Types Myocardial infarction Acute myocardial infarction Extensive myocardial infarction Cerebral infarction Transmural myocardial infarction Symptoms and signs of infarction First aid for a heart attack Treatment Clinical recommendations Consequences of a heart attack Rehabilitation and recovery after a heart attack Recommendations for exercise therapy Rehabilitation in a clinic Rehabilitation at home Help with a breathing simulator "SAMOZDRAV" in rehabilitation Disability after a heart attack Diet Breathing exercises after a heart attack Prevention of heart attack Heart attack is one of the main causes of death in most countries of the world. A third of cases of acute myocardial infarction are fatal, and a fifth of sudden deaths are associated with a heart attack.
Myocardial infarction is a severe, acute manifestation of cardiac ischemia associated with a lack of blood supply to the heart muscle (myocardium). As a result, cardiac muscle cells die, forming a focus of necrosis.
Kinds
Medicine broadly classifies heart attacks depending on different criteria. Thus, according to the size of the affected muscle tissue, the infarction can be small-focal (one or several small foci of necrosis) and large-focal (extensive necrotic lesion).
According to the depth of the necrotic focus, the infarction can be transmural (the necrotic area is formed in the area of the entire heart muscle), subepicardial (the necrotic area is located near the epicardium), subendocardial (necrosis is formed adjacent to the endocardium) and intramural (the lesion is formed in the left ventricle).
A heart attack can be:
- primary,
- repeated,
- recurrent.
The latter appears during the period of muscle scarring after the primary infarction. Depending on the development of complications, they speak of uncomplicated and complicated heart attack.
The periods of illness during a heart attack are divided into acute, acute, subacute, post-infarction.
Myocardial infarction
Myocardial infarction is damage to the middle layer of the heart muscle (myocardium). It is divided into several stages, the first of which is angina. Acute ischemia of the heart vessels refers to the most acute stage of myocardial infarction; the acute period is characterized by the formation of a necrotic area. In the subacute period, preparation for the formation of a scar in the affected area occurs; in the post-infarction state, a scar of the heart muscle is formed.
The stage of scar formation is not reversible; it is impossible to restore myocardial cells and avoid necrotic damage. After the disease, the affected area of the muscle does not participate in the contraction of the heart muscle.
Cardiomyocytes (heart muscle cells hit by a heart attack) die within 24 hours after the most acute stage of the disease. After 24 hours, the affected area can be clearly seen. After two weeks, the formation of connective tissue at the site of necrosis begins. It takes about two months for the scars to fully form.
Acute myocardial infarction
The main symptom of acute myocardial infarction is sharp chest pain, similar to severe squeezing. It differs from an attack of angina in that it is not controlled by medications and lasts more than 15 minutes. Pain extends to:
- spatula,
- neck,
- left shoulder,
- left hand,
- lower jaw.
The patient may lose consciousness. With atypical localization, the pain may be in the abdomen or spine.
An acute heart attack can be “prevented” by chest discomfort, weakness, and dizziness that occurs several days in advance.
In some cases, a heart attack may not cause severe pain. Tachycardia, weakness, nausea, general deterioration in health can become signs of an acute heart attack.
Extensive myocardial infarction
Extensive myocardial infarction is a large and deep lesion of the middle layer of the heart muscle. Due to the fact that the left ventricle of the heart bears a large load during cardiac contraction (it is from it that blood exits into the aorta under high pressure), a large infarction most often occurs in this part of the heart. At the same time, the atria and right ventricle can also be subject to extensive infarction.
The epicardium, myocardium and endocardium - layers of the heart muscle - with an extensive infarction experience deep damage, up to 7 cm in length. Like any heart attack, extensive damage to the heart muscle is a consequence of insufficient oxygen supply to the myocardium, resulting from the filling of the lumen of blood vessels with blood clots. The formation of a blood clot, in turn, provokes a new vasospasm. Such a “vicious circle” leads to blockage of the artery and a sharp limitation in the supply of oxygen to the heart muscle due to poor circulation. After circulatory arrest, myocardial cells begin to die within half an hour; a few hours after the artery is “blocked,” an extensive heart attack develops.
Brain infarction
A cerebral infarction, known as an ischemic stroke, develops against the background of impaired blood circulation in the brain and the supply of oxygen to its cells. Its causes, as well as heart attack, should be sought in increased thrombus formation and damage to vital vessels.
Therefore, the main task during a cerebral infarction is to restore blood flow through the thrombosed artery, minimize the risks of developing cerebral edema and convulsions, and reduce the risk of complications from the heart and blood vessels.
During intensive stroke therapy, blood pressure is constantly monitored and this indicator is maintained 10% above the patient’s “working” pressure in order to establish blood supply to the brain. Monitoring of heart rhythm and metabolic rates in the body is carried out.
For cerebral infarction, conservative treatment methods are used. Within 5 hours from the first signs of the disease, thrombolytic intravenous therapy is carried out to dissolve the blood clot that has blocked the cerebral vessel. Therapy is carried out only with the consent of the patient (he must be conscious) or his relatives with the exact time of hemorrhage confirmed by CT.
If it is impossible to perform thrombolysis, the patient is prescribed antiplatelet drugs that reduce the formation of blood clots.
For treatment after a stroke, aspirin, dipyridamole, and clopidogrel are used no later than 48 hours. Aspirin is also prescribed in the future; patients take it up to a year after the stroke.
Transmural myocardial infarction
This type of heart attack is associated with large damage to the layers of the heart muscle. In a typical heart attack, the myocardium (the middle layer of the heart muscle) is affected. With a transmural infarction, the epicardium and endocardium - the outer and inner layers of the heart muscle - are affected, while necrosis affects the heart through and through.
With a transmural infarction, the blood supply is disrupted in the coronary artery basin. Immediately (within one minute) after the onset of acute ischemia, the force of contraction of the heart muscle over a wide area and depth decreases. The nature and size of the damage depends on various factors, including the need of the heart muscle for the intensity of blood supply, the ability of the vessels to take over the function of blood supply to the thrombosed artery, and the duration of development of the pathology.
Five periods of illness
Each period has its own characteristics and characteristics:
- Pre-infarction. This period can last for several days or even weeks. The main symptom is an increase in angina attacks.
- The sharpest. It has a short duration - maximum 2 hours. In other words, little time passes from the development of ischemia to the occurrence of necrosis. This period can last only 20 minutes, so urgent hospitalization is necessary.
- Spicy. As a rule, several days pass from the onset of necrosis to myomalacia. Maximum duration – 2 weeks.
- Subacute. Scars are already beginning to form. The maximum duration of this period is 2 months.
- Post-infarction. The scar matures, and the myocardium has to adapt to new working conditions. It is very important here how the heart behaves during fundamental changes. If there is no adaptation, there is a high probability of a second attack.
Symptoms and signs of a heart attack
Typical cases of heart attack are associated with severe pain in the chest, which radiates to the left shoulder, collarbone, neck, left half of the face, lower jaw, and interscapular area. The larger the area of damage to the heart muscle, the more severe the pain. The pain lasts more than 30 minutes and is not relieved by taking medications.
In the atypical course of the acute stage of a heart attack with unexpressed pain, acute weakness, sticky sweat, pale skin, tachycardia, arrhythmia, cough and suffocation, swelling and distorted consciousness may occur.
In the acute stage of a heart attack, the pain usually goes away. Due to necrosis, the temperature may rise and arterial hypotension may develop.
In the subacute period, the condition normalizes, tachycardia and systolic murmur disappear, pressure and temperature normalize.
What does death from a heart attack look like?
Any cause of death due to myocardial infarction is associated with a malfunction of the circulatory system. A pathological process in the heart muscle leads to irreversible processes, fatal sensations and, as a rule, death.
Processes in the body
Violation of the blood supply to the heart muscle of any etiology, which is the cause of death from a heart attack, is manifested by the following symptoms:
| Cause | Consequence |
| Violation of the rhythm and sequence of the stage of excitation and contraction of the heart muscle | Blood is pumped in insufficient volume, and coronary shock occurs (a sharp decrease in the ability of the myocardium to contract). In this case, clinical death occurs. |
| Stopping venous blood flow | Pulmonary edema occurs and death occurs due to a heart attack. |
| Inconsistency of the heart ventricles | Disorganized series of impulses arise in the ventricles of the heart, their source is in the lower chambers of the heart. Blood pumping stops, which causes death in myocardial infarction. |
| Rupture of the walls of the heart | The heart fills with blood, a rupture occurs and the heartbeat stops immediately. |
External signs of death from a heart attack
By some signs you can understand that a person is no longer a tenant.
They show what death that occurs from a heart attack looks like. In these cases, the following symptoms of impending death are noted:
- tachycardia or bradycardia;
- decrease in blood pressure: pulse becomes very rare;
- the skin acquires a bluish tint, the lips turn blue especially quickly;
- fluid stagnation and swelling occur in the lungs;
- loss of consciousness;
- convulsions;
- dilated pupils - reaction to light is almost completely lost;
- breathing is initially noisy and frequent, then becomes rarer, until it stops completely (apnea is recorded).
- absence of a curve on the electrocardiogram.
Important! Irreversible processes in the body develop 3-5 minutes after clinical death is declared. Only about 3-4% of patients emerge from clinical death without consequences. Other patients do not restore all body functions after resuscitation.
External signs of death from a heart attack are not reflected in any way on the dead body of the patient. Rigor mortis and discoloration of the skin occur at the same time as in patients who die for other reasons.
First aid for heart attack
If acute pain occurs, you must urgently call an ambulance
. In the absence of contraindications, you can take acetylsalicylic acid in a dose of 150-300 mg, after crushing the tablet.
Before the ambulance arrives, the patient must be kept in a reclining position and at rest.
In the room, you need to open the window and unfasten tight clothes and belt.
Doctors call the first hour of the most acute stage of a heart attack “golden”; the outcome of the disease most often depends on this time.
Treatment
In the most acute stage of a heart attack, first of all, doctors relieve pain. For this purpose, various analgesics and narcotics (morphine) can be used intravenously. For a faster effect, painkillers are administered intravenously.
After the electrocardiogram is taken, thrombolytics are administered to restore coronary blood flow. To eliminate a pain attack, neuroleptanalgesia is performed.
Next, the patient is prescribed a set of drugs to reduce the myocardial oxygen demand, beta blockers to reduce the load on the heart, medications to thin the blood and reduce the level of blood clotting. If necessary, inhibitors, sedatives and hypnotics are prescribed. The combination of drugs depends on the presence of concomitant diseases in the patient and the severity of the heart attack.
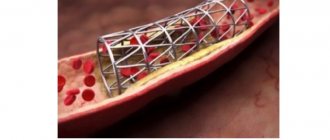
To treat a heart attack, surgical methods of restoring blood flow are used (coronary artery bypass grafting, balloon angioplasty).
During the first days of treatment, the patient is prescribed bed rest, and starting from days 3-4, the patient can sit on a chair for about an hour twice a day. With an uncomplicated heart attack, the patient is allowed to walk 5-7 days after the heart attack. In case of an uncomplicated form of myocardial infarction, the patient is discharged from the hospital on days 10-12; in case of complications, hospitalization can last up to 4 weeks.
Clinical guidelines
Clinical recommendations “Acute myocardial infarction with ST segment elevation of the electrocardiogram” were developed by the Russian Society of Cardiology with the participation of the Association of Cardiovascular Surgeons of Russia, approved by the Scientific and Practical Council of the Ministry of Health of the Russian Federation and approved by the Ministry of Health in 2021. The document contains information about the disease, forms of its diagnosis, symptoms, treatment methods, possible complications, care and rehabilitation.
Appendix B of the document contains recommendations for patients who have had a heart attack related to secondary prevention of the disease. The recommendations say that patients should stop smoking, ensure regular physical activity, follow a diet designed for such cases, lose excess weight, follow the doctor's recommendations, maintain low blood cholesterol levels with the help of medications, ensure stable normalization of blood pressure (if present). arterial hypertension), maintain normal blood sugar levels (in the presence of diabetes mellitus). In addition, with extensive damage to the heart muscle and/or complications of myocardial infarction, additional treatment is required, which is prescribed by a doctor. Stopping essential medications early is known to significantly increase the risk of another heart attack, death, and heart failure, which can significantly limit your daily activities. You should not stop taking medications without consulting your doctor. To reduce the risk of recurrent events (myocardial infarction, its complications), it is highly advisable for you to participate in a special rehabilitation program, including regular dosed physical activity, psychological support, and monitoring of risk factors.
Possible complications
In the first hours and days after the development of the disease, complications may appear. They significantly worsen the course of the disease and reduce the chances of successful treatment.
Most patients complain of interruptions in the heart (arrhythmia can be different). They can persist for several days. Particularly dangerous during this period is ventricular fibrillation, which then turns into fibrillation. A person's risk of death increases significantly.
Left ventricular failure has the following symptoms: congestive wheeze, pulmonary edema and some manifestations of asthma. Cardiogenic shock, which rapidly develops with a large infarction, poses a huge danger. Often doctors simply do not have a chance to save a dying patient. The main signs of such shock are: a sharp drop in blood pressure, rapid heartbeat, cyanosis, and impaired consciousness.
Often, patients experience rupture of muscle fibers, which can subsequently provoke cardiac tamponade. In less than 4 percent of cases, a person experiences a severe disruption of blood flow in the lungs. This complication is also characterized by increased mortality.
Another complication is acute cardiac aneurysm, which gradually turns into a chronic stage. As a result, heart failure occurs.
Fibrin deposition that occurs on the endocardial walls is a direct threat to various internal organs, including the kidneys, brain and lungs. Because of this complication, signs of a heart attack are especially severe in men and women.
The later period of the disease is accompanied by complications such as pericarditis and eosinophilia. There are also other serious illnesses.
Consequences of a heart attack
The early consequences of a heart attack include acute left ventricular failure, accompanied by shortness of breath, tachycardia and cough, cardiogenic shock, disturbances in heart rhythm and cardiac patency.
Approximately every fifth case of a heart attack results in thinning and bulging of the wall of the left ventricle (cardiac aneurysm) for the patient.
Often during a heart attack, against the background of varicose veins and prolonged bed rest, thromboembolic consequences occur, in which the vessels are blocked by blood clots.
It is not uncommon for acute coronary syndrome to be accompanied by problems in the gastrointestinal tract: ulcers, adhesions, erosions.
After an acute period of a heart attack, post-infarction Dressler syndrome (inflammation of the pericardium, alveoli, pleura, joints), a parietal thrombus in the heart cavity, and late post-infarction angina may develop. Also, the consequences of a heart attack include the risk of recurrence due to damage to the arteries.
However, patients with myocardial infarction can actively influence the prognosis regarding recurrence. Compliance with doctors' recommendations and lifestyle modifications makes it possible to live a full life after a heart attack.
Reasons for the development of the disease
Heart attack is an acute form of IHD (coronary artery disease). In the vast majority of cases (more than 95 percent), the cause of the disease is atherosclerotic damage to the arteries. This, in turn, provokes a narrowing of the lumen. Quite often, doctors record cases where atherosclerosis is combined with acute thrombosis of a part of the heart that has already been affected. All this leads to a complete (or partial) cessation of blood supply to the heart.
A heart attack can also develop due to the following diseases and factors:
- Diabetes.
- High pressure.
- Obesity and poor nutrition.
- Constant stress, depression and other nervous and mental illnesses.
- Constant use of cigarettes and alcoholic beverages. They also provoke symptoms of myocardial infarction.
Rehabilitation and recovery after a heart attack
The main tasks of rehabilitation after a heart attack are the restoration of the circulatory system, ability to work and a normal lifestyle. Rehabilitation includes a set of measures, consistently and continuously carried out under the supervision of doctors.
Rehabilitation measures are individual and depend on the patient’s condition, the severity of the heart attack, and chronic diseases. At the same time, the stages of rehabilitation are associated with being in a hospital, in a sanatorium and at home.
In the hospital, the disease is diagnosed, treatment is carried out after restoration of the patency of the coronary vessels, risks are assessed and a prognosis for the recovery period and relapse is formed.
The inpatient rehabilitation period is the time of the acute period of a heart attack, which the patient spends in a specialized rehabilitation department of the hospital and then in a cardiological sanatorium.
An outpatient rehabilitation period is provided for home conditions under the supervision of a cardiologist and exercise therapy doctor.
Rehabilitation is medicinal and non-medicinal methods of recovery. These include:
- gymnastics to prevent the formation of repeated blood clots and increase blood supply and oxygen supply,
- physiotherapy,
- psychological help.
At the same time, an individual set of measures includes a gradual increase in physical activity. Typically, two weeks after a heart attack, patients are allowed to walk up to 2 km per day, assessing the ability of the heart to work using echocardiography (ultrasound examination of the heart), and performing exercise tests.
The exercise therapy complex gradually includes swimming, walking at a pace, and training on exercise machines. Depending on the functional class of ischemia, classes are held in a training or gentle mode.
During rehabilitation, measures of psychological recovery are important. Returning to normal life and overcoming fear, including before physical activity, is an important stage of recovery after a heart attack. The formation of depressive and anxiety states can delay the results of rehabilitation for a long time and worsen its quality.
Non-drug methods, in addition to physical rehabilitation, include lifestyle correction:
- quitting smoking and alcohol,
- diet,
- full sleep.
Medicines are used for:
- preventing angina attacks,
- blood pressure control,
- blood clotting,
- lipid metabolism,
- treatment of arrhythmia and chronic heart failure.
A comprehensive rehabilitation program helps patients recover in a shorter time and prevent recurrent heart attacks and other complications.
Diagnosis of the disease
The peculiarity of diagnostic procedures is that they can be prescribed not only during the examination period, but also during the treatment of the disease. The doctor should systematically study data on the activity of serum enzymes, as well as electrocardiogram indicators. This allows you to avoid various complications in the future, which in turn increases the patient’s chances of successful treatment.
A person can come to a specialist with various complaints. They directly depend on the degree of development of the disease, its form and duration. A heart attack is detected when severe pain in the chest area persists for 30 minutes (the attack lasts up to one hour). In this case, the patient feels acute heart failure. Other heart attack symptoms may also appear in women and men.
An electrocardiogram, among other things, allows you to record various changes in the activity of the heart. For example, the doctor has the opportunity to detect a negative T wave, a pathological QRS complex and other negative phenomena. After this, the doctor needs to conduct a number of other diagnostic examinations, or prescribe an urgent operation.
In the first few hours after the onset of severe pain, there is a sharp increase in myoglobin in the blood. This is a special protein whose main task is to supply oxygen inside the cells.
8 hours after the onset of a heart attack, a noticeable increase in creatine phosphokinase activity may be observed. Gradually the indicators are normalizing. The stabilization process takes about two days, sometimes less. The level of creatine phosphokinase in the blood should be measured several times a day. This should also be classified as diagnostic procedures that are of particular importance to the patient.
In the later stages of the disease, doctors also use different diagnostic methods, despite the fact that the risk of death increases. In particular, a specialist needs to determine the enzyme lactate dehydrogenase. The indicator returns to normal only after one week. It often takes two weeks for lactate dehydrogenase enzyme levels to normalize and stabilize.
Unstable angina can provoke an increase in troponin protein isoforms. Doctors detect these changes through tests. Symptoms of a heart attack in a man or woman may also subside.
The blood test that the patient gives allows the doctor to see an increase in the level of ESR, leukocytes and other elements. The clinical picture looks more complete, which contributes to successful treatment in the future.
Many cardiologists prescribe echocardiography, the main task of which is to identify various disorders of ventricular contractility, as well as thinning of its wall.
In more prestigious clinics, a modern diagnostic procedure is performed - coronary angiography. It allows the specialist to identify thrombotic occlusion of the artery. In addition, this diagnostic method allows the doctor to determine whether it is advisable to perform surgery on the patient’s heart or not. In other words, the likelihood of bypass surgery or angioplasty is assessed. Such radical treatment methods are often the only path to salvation when serious heart diseases are detected.
RECOMMENDATIONS FOR LFK
Classes at the hospital stage must be conducted by a physical therapy instructor. Although the complex for this group of patients is very gentle, the load still depends on the patient’s condition. Severe degrees require complete rest during the first week. With moderately severe patients, the instructor begins classes on the 2nd – 3rd day.
On the 4th – 5th day the patient is allowed to sit for some time on the bed with his legs dangling. From the 7th day you can take your first steps near the bed. After a couple of weeks, the doctor will allow the patient to “walk” around the ward. Go out into the hallway - from the 3rd week. With the help of an instructor, you can try to climb several steps. The number of steps and meters covered is growing every day (up to 500 - 1000 m). The patient is under the supervision of doctors or relatives, because his condition needs to be constantly assessed - by heart rate (heart rate - pulse) and blood pressure level. For reliability, these indicators are checked before the walk (half an hour) and after (half an hour).
If the treatment proceeds without complications, the patient, after an inpatient course, is sent to a cardiological sanatorium somewhere in the suburbs. There is no need for such a patient to travel long distances. There, as part of a 4-week rehabilitation course, he will receive:
- Drug treatment.
- Help from a psychotherapist.
- Diet food.
- Dosed physical activity.
REHABILITATION IN THE POLYCLINIC
Patients who have had a heart attack are divided into 4 categories according to the severity of the heart attack and the condition after it. This is determined by the doctor based on examination data. For 1st and 2nd grade
characterized by somewhat greater physical activity.
Such patients are prescribed sanatorium treatment immediately after hospitalization, and after that a recovery course in a clinic at their place of residence. Three times a week they visit exercise therapy
, where classes are held in 4 modes (gentle, gentle training, training and intensive training).
The individual physical rehabilitation program is based on determining the severity of the patient’s condition, the severity of coronary insufficiency, the presence of complications and the nature of the heart attack. It is aimed at increasing the functionality of the myocardium, as well as improving the nutrition of the heart muscle by stimulating intracellular metabolic processes.
Also, as part of the program, the doctor carries out an individual selection of medications.
.
works with such patients .
It is very important that the person leaves the expectation of a second heart attack and the feeling of fear.
REHABILITATION AT HOME
Using the recommendations of exercise therapy instructors, patients should regularly do a set of exercises at home. This includes morning exercises and walking. But we must not forget about self-monitoring (measure blood pressure, pulse). For hiking, it will be useful to purchase a pedometer - this way you will know the results of your training, and possibly your achievements. Do not forget about alternating loads and rest.
To quickly say goodbye to the disease, a person needs to forget that he is sick, believe in himself and his speedy and final recovery. Your loved ones should also work on this. A calm, friendly atmosphere should reign in the house. A person must feel necessary, useful, believe in his return to normal life, perhaps to his favorite job.
Some patients who suffered a heart attack belong to the 3rd and 4th functional class
. Their rehabilitation program differs from the program of the first two. Its goal is to provide the patient with such a level of activity that he can care for himself independently. Perhaps - do simple housework or work in an intellectual field (at home).
Physical rehabilitation of this group of patients takes place at home (physical therapy, massage, walks in the yard, slowly climbing a few steps up the stairs). But the patient must be visited periodically by a therapist and a cardiologist.
When you don't die from a heart attack
A favorable prognosis is given to patients with minor, localized myocardial damage, when only part of the organ is susceptible to necrosis. In this case, the cells that remain unharmed take over the functions of the entire organ, and the person, having undergone the necessary therapy and rehabilitation measures, continues to live. However, it is extremely important to follow all the recommendations of your doctor.
Medicine does not stand still: scientists are working to create drugs and techniques that will reduce mortality from heart attacks. Until this happens, a person must take care of his health to avoid a heart attack.
HELP OF THE SAMAZDRAV RESPIRATORY SIMULATOR IN REHABILITATION
To quickly return to a normal lifestyle, you can use the Samozdrav breathing simulator. Regular exercises on this device will improve blood supply to the heart. It can be especially useful for that group of patients who undergo rehabilitation at home.
You can start training on the simulator within 3 months after a heart attack. The Samozdrav simulator is useful both for the rehabilitation of the patient and for the prevention of a recurrent heart attack. After all, with the help of a hypercapnic mixture, vascular spasm is relieved and the functioning of the entire cardiovascular system is improved.
Due to constant training, a system of collaterals is formed - small blood vessels around the heart. They provide alternative blood supply and more complete nutrition of the heart muscle.
By exercising on the Samozdrav simulator, the patient will recover faster after a heart attack, because blood flow is normalized and the load is removed from the coronary vessels. Classes on the Samozdrav simulator will give tangible results within 3-4 months, and for such a serious illness as a heart attack this period is quite short.
Disability after a heart attack
A heart attack requires a long period of treatment and rehabilitation. At the same time, a person’s full working capacity is not always restored. For these reasons, permanent or temporary disability is given to patients with a heart attack quite often.
All patients who have suffered a major heart attack have the right to four months of paid rehabilitation based on the compulsory medical insurance policy. Usually this period of rehabilitation is enough to understand whether a person needs a disability or whether he is able to fully begin his usual work. If there is reason to think about partial loss of ability to work, the patient, on the recommendation of the attending physician, can undergo an examination by a medical and social expert commission.
To assess the level of disability, the commission will assess:
- patient self-care options,
- his education,
- possibility of returning to normal work,
- general health.
As a result, disability may be assigned to those whose work involves frequent stress, increased attention, and physical activity; pensioners and patients who have undergone vascular surgery; people with heart failure or unstable angina, as well as those who have lost their ability to work by 50 percent or more.
The commission evaluates each case individually and makes a decision based on a combination of factors both on the fact of establishing disability and on its group.
Diet
In the first week after myocardial infarction, a low-calorie diet with limited fluid, salt, fat, excessive fiber and cholesterol is recommended. The diet should include foods rich in potassium and vitamin C.
In the first week, food is served pureed, in small portions 6-7 times a day. It can be:
- semolina,
- oatmeal,
- buckwheat,
- rice porridge,
- lean veal,
- chicken,
- fish,
- steamed white omelette,
- cottage cheese and kefir,
- carrot and apple salad,
- beets and cabbage,
- fruit purees,
- honey.
You can't eat:
- baked goods and sweets,
- smoked,
- fried,
- fatty,
- spicy,
- salted and pickled dishes;
- pasta,
- beans,
- coffee,
- boiled and fried eggs.
After the acute period, whole foods are introduced into the diet, but dietary restrictions should become the norm for a person.
The basis of the diet should be:
- vegetables,
- fruits,
- nuts,
- lean meats and fish,
- cereals
Smoked, canned, fried and salted foods are not recommended for consumption. It is convenient to control your weight using your body mass index (the result of dividing your weight in kg and height in meters squared).
It should be within 25-27 kg/m. In addition, the waist circumference is assessed: for men this figure should not exceed 94 cm, for women – 80 cm.
Diet for weight loss
First breakfast.
One hundred grams of low-fat cottage cheese, a cup of coffee with milk and without sugar.
Lunch.
Fresh cabbage salad (170 g) with sour cream without salt.
Dinner.
Vegetarian cabbage soup (200 ml), 90 g lean boiled meat, 50 g green peas, 100 g apples.
Afternoon snack.
One hundred grams of cottage cheese and 180 ml of rosehip decoction.
Dinner.
Boiled fish (100 g) and vegetable stew (125 g).
Before going to bed, at night.
Kefir (180 ml) and 150 g of rye bread.
Let us repeat, this is an approximate diet for one day. This diet contains 1800 kcal.
For patients without excess weight problems, the diet is significantly expanded.
They are prescribed a diet with a calorie content of 2500 - 3000 kcal
. The consumption of animal fats and carbohydrates is limited. Also 4-5 meals a day. It is useful to spend fasting days on apples (1.5 kg) or fresh cucumbers (2 kg). For “avid meat eaters”, 600 g of lean meat plus a side dish of vegetables (fresh cabbage, green peas) are even allowed.
Strongly not recommended
Doctors do not allow such patients to drink
alcohol
, even of the highest quality. It causes tachycardia and an undesirable increase in appetite. The consumption of smoked meats, fried foods, fatty sausages and sweets is absolutely unacceptable.
Breathing exercises after a heart attack
A heart attack is an acute condition associated with extreme strain on blood vessels and extreme circulatory impairment. Lack of oxygen in the heart muscle leads to its death. Unfortunately, necrosis of the heart muscle is irreversible, but nevertheless, it is necessary to create conditions for sufficient oxygen in the body for both primary and secondary prevention of the disease.
Acute pain during angina attacks, which are precursors to a heart attack, signals the myocardium about problems with oxygen.
The surest way to provide the heart muscle with enough oxygen is to reduce risk factors and breathe properly. We receive oxygen through the respiratory organs, and they must be trained and tuned to support a full respiratory cycle.
The Samozdrav breathing simulator can become a confident and powerful support in the prevention of heart attack. One of the basic positive effects of breathing training on the body is sufficient oxygen supply to the body and maintenance of normal CO2 levels. Thanks to training with Samozdrav, you can constantly maintain oxygen levels at a level that eliminates oxygen deficiency. This means a high probability of myocardial preservation and significantly reduces the risk of heart attack.
In addition to the “direct supply” of oxygen to the body, breathing training strengthens the functioning of the nervous system and corrects reactions to stress, providing peace and a smooth emotional background even under high loads.
Training with Samozdrav corrects metabolism and is effective in treating obesity. They activate metabolism by normalizing the level of oxygen in cells and tissues, normalize the excretion of metabolic products, and allow for better absorption of nutrients.
Samozdrav is indispensable for patients with hypertension. It was the treatment of this disease that became the primary goal of the creators of the breathing simulator, and today its effectiveness in treating hypertension without medications has been fully proven by research and many years of practice of use by millions of people.
Breathing training can cope with any modified risk factor for heart attack. Regular exercise will give the myocardium sufficient oxygen levels and keep the heart healthy.
Prevention of MI
The only way to prevent the development of a large heart attack is to control risk factors for the development of the disease and seek medical help in a timely manner. It is important to eat right, be physically active, have a healthy weight, not smoke, and not abuse alcohol.
If you suffer from diabetes, hypertension, coronary heart disease, or have thyroid problems, do not start the disease. Visit your doctor on time and follow his instructions. Ignoring medical recommendations and undisciplined pill taking significantly increase the chances of developing AMI.
It is also necessary to undergo regular medical examinations and tests. Determining cholesterol and sugar levels, measuring blood pressure, and monitoring ECG help identify diseases at the earliest stages and take timely measures to prevent progression.