidence of liver enzyme elevations in placebo patients was also very low [78]. It should be noted that the incidence of hepatotoxic reactions with sitaxentan, which was subsequently withdrawn from the market due to fatal liver damage, was also lower in clinical studies (7%) than in studies of bosentan [78]. Ambrisentan is less likely than bosentan to enter into clinically significant drug interactions [79].
Nitric oxide is a powerful vasodilator that selectively acts on the vessels of the pulmonary circulation. Abroad, patients with PH are given 2–3 week courses of inhaled nitric oxide (20–40 ppm) for 5–6 hours a day. Clinical trial results suggest that inhaled nitric oxide may be an effective therapeutic option for the treatment of PH of varying severity [80, 81].
The mechanism of action of PDE-5 inhibitors is mediated through enhancing the effects of nitric oxide. By preventing the degradation of cGMP, they enhance the relaxing effect of nitric oxide on vascular smooth muscle and its antiaggregation activity, causing a decrease in pulmonary vascular resistance and overload of the right ventricle of the heart. It is possible that the beneficial effect of drugs of this group in PH may be facilitated by their pleiotropic effects. In particular, sildenafil has antioxidant properties and has an antiproliferative effect [82–84]. The results of one study suggested that sildenafil has an inotropic effect [85]. In addition to PDE-5, sildenafil inhibits PDE-1, the level of which increases in PH [86]. In addition, during treatment with sildenafil, to a greater extent than during treatment with other drugs, the level of endothelial progenitor cells increases, the number of which is reduced in idiopathic and hereditary PH [87].
Clinical studies of sildenafil involved predominantly patients with class II–III, including 71% of patients with idiopathic PH and 25% with PH associated with connective tissue diseases. When used in doses of 25–100 mg 2–3 times a day, it caused improved hemodynamics, increased exercise tolerance and improved PH functional class [88].
A number of meta-analyses have demonstrated equal effectiveness of sildenafil with prostacyclin analogues and endothelin receptor antagonists [45, 89]. According to the results of P. Steele et al., one-year survival rate with the use of sildenafil (75.2%) was comparable to that with the use of epoprostenol (78.4%), bosentan (77.8%), treprostinil (76.1%), sitaxentan (75.8%) and beraprost (74.1%) [60]. Sildenafil is indicated for the treatment of patients with PH II–III FC [1]. There is currently no data to support its use in patients with asymptomatic PH. It should also not be considered as the first choice drug for patients with severe disease (FC IV, 6-minute walk test < 100 m) [90]. The recommended dose of sildenafil, according to the instructions for medical use, is 20 mg 3 times a day, however, a long-term stable effect of the drug has been demonstrated only when using a dose of 80 mg/day. The dose limitation to 60 mg/day is due to safety concerns, since a number of the most common side effects of the drug (redness of the skin, headache, visual disturbances) are dose-dependent [88].
Sildenafil is generally well tolerated by patients with PH, including with long-term use, however, when prescribing it, the level of systemic blood pressure should be assessed, and also find out whether the patient is taking concomitant medications that can enhance its hypotensive effect (nitrates, α-blockers) .
Another PDE-5 inhibitor registered abroad for the treatment of PH is tadalafil (40 mg/day). The basis for its registration for this indication was the results of a 16-week RCT in which tadalafil in doses of 2.5 to 40 mg was compared with placebo in patients with PH [91]. The results obtained were similar to those of the SUPER-1 study, which studied sildenafil [88]. The use of tadalafil led to improved results of the 6-minute walk test at 44 m, improved hemodynamic parameters and quality of life of patients. The tolerability of tadalafil is similar to that of sildenafil.
The results of a recently published 24-week, double-blind, placebo-controlled study (n = 66) indicate that vardenafil 5 mg twice daily is also effective in PH and is well tolerated [92].
For patients who experience worsening (or no improvement) of their condition during monotherapy, experts recommend combination pharmacotherapy [1, 15]. This recommendation is based primarily on the theoretical assumption that the therapeutic effect can be enhanced by the action of drugs on different pathogenetic targets [93]. This assumption has been confirmed in a number of clinical studies, but currently available data do not allow us to definitively prove the benefits of combined therapy.
PI compared with monotherapy. According to the results of a meta-analysis of 6 RCTs (858 patients), combination therapy improves clinical and hemodynamic outcomes, but does not reduce mortality compared with monotherapy [94]. Potentially useful combinations include combining prostanoids with endothelin receptor antagonists, prostanoids with PDE5 inhibitors, and PDE5 inhibitors with endothelin receptor antagonists.
Thus, currently on the international pharmaceutical market there are quite a lot of drugs of different pharmacological groups for the treatment of PH, but the mortality of these patients remains at a high level. The search for effective and safe pharmacotherapy for PH continues. Drugs of several pharmacological classes are under development: Rho-kinase inhibitors, stimulators of soluble guanylate cyclase (riociguat, etc.), vasoactive polypeptides, serotonin transporter inhibitors, protein tyrosine kinase inhibitors (imatinib), vascular endothelial growth factor, etc. [34].
Literature
1. McLaughlin VV, Archer SL, Badesch DB, et al. ACCF/AHA 2009 Expert Consensus Document on Pulmonary Hypertension A Report of the American College of Cardiology Foundation Task Force on Expert Consensus Documents and the American. Heart Association Developed in Collaboration With the American College of Chest Physicians; American Thoracic Society, Inc.; and the Pulmonary Hypertension Association J Am Coll Cardiol. 2009 Apr 28;53(17):1573–619. 2. McLaughlin VV. Classification and epidemiology of pulmonary hypertension. J Am Coll Cardiol 2004;43(12):5S–12S. 3. Thenappan T, Shah SJ, Rich S, et al. A USA-based registry for pulmonary arterial hypertension: 1982–2006 Eur Respir J 2007;30:1103–10. 4. D'Alonzo GE, Barst RJ, Ayres SM, et al. Survival in patients with pulmonary primary hypertension. Ann Intern Med 1991;115:343–49. 5. Appelbaum L, Yigla M, Bendayan D, et al. Primary pulmonary hypertension in Israel: a national survey. Chest 2001;119(6):1801–806. 6. Sandoval J, Bauerle O, Palomar A, et al. Survival in primary pulmonary hypertension. Validation of a prognostic equation. Circulation 1994;89(4):1733–44. 7. Shapiro S, Traiger GL, Turner M, et al. Sex differences in the diagnosis, treatment, and outcome of patients with pulmonary arterial hypertension enrolled in the registry to evaluate early and long-term pulmonary arterial hypertension disease management. Chest 2012; 141(2):363–73. 8. McLaughlin VV, Davis M, Cornwell W. Pulmonary arterial hypertension. Curr Probl Cardiol 2011;36(12):461–517. 9. Frumkin LR. The Pharmacological Treatment of Pulmonary Arterial Hypertension. Pharmacol Rev 2012;1. 10. Sidorenko B.A., Preobrazhensky D.V., Batyraliev T.A., Belenkov Yu.N. Pulmonary arterial hypertension: changing approaches to treatment // Cardiology 2011. No. 51(1). pp. 100–8. 11. Herve P, Humbert M, Sitbon O, et al. Pathobiology of pulmonary hypertension: the role of platelets and thrombosis. Clin Chest Med 2001;22:451–58. 12. Hoeper MM, Sosada M, Fabel H. Plasma coagulation profiles in patients with severe primary pulmonary hypertension. Eur Respir J 1998;12:1446–49. 13. Beckmann R, Frank H, Kneussl M, et al. Fibrinogen, t-PA, and PAI-1 plasma levels in patients with pulmonary hypertension. Am J Respir Crit Care Med 1994;150:929–33. 14. Fuster V, Steele PM, Edwards WD, et al. Primary pulmonary hypertension: natural history and the importance of thrombosis. Circulation1984;70:580–87. 15. Gali N, Hoeper MM, Humbert M, et al. Guidelines for the diagnosis and treatment of pulmonary hypertension. The Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS), endorsed by the International Society of Heart and Lung Transplantation (ISHLT) Eur Heart J 2009;30(20 ):2493–537. 16. Kawut SM, Horn EM, Berekashvili KK, et al. New predictors of outcome in idiopathic pulmonary arterial hypertension. Chest 2008;134:139–45. 17. Badesch DB, Abman SH, Simonneau G, et al. Medical therapy for pulmonary arterial hypertension. Updated ACCP evidence-based clinical practice guidelines. Chest 2007;131:1917–28. 18. Chazova I.E., Martynyuk. T.V., Adeyev S.N. and others. Russian recommendations for the diagnosis and treatment of pulmonary hypertension // Cardiovascular Therapy and Prevention 2007. No. 6(6). Appendix 2. 19. Rich S, Seidlitz M, Dodin E, et al. The short-term effects of digoxin in patients with right ventricular dysfunction from pulmonary hypertension. Chest 1998;114:787–92. 20. Rich S, Kaufmann E, Levy PS. The effect of high doses of calcium-channel blockers on survival in primary pulmonary hypertension N Engl J Med 1992;327:76–81. 21. Sitbon O, Humbert M, Jais X, et al. Long-term response to calcium channel blockers in idiopathic pulmonary arterial hypertension. Circulation 2005;111:3105–11. 22. Tonelli AR, Alnuaimat H, Mubarak K. Pulmonary vasodilator testing and use of calcium channel blockers in pulmonary arterial hypertension. Respir Med 2010;104(4):481–96. 23. Mukerjee D, St George D, Coleiro B, et al. Prevalence and outcome in systemic sclerosis associated pulmonary arterial hypertension: application of a registry approach. Ann Rheum Dis 2003;62:1088–93. 24. Montani D, Savale L, Natali D, et al. Long-term response to calcium-channel blockers in non-idiopathic pulmonary arterial hypertension. Eur Heart J 2010;31(15):1898–907. 25. Humbert M, Sitbon O, Simonneau G. Treatment of pulmonary arterial hypertension. N Engl J Med 2004;351:1425–36. 26. Badesch DB, McLaughlin VV, Delcroix M, et al. Prostanoid therapy for pulmonary arterial hypertension. J Am Coll Cardiol 2004; 43(12):56S–61S. 27. Ivy DD. Prostacyclin in the intensive care setting. Pediatr Crit Care Med 2010; 11(2 Suppl.): S41–S5. 28. Barst RJ, Rubin LJ, Long WA, et al. A comparison of continuous intravenous epoprostenol (prostacyclin) with conventional therapy for primary pulmonary hypertension. The Primary Pulmonary Hypertension Study Group. N Engl J Med 1996;334:296–302. 29. Sitbon OHM, Nunes H, Parent F, et al. Long-term intravenous epoprostenol infusion in primary pulmonary hypertension: Prognostic factors and survival. J Am Coll Cardiol 2002;40:780–88. 30. Chen YF, Jowett S, Barton P, et al. Clinical and cost-effectiveness of epoprostenol, iloprost, bosentan, sitaxentan and sildenafil for pulmonary arterial hypertension within their licensed indications: a systematic review and economic evaluation. Health Technol Assess 2009;13(49):1–320.
About the authors / For correspondence
Ushkalova E.A. – Doctor of Medical Sciences, Prof. Department of General and Clinical Pharmacology of RUDN University. Leading researcher of the therapeutic department of the Federal State Budgetary Institution “Scientific Center of Obstetrics, Gynecology and Perinatology named after. IN AND. Kulakova”, E-mail; Runikhina N.K. – Doctor of Medical Sciences, Head. therapeutic department of the Federal State Budgetary Institution “Scientific Center of Obstetrics, Gynecology and Perinatology named after. IN AND. Kulakov” of the Ministry of Health and Social Development of the Russian Federation. Email: [email protected] ; Novikova I.M. – Candidate of Medical Sciences, senior researcher of the therapeutic department of the Federal State Budgetary Institution “Scientific Center of Obstetrics, Gynecology and Perinatology named after. them. IN AND. Kulakov” of the Ministry of Health and Social Development of the Russian Federation.
Similar articles
- Pulmonary hypertension: current issues of diagnosis and treatment
- Secondary pulmonary hypertension in a child with concomitant cardiorespiratory pathology (clinical case)
- Principles of rational perioperative pharmacotherapy in patients with congenital heart defects complicated by pulmonary hypertension
- Riociguat is a new drug for the treatment of pulmonary hypertension.
- Drug therapy for patients with pulmonary hypertension: a look into the future
Is cardiac echocardiography safe?
During this study, there is no radiation or other load on the organ. Therefore, if necessary, it can be prescribed even several times a week.
This study is characterized by the absence of complications and side effects.
EchoCG does not harm either the expectant mother or the fetus during pregnancy.
Limitations for the procedure may include inflammatory diseases of the skin of the chest, chest deformities and some other reasons.
How to do an ultrasound of the heart at the MedicCity clinic?
It is advisable for every person to have an echocardiogram at least once in their life. The fairly low cost of cardiac ultrasound is another reason to prefer this particular diagnostic method.
At MedicCity you can undergo all types of cardiac diagnostics - ECG, EchoCG, bicycle ergometry, HOLTER, ABPM, etc.
Just type in a search engine: “Ultrasound of the heart, Savelovskaya metro station, Dynamo metro station.” Or call us at: +7 (495) 604-12-12.
The doctors of our multidisciplinary clinic will do everything possible to relieve your heart pain!