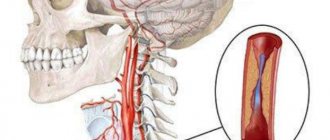
Pathological tortuosity (kinking) of the carotid arteries is one of the least studied and mysterious diseases. The role of pathological tortuosity in the development of symptoms of cerebrovascular insufficiency is still being studied, but it has been established that every third person who died from a stroke had pathological bends of the carotid or vertebral arteries. In 16-26% of the adult population, various variants of elongation and tortuosity of the carotid or vertebral arteries in the neck are detected. Pathological tortuosity is the uneven course of an artery with the formation of bends, loops and twists, which affects the nature of blood flow through the artery and can contribute to the development of acute cerebrovascular accidents.
Treatment methods at the Innovative Vascular Center
The vascular surgeons of our clinic have significant experience in unique operations on the carotid arteries with pathological tortuosity. The main problem for surgical treatment is determining clear indications for surgical treatment. Our clinic has developed a clear diagnostic protocol that allows us to determine the clinical significance of a particular tortuosity and the degree of its effect on cerebral blood flow. The experience of successful operations in our clinic for pathological tortuosity exceeds 200 cases.
Surgical treatment and prevention of cerebral ischemia of extraranial origin
4.6 / 5 ( 5 votes)
"Surgical prevention of ischemic stroke in patients with diseases of the main arteries of the head and neck"
Introduction Vascular diseases of the brain are a pressing medical and social problem. Every year more than 6 million people suffer a stroke in the world, of which 400-450 thousand are registered only in Russia. Stroke is the absolute leading cause of disability in the population. Of all acute cerebrovascular accidents, 70% are ischemic stroke. In economically developed countries, a similar situation was observed several decades ago, but due to the implementation of preventive measures against atherosclerosis on a national scale in these countries, the situation has changed radically - mortality from cardiovascular causes has decreased by 2 times or more, and the average life expectancy of the population has sharply increased.
In population studies, about 50% of ischemic episodes, both permanent and temporary, are thrombotic or embolic complications of atherosclerosis of large and medium-sized arteries, about 25% are associated with diseases of small-diameter intracranial vessels, about 20% are associated with embolism from the heart, and the remaining 5% of episodes are associated with rarer causes (artery dissection, arteritis, blood diseases leading to hypercoagulability syndrome, etc.). Atherosclerotic lesions of arteries of large and medium diameter, appearing to be the most common cause of ischemic episodes, are the most significant object of surgical intervention or drug treatment aimed at preventing possible ischemic cerebral catastrophes.
Pathogenesis of atherothrombotic stroke.
Atheromatous plaques primarily affect large (aortic arch) and medium-sized arteries, especially at sites of division (bifurcation of the common carotid artery), tortuosity (siphon of the internal carotid artery (ICA)) or confluence (basic artery (BA). Intracranial arteries (distal to the circle of Willis ) suffer from atherosclerosis extremely rarely, in connection with this, occlusions of these arteries occur due to embolism more often than due to local thrombosis at the site of the atheromatous plaque. This distribution of atherosclerotic plaques is probably determined by the sites of hemodynamic stress and endothelial injury, border zones of separation flow and stagnation of blood and turbulence, which can cause thrombus formation, which in itself leads to the progression of atheromatous lesions. From the early stages of their formation, plaques are complicated by adhesion, activation and aggregation of platelets, which triggers coagulation and mural thrombosis. Atherothrombotic plaque can grow and clog the lumen arteries, then the thrombus in the arterial lumen spreads proximally or distally, the thrombus can undergo lysis through fibrinolytic mechanisms of the vascular wall and blood. The thrombus, or part of it, can become an embolus, leading to occlusion of the distal arteries. Thus, emboli are composed of a combination of cholesterol, platelet aggregates, and fibrin. Depending on their composition, size, density, and age, emboli may be lysed, fragmented, or continue to occlude the distal artery and possibly trigger local anterograde and retrograde thrombosis. It is likely that the nature and speed of local blood flow determine to some extent the fate of emboli. Whether cerebral infarction occurs or not depends on the adequacy of collateral blood flow. Emboli are transported to the brain or eye along the normal arterial blood supply, which itself varies from person to person. Thus, an embolus formed in the ICA usually enters the eye or the anterior two-thirds of the cerebral hemisphere, but can enter the occipital lobe through the posterior communicating artery (PCoA). Emboli can appear in more unusual places (for example, with severe damage to the vertebral arteries (VA) and low blood flow in the OA, an embolus formed in the ICA can reach the OA through the circle of Willis). The embolus may end up in the opposite hemisphere, reaching the latter through the anterior communicating artery (ACOA). Other “exotic” variants of embolic migration are also possible. Finally, ischemic stroke on the side of the occluded ICA may result from slow blood flow in the area of its supply or in the border zone, especially if the collateral blood supply is insufficient. Atherosclerotic damage to the arteries may not produce obvious clinical symptoms, nevertheless causing an undoubted danger of developing cerebral ischemic episodes in the future. According to these clinical features, patients with atherosclerosis of the main arteries of the head are conventionally divided into symptomatic and asymptomatic, respectively.
Carotid endarterectomy or drug prophylaxis? The first successful endarterectomy was performed in the USA in 1953. In subsequent decades, indications for carotid endarterectomy (CEA) have steadily expanded, and the number of operations performed has grown rapidly. For example, in 1985, the indications for performing CEA in the USA were as follows:
1. hemispheric TIA 2. transient monocular blindness 3. vertebrobasilar insufficiency 4. general hypoperfusion 5. stroke with minimal residual deficit 6. lesion or combination of lesions predisposing to stroke
The latter indication was, of course, a euphemism for asymptomatic carotid stenosis. Nonstenotic but severely ulcerated plaques at the carotid bifurcation in both symptomatic and asymptomatic patients have also been considered by many leading surgeons as a suitable indication for surgical treatment. At that time, the evaluation of virtually every patient candidate for CEA included conventional angiography, but standards for measuring the percentage of narrowing or diameter were not developed. It was widely believed that a 50% narrowing of the diameter resulted in a hemodynamically and therefore clinically significant effect predisposing to the development of stroke, thus amenable to surgical removal. In addition, most, if not all, surgeons accepted the premise that the risk of intraoperative hypotension in the presence of carotid stenosis was a particularly dangerous combination. As a result, asymptomatic carotid disease has been considered and treated prophylactically in patients undergoing cardiac or abdominal aortic surgery. With these indications, by 1985, CEA had become the most common peripheral vascular procedure performed in the United States, with more than 107,000 CEA performed at nonfederal medical centers that year. In the 60s of the last century, neurosurgeons at the N.V. Sklifosovsky Research Institute for Emergency Medicine were actively involved in the problem of diagnosis and surgical treatment of stenotic lesions of the main arteries of the head. This huge and steadily expanding number of operations has not escaped the attention of many leading neurologists. Articles began to appear on the effectiveness and safety of carotid surgeries in general and in asymptomatic patients in particular. Several significant reports highlighted potential flaws in presentations that supported the generally accepted indications for CEA. An important publication on this topic was Brott and Thalinger's review of all CEAs performed in Cincinnati, Ohio in 1984. They found an unexpectedly high operative morbidity and mortality rate (9.5%) and argued that these surgical outcomes are likely to be typical throughout the country, and if so, is there any benefit to CEA at all? Such concerns led to the design, initiation, and eventual execution of several randomized prospective clinical trials comparing the results of CEA with the best medical treatment available at the time in symptomatic and asymptomatic patients. Seven large studies conducted in North America and Europe included three in symptomatic patients and four in asymptomatic patients. All studies were multicenter, prospective, and randomized, but had different patient inclusion and exclusion criteria, different methods for measuring the degree of stenosis, and different methods for reporting results. Despite these differences, there was strong agreement in the important outcomes of all symptomatic studies and three of the four asymptomatic studies.
Large multicenter randomized prospective studies were devoted to comparison of the effectiveness of conservative and surgical prevention of ischemic stroke in patients with symptomatic carotid stenoses: North American Symptomatic Carotid Endarterectomy Trial (NASCET) and European Carotid Surgery Trial (ECST), etc. The mentioned studies compared the effectiveness of isolated conservative prevention with a combination of “surgical prevention + conservative prevention” in patients with varying degrees of carotid stenosis. Since quantitative indicators of carotid damage have become the main factor in the selection of patients for surgical treatment, before moving on to a brief description of the studies and their results, it is very important to discuss methods for measuring the degree of stenosis. The American method differs significantly from the European method. The American method was used with the Extracranial Arterial Occlusive Disease Study in the 1950s and continued to be used in the Veterans Administration (VA) Asymptomatic Trial, NASCET, and Asymptomatic Carotid Atherosclerosis Trial (ACAS). The method involves measuring the diameter of the lumen at the site of greatest stenosis (A) on angiography and comparing it with the diameter of the ICA distal to the stenosis, at the point where the walls of the ICA become parallel (B).
the degree of stenosis according to the European method involves presenting the hypothetical boundaries of the ICA bulb, the diameter of which (C) is normally greater than the lumen of the ICA. The degree of stenosis is calculated using the formula:
(1 – A/C)x100
The difference in numbers for the same stenosis is most pronounced with low degrees of stenosis and becomes minimal with severe stenosis.
This difference is presented in the table:
Randomized trials on the prevention of ischemic stroke in symptomatic patients. NASCET
The study was designed to test the hypothesis that symptomatic patients (with hemispheric or monocular TIAs or previous minor strokes) with ipsilateral carotid stenosis (30-99% by NASCET) would experience fewer fatal and nonfatal strokes after CEA and medical treatment than patients after isolated drug treatment. It was planned to enroll 3000 patients in the study and follow them for 5 years. Patients were divided into groups of severe (70-99%) and moderate (30-69%) stenoses. In the group of patients with severe stenoses, the study ended early: the cumulative two-year risk of any ipsilateral stroke in the medical group was 26%, and in the surgical group it was 9% (including perioperative surgical risk of stroke). The absolute risk reduction was 17% and the relative risk reduction was 65%. The risk of mortality in the groups was 12% and 5%, respectively. The relative reduction in mortality risk was 58%.
Effect of carotid endarterectomy on reducing the risk of stroke or death according to NASCET results
Patients with moderate stenoses (50-69%) showed a small but statistically significant benefit of CEA, while patients with minor stenoses (30-49%) showed no benefit of CEA. This overwhelming advantage in the group of severe stenoses was made possible due to the relatively low risk of surgery. Thus, the 30-day rate of “death + stroke” was 5.8%. It was also noted that the risk of stroke in the drug group was higher for every 10% increase in the degree of stenosis from 70 to 99. It was then noted that retinal TIAs had a less dire prognosis than hemispheric TIAs in the drug control group. So the probability of developing a stroke within 2 years in the group of “retinal” patients was 17%, and in the group of “hemispheric” patients - 44%. It was also noted that the presence of contralateral occlusion significantly worsened the prognosis of patients in the drug group. At two-year follow-up, 54.6% of such patients in the medical group suffered a stroke or died, while the same figure was only 20% in the surgical group. Patients enrolled in the study with a history of TIA but who had infarcts detected on brain CT showed an increased risk of developing ipsilateral stroke during follow-up (26% vs. 13%). In subsequent publications, NASCET investigators noted that the presence of plaque ulceration on angiography seriously complicates prognosis. Thus, the two-year risk of stroke in “medicated” patients with an ulcerated plaque increased from 26.3% to 73.2% with an increase in the degree of stenosis from 70% to 99%. Interestingly, the risk in patients without ulceration was 21.3%, regardless of the degree of stenosis. In addition, the operative risk did not change significantly in patients with and without ulceration. In February 1998, NASCET investigators reported results for patients with moderate stenoses. From the report it became clear that patients with 50-69% stenoses are preferable to undergo CEA (based on 5-year follow-up results). However, the difference, although statistically significant, was not as dramatic as in the severe stenosis group. In addition, the surgical risk in this group was higher and amounted to 6.7%. ECST Initiated in 1981, this randomized prospective study was conducted under the auspices of the Medical Research Council of GB. Patients were divided into three categories of stenosis: 0-29%, 30-69% and 70-99%, measured according to the European method. Overall, the 3-year risk of stroke in patients with severe stenosis (70-99%) was 21.9% in patients receiving medical therapy and 12.3% in patients after CEA. The absolute reduction in stroke risk was 9.6% and the relative reduction was 56%.
Three-year risk of stroke in the drug prevention group in patients with severe carotid stenosis:
In 1991, researchers reported their preliminary results, which coincided with the American ones. In the small stenosis group, the risk of stroke was small, and patients were recommended to undergo drug treatment. In the group of severe stenoses, despite the 30-day surgical risk of 7.5%, there was a six-fold reduction in the risk of stroke when using the surgical method of treatment. For 778 patients randomized to the severe stenosis group, CEA virtually eliminated the risk of ipsilateral stroke during follow-up. The table details the average annual risk of ipsilateral ischemic stroke following successful CEA.
In 1996, European researchers reported the results of an observation of a group with moderate stenoses. There was no significant advantage of the surgical treatment method. However, we should not forget about the significant difference between the methods for measuring the degree of stenosis between Europe and the USA.
Thus, both studies, although differing in tactical details, were unanimous in their strategic conclusions: with severe symptomatic stenoses, surgical prevention of ischemic stroke has undoubted (p
NASCET found a clear association between the number of risk factors and the rate of late stroke in the group of patients treated conservatively. A similar but less pronounced association was demonstrated in asymptomatic arteries.
ACST ACST is a more modern (and to date the largest) randomized trial on the choice of method for the prevention of ischemic stroke in asymptomatic patients. It was initiated and led by the Medical Research Council and the UK Stroke Association. 3120 patients with carotid stenosis ≥60% were randomized to surgery (50% CEA performed within 1 month, 88% within 1 year) or medical group. The average follow-up period was 3.4 years. Exclusion criteria were: high risk of surgical intervention, previously performed ipsilateral CEA, suspected cardiac embolism. The 5-year risk of stroke (including perioperative stroke) was 6.4% in the surgical group and 11.8% in the medical group. Risk rate for fatal or disabling stroke: 3.5% and 6.1%, respectively. Risk rate for fatal stroke: 2.1% and 4.2%, respectively. Two features were also revealed: the benefits of surgical prophylaxis were more pronounced in men; there was no statistically significant advantage of the surgical method of prevention in patients over 75 years of age. Thus, the results of ACAS and ACST revealed a significant (although less pronounced than in symptomatic patients) benefit of surgical prophylaxis in patients with asymptomatic carotid stenoses of 60-99%.
The nature of the atherosclerotic plaque is also a significant factor: heterogeneous, hypoechoic plaques increase the patient's risk of stroke.
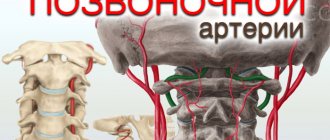
Pathological tortuosity of the main arteries of the head. Acute and chronic cerebral circulatory failure can be caused not only by atherosclerotic stenosis, but also by the presence of kinks and loops of the internal carotid and (or) vertebral arteries. According to pathological studies, severe tortuosity of the carotid arteries was found in 30% of patients who died from ischemic stroke 1. Tortuosity of the carotid or vertebral artery with impaired blood flow and symptoms of acute or chronic cerebrovascular accident in the corresponding vascular area is considered pathological 2. Form of lengthening - Tortuosity - there are C and S-shaped bends of the arteries - Kinking - there are bends of the elongated arteries at an acute angle (angulation) - Coiling - there is elongation of the arteries in the form of loops and spirals. 3. Characteristics of bends - Without reducing the lumen - With a narrowing of the lumen at the bend - With the formation of partitions
A change in the course of the artery leads to noticeable hydrodynamic and hemodynamic disturbances: 1. In a bend, the local blood pressure at the artery section is minimal on the inner wall of the bend, progressively increases and reaches a maximum on the outer wall of the artery bend. 2. In inverse proportion to local pressure, the local speed of blood flow also changes (minimum at the outer radius and maximum at the inner radius). 3. Due to the difference in pressure (at the outer and inner radius), stable secondary flows of transverse and counter blood circulation arise, having the nature of a vortex. 4. A sharp sudden increase in pressure (especially during a hypertensive crisis) can lead to hydrodynamic blockage in the bend area. 5. The total energy losses during artery tortuosity are significant and, accordingly, increase with echelon tortuosities (the so-called S or Z-shaped tortuosities).
Conclusion.
Thus, today, carotid endarterectomy is indicated for patients with carotid stenoses of 70-99%. 1. asymptomatic patients with carotid stenosis of 60-99% 2. symptomatic patients with stenosis of the internal carotid artery more than 50%, tortuosity of the vertebral arteries, pathological tortuosity of the carotid arteries.
Indications for surgical treatment of pathological tortuosity of the brachiocephalic and vertebral arteries: 1. ischemic stroke or TIA in the territory of the tortuous artery; 2. CNM in the absence of the effect of conservative therapy and a decrease in the patient’s quality of life; 3. asymptomatic tortuosity in the presence of focal changes on CT scan of the brain; 4. stenosis > 60% at the site of artery bending and loop formation. 5. The difference in blood flow velocity in the tortuosity zone is 2 or more times according to Doppler ultrasound.
Indications for the operation of extra-intracranial microanastomosis (EICMA): 1. Occlusion of the carotid artery with a clinical picture of depletion of the cerebral perfusion reserve and decompensation of collateral circulation, manifested by transient ischemic attacks in the basin of the occluded internal carotid artery. 2. Hemodynamically significant stenosis of the middle cerebral artery and tandem stenoses. 3. As the first stage of surgical treatment before CEA for occlusion of the contralateral carotid artery.
Indications for reconstruction of the vertebral artery.
1. Patients with symptoms of unstable hemodynamics in the vertebrobasilar region: - With stenosis of the dominant vertebral artery more than 75%. - With a stenotic process of the same degree of stenosis of both vertebral arteries. — In case of segmental occlusion of the second segment of the vertebral artery in the presence of hypoplasia of the other. 2. Patients with a clinical picture of stem dyscirculation of thromboembolic origin, in which the source of the embolism from the vertebral artery has been identified. 3. With extravasal compression significantly affecting vertebral blood flow (cervical rib, Kimmerly's anomaly, uncovertebral arthrosis and other spondylogenic causes).
Methodology for carotid endarterectomy surgery.
At the moment, there are two main methods of performing carotid endarterectomy: 1. Classic carotid endarterectomy with the possible use of lateral expansion patch angioplasty. 2. Eversion carotid endarterectomy.
The use of one or another technique often depends on the personal preferences of the operating surgeon, but in some conditions each method has its own advantages and is most preferable in a particular clinical situation.
Classic carotid endarterectomy is most often performed for:
1. When the atherosclerotic plaque is localized in the common carotid artery, its bifurcation and at the mouth of the internal carotid artery without prolongation of the plaque to the proximal and middle third of the internal carotid artery. 2. If the diameter of the internal carotid artery is sufficient (4-5 mm), otherwise, without using an expanding patch, there is a high probability of postoperative restenosis of the internal carotid artery, which is most important in women. 3. With a high location of the bifurcation of the common carotid artery. 4. During classical carotid endarterectomy, arteriolysis along the posterior surface of the carotid group and removal of the carotid body are not required, which significantly reduces the duration of the operation and the risk of damage to the vessels located behind the internal and common carotid arteries - the ascending pharyngeal and carotid body arteries.
Eversion carotid endarterectomy is preferred:
1. In the presence of concomitant pathological tortuosity of the internal carotid artery, when, simultaneously with carotid endarterectomy, it is possible to perform redressing of the internal carotid artery with its reimplantation into the “former” mouth or a new mouth on the common carotid artery. 2. In the case of a prolonged atherosclerotic plaque, with its spread above the mouth of the internal carotid artery. 3. With a “narrow” internal carotid artery (diameter less than 3-4 mm) and a high risk of using an expanding lateral patch (patch suppuration in patients with diabetes mellitus).
Conditions for performing carotid endarterectomy surgery.
Most operations are performed under multicomponent endotracheal anesthesia, which significantly increases the body's resistance to hypoxia, and moderate controlled arterial hypertension is also used for this purpose. After clamping the carotid, blood pressure rises by an average of 20 mm. RT. Art. and equals approximately 140-160/90 mmHg. Systemic heparinization protects against thrombus formation in compressed arteries and reduces intraoperative embolism. The amount of heparin is administered at the rate of 100 U/kg of patient weight.
Scheme of the operation of classical carotid endaretrectomy.
Position the patient on his back with his head turned in the direction opposite to the operation. The incision line is projected along the anterior edge of the sternocleidomastoid muscle, starting from the mastoid process and ending 1-2 cm distal to the jugular notch. The skin, subcutaneous fascia, and subcutaneous muscle are dissected in layers. On the access route, the external jugular vein may be encountered, which is ligated and divided. The anterior edge of the sternocleidomastoid muscle is mobilized and retracted laterally using an Anderson-Edson retractor. As you move deeper into the wound, the lateral branch of the retractor is also inserted deeper, but the medial branch should not be deepened or moved, which can cause damage to the cartilage of the larynx. Immediately below the sternocleidomastoid muscle is the internal jugular vein with the common facial vein branching off from it - the key to the bifurcation of the common carotid artery. The common facial vein is divided and sutured, after which the internal jugular vein becomes mobile and is easily retracted externally. At this point, it is necessary to perform systemic heparinization and begin skeletonization of the carotid arteries. It is easiest to start from the lower corner of the wound, where the Common Carotid Artery is located. The carotid artery sheath is opened and dissection is performed in the longitudinal direction, which is safe. When approaching the bifurcation of the CCA, it is necessary to work with dissecting scissors in the longitudinal direction so as not to roughly impact the arterial wall and not cause intraoperative microembolism from the surface of the unstable atherosclerotic plaque. As the arteries are isolated, the common carotid, internal carotid, external carotid and superior thyroid arteries are taken onto holders made of thin braid. The boundaries of the spread of the atherosclerotic plaque are visually determined; the internal carotid artery must be skeletonized distally 1 cm from the upper border of the atherosclerotic plaque.
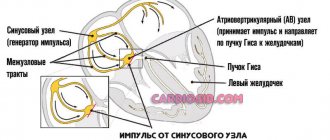
Next, a test is performed with clamping of the internal external and common carotid arteries, during which blood flow through the homolateral middle cerebral artery is recorded using transcranial Dopplerography. If the blood flow velocity does not decrease by more than 60% of the initial value and does not become less than 20 cm/sec, then it is possible to perform the operation without temporary intraluminal shunting. Otherwise, a shunt is used. The superior thyroid, internal carotid, common carotid and external carotid arteries are sequentially clamped. A linear arteriotomy is performed starting from the common carotid artery, in the bifurcation area to the bulb of the internal carotid artery.
The atherosclerotic plaque is visualized, its boundaries are determined, and it is peeled off from the unchanged arterial wall. It is sequentially separated, first in the proximal sections, from the mouth of the superior thyroid artery, from the external carotid and finally from the internal carotid artery, the plaque in it “disappears.” Remains of intima, cholesterol and calcium are removed, and the artery is washed with solutions.
Then they begin to apply a continuous wrapping suture using Prolene 6-0 thread. When suturing the internal carotid artery, it is necessary to retreat 0.7-1 mm from the edge of the incision and each subsequent needle injection should be made after 1 mm; as you approach the common carotid artery, you can “roughly grab” the arterial wall into the suture, because The diameter of the common carotid artery is quite large and restenosis in this location is rare.
After the arteriotomy opening is almost completely sutured, it is necessary to flush the artery lumen, check retrograde blood flow from the internal and external carotid arteries, orthograde blood flow from the common carotid artery, to remove blood clots and intimal debris.
Clamps are applied to the arteries again and the vascular suture is completed. The blood flow velocity in the homolateral middle cerebral artery is monitored using transcranial Doppler sonography. I remove the clamps in the following order. First, from the superior thyroid artery, then from the external carotid artery, then from the common carotid artery (possible thrombotic and atheromatous masses enter the basin of the external carotid artery) and finally remove the clamp from the internal carotid artery.
The operation is completed by sequential suturing of the vascular sheath, subcutaneous muscle and tissue, and skin. To control bleeding, a Redon drain is left in the intermuscular space.
The article was prepared using materials from the methodological recommendations (No. 44) of the Moscow Department of Health 2008 “Surgical prevention of cerebrovascular accidents of extracranial origin.”
Compiled by V.V. Krylov, E.I. Gusev, V.L. Lemenev, A.V. Vorobyov, O.Yu. Nakhabin and others. Author of the article: neurosurgeon Anton Viktorovich Vorobiev Frame around the text
Why choose us:
- we will offer the most optimal treatment method;
- we have extensive experience in treating major neurosurgical diseases;
- We have polite and attentive staff;
- Get qualified advice on your problem.
Causes and prevalence of pathological tortuosity
Pathological tortuosity always develops due to the elongation of the internal carotid artery, which is forced to fold into bends or even loops. Excessive length of the internal carotid artery is often formed during embryonic development, that is, the tortuosity of the artery is most often congenital. With age, further twisting of the redundant carotid artery into a loop may occur. According to some researchers, pathological tortuosity may be the cause of neurological and intellectual problems in children of preschool and primary school age.
Lengthening of the internal carotid artery can also develop as a result of advanced hypertension, when constantly elevated blood pressure causes changes in the artery wall and its bends. Such tortuosity rarely affects cerebral hemodynamics and is more often a phenomenon detected incidentally by ultrasound of the great arteries.
Pathological tortuosity of the carotid arteries was detected in 16% of patients who died from ischemic stroke; more than 23% of children who suffered an ischemic stroke had pathological tortuosity. When examining patients undergoing treatment for cerebrovascular accidents, pathological tortuosity was detected by ultrasound angioscanning in 12%. Various disorders of the internal carotid arteries, according to pathological studies, were identified in 40% of people.
Diagnostics
Diagnosis of vertebral artery syndrome presents certain difficulties and both overdiagnosis and underdiagnosis of vertebral artery syndrome often occur. Overdiagnosis of the syndrome is often due to insufficient examination of patients, especially in the presence of vestibulo-atactic and/or cochlear syndrome, when the doctor fails to diagnose diseases of the labyrinth.
To establish a diagnosis of vertebral artery syndrome, 3 criteria must be present.
- The presence in the clinic of symptoms of one of 9 clinical options or a combination of options
- Visualization of morphological changes in the cervical spine using MRI or MSCT, which may be the main reasons for the development of this syndrome.
- The presence of changes in blood flow during ultrasound examination when performing functional tests with flexion - extension of the head and rotation of the head.
Clinical and anatomical options
Lengthening the artery. The most common is elongation of the internal carotid or vertebral artery, which leads to the formation of smooth bends along the course of the vessel. An elongated artery is rarely a cause of concern and is usually discovered during random examination. Lengthening the artery is important for ENT doctors, since the artery wall may be abnormally close to the palatine tonsils and may be accidentally damaged during tonsillectomy. With age, the elasticity of the arterial wall changes and smooth bends of the artery can become kinks, with the development of a picture of cerebral circulation disorders. When arteries are lengthened without kinks, ultrasound examination of blood flow does not detect any disturbances.
Kinking is a bend in an artery at an acute angle. Kinking can be congenital, when cerebral circulation disorders are detected from early childhood and develop over time from an elongated carotid artery. The formation of kinks is promoted by arterial hypertension and the progression of atherosclerosis in the internal carotid artery. Clinically, kinking of the internal carotid artery is manifested by transient disturbances of cerebral circulation. With kinking of the vertebral artery, vertebrobasilar insufficiency develops. Identification of kinking with brain symptoms raises the question of surgical correction of tortuosity.
Coiling is the formation of a loop of an artery. Despite the smooth movement of the loop, changes in blood flow in it are very significant. The nature of the bends during coiling may change depending on body position and blood pressure. A chaotic nature of the blood flow is observed, which leads to a decrease in blood pressure after the loop and, accordingly, to a decrease in blood flow through the cerebral arteries. If a person has a well-developed circle of Willis on the lower surface of the brain, then he will never know about the existence of a loop or inflection. The appearance of symptoms of cerebral circulatory failure indicates disturbances in blood flow compensation and dictates the need for detailed examination and treatment.
Treatment
Treatment of vertebral (vertebral) artery syndrome consists of two main areas: improving hemodynamics and treating diseases that lead to compression of the vertebral arteries.
Drug treatment
Anti-inflammatory and decongestant therapy is aimed at reducing perivascular edema resulting from mechanical compression. Drugs that regulate venous outflow (troxerutin, ginkgo biloba, diosmin). NSAIDs (Celebrex, lornoxicam, celecoxib)
Vascular therapy is aimed at improving blood circulation in the brain, since hemodynamic disturbances occur in 100% of patients with this syndrome. Modern diagnostic methods make it possible to evaluate the effectiveness of treatment with these drugs and the dynamics of blood flow in the vessels of the brain using ultrasound examination. The following drugs are used for vascular therapy: purine derivatives (trental), vinca derivatives (vincamine, vinpocetine), calcium antagonists (nimodipine), alpha-blockers (nicergoline), instenon sermion.
Neuroprotective therapy
One of the most modern areas of drug treatment is the use of drugs to improve energetic processes in the brain, which allows minimizing neuronal damage due to episodic circulatory disorders. Neuroprotectors include: cholinergic drugs (citicoline, gliatiline), drugs that improve regeneration (Actovegin, Cerebrolysin), nootropics (piracetam, Mexidol), metabolic therapy (mildronate, Thiotriazoline, Trimetazidine)
Symptomatic therapy includes the use of drugs such as muscle relaxants, antimigraine drugs, antihistamines and others.
Treatment of degenerative diseases includes non-drug treatment methods, such as exercise therapy, physiotherapy, massage, acupuncture, and manual therapy.
In most cases, the use of complex treatment, including both drug and non-drug treatment, can reduce symptoms and improve blood circulation in the brain.
Surgical treatment methods are used in cases where there is severe compression of the arteries (disc herniation, osteophyte) and only surgical decompression can achieve a clinical result.
Course of the disease
If tortuosity of the carotid artery becomes symptomatic, then it is quite painful for the patient. Minor signs and symptoms of the disease gradually intensify and lead to decreased ability to work. The presence of pathological tortuosity can lead to symptomatic hypertension, which in turn contributes to the progression of tortuosity and the formation of kinks. In places where the carotid artery is bent, adhesions can form, which further disrupts the nature of blood flow, making it turbulent. Ultimately, these processes can lead to transient ischemic attacks or stroke.
Symptoms
The symptoms of pathological tortuosity of the carotid and vertebral arteries are varied. The most common symptoms are:
- so-called transient ischemic attacks (temporary interruptions in blood supply), accompanied by temporary paralysis of the upper limbs, speech impairment, temporary blindness;
- noise in the head, dizziness;
- migraine attacks;
- impaired coordination of movements, falls without loss of consciousness;
- short fainting spells.
How to treat?
If you have non-straightness of the vertebral arteries, treatment depends on the severity of the symptoms. In the early stages, conservative treatment can also help. It is necessary to figure out what caused the pathology and first cure the underlying disease. If the cause of this pathology is a spasm of the cervical muscles, it needs to be removed. Physical therapy or massage may help. Conservative treatment did not help? Then the doctor prescribes surgery.
Drug treatment
The doctor also decides which medications to prescribe, but most often drugs that improve venous outflow, painkillers, pills that lower blood pressure, etc. are prescribed. Such treatment cannot solve the problem itself, i.e. correct changes in the vessel, but it improves the patient’s well-being.
Surgical
The operation is prescribed if the doctor fears that the patient will have an ischemic stroke. The surgeon decides what exactly needs to be done. Sometimes he shortens and straightens the artery, sometimes he performs prosthetics or stenting.