Features of the manifestation of fibrosis of heart valves
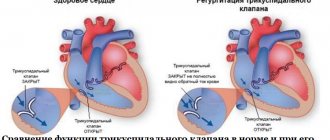
The condition does not worsen immediately. It is possible to identify compaction of the valve wall from the clinical picture of a hemodynamic failure only with the development of severe regurgitation. It is characterized by reverse blood flow. It returns to the atrium or ventricle depending on the affected valve. The essence of the problem lies in the incomplete closure of the valves. Sometimes it happens the other way around. Fibrosis leads to the fusion of the valves with each other. In the first case, the pathological process provokes an enlargement of the atrium, and in the second, a narrowing of the valve opening.
The degree of regurgitation varies between mild and severe. The clinical picture will depend on the severity of the pathology.
Mitral valve damage
If the mitral valve leaflets are compacted, the patient may eventually develop the following symptoms of fibrosis:
- fast fatiguability;
- frequent shortness of breath;
- feeling of heartbeat;
- arrhythmia;
- feeling of shortness of breath;
- pain in the heart area;
- swelling of the legs.
Aortic valve damage
Fibrosis of the aortic valve contributes to the manifestation of cerebral hypoxia. The patient exhibits a pathological process with the following symptoms:
- general weakness;
- pulmonary edema;
- loss of consciousness;
- angina pectoris.
Treatment
{banner_banstat3}
Treatment of the pathology is complex and serious, aimed at eliminating the cause
. Patients are advised to lead a healthy lifestyle, eat right, fight bad habits, walk in the fresh air, avoid stress, and be under the supervision of a doctor.
- If the cause of the pathology is atherosclerosis, patients are prescribed an anti-cholesterol diet and medications that reduce the level of LDL in the blood - statins Fluvastatin, Lovastatin, fibrates Clofibrate, Fenofibrate, drugs that enhance
the excretion of bile acids - Cholestyramine, Cholestipol " - To treat hypertension, drugs of different groups are used: diuretics - Hypothiazide, Veroshpiron, adrenergic blockers - Atenolol, Bisoprolol, slow calcium channel blockers - Nifedipine, Amlodipine.
- Peritonitis requires emergency surgery.
- If thickening of the aorta is a consequence of arteritis, anti-inflammatory therapy is carried out.
- Venereologists prescribe antisyphilitic drugs - drugs of penicillin, bismuth, arsenic, mercury.
Surgical treatment for thickening of the aortic valve leaflets involves repair or replacement of the valve. In the case of aortic dissection along its length, or the formation of an aneurysm, the issue of vessel prosthetics or installation of a stent in the thickening zone is resolved.
Traditional medicine to strengthen the structure of the aorta:
- The garlic is peeled, crushed, and poured with boiling water. The infusion is stirred several times during the day, lemon juice is added and infused for a week in a dark and cool place. Take the resulting remedy one teaspoon three times a day half an hour before meals. The duration of treatment is three months.
- An infusion is prepared from rowan bark and water. The resulting product is boiled for two hours, cooled and filtered. Take a tablespoon three times a day.
- A collection of clover grass, rose hips and hawthorn berries, hops, mint, oregano, motherwort, and sweet clover is poured with boiling water, left for two hours, filtered and taken three times a day before meals for a month.
Currently, there are many treatment methods aimed at restoring the structure of the aorta. But before starting such therapy, you need to consult with your doctor.
Fibrosis classification
Each form of pathology has its own characteristics.
- The focal form is the basic one. It is characterized by moderate fragmented damage to the structure of the valve apparatus.
- The diffuse type is characterized by a large area of damage (cusps and subvalvular space). It is detected at advanced stages of fibrosis development.
- The cystic form is perceived as a separate pathology. It manifests itself as serious disruptions in metabolic processes and leads to the formation of cysts.
If the cusps of the mitral valve are sealed, then it is not at all necessary that this is a heart defect. Fibrosis is only a pathological change that occurs under the influence of other factors, and not a diagnosis. Because of it, stenosis and valve insufficiency can develop. The appearance of voiced pathologies requires urgent medical intervention. The proliferation of fibrous tissue can be perceived as a substrate for the formation of cardiac muscle defects. However, it is unlikely to predict its development in advance. The chances of timely identification of the problem increase through regular examination.
Fibrosis of the heart and liver. Renin-angiotensin-aldosterone system and fibrosis
00:00
Drapkina Oksana Mikhailovna , executive director of the Internet Session, secretary of the interdepartmental council on therapy of the Russian Academy of Medical Sciences:
— I will give the next lecture. It will be called “Fibrosis of the heart and liver: what is common.”
Dear colleagues, the topic of fibrosis, in my opinion, is very relevant. It gives us the opportunity, if possible, to make our tissues (connective, parenchymal, muscle cells, any other tissue) live longer. Fibrosis is the natural aging of the body. Fibrosis of any organ (I want to emphasize again), any cell (it could be an endothelial cell, a vascular cell, a liver cell). The mechanisms of fibrosis development are largely similar.
Today I will try to begin our educational course, which we hope to make continuous. This problem will involve more than just cardiologists. Hepatologists will definitely be involved. In particular, Professor Pavlov, who works in our clinic. He deals with the liver problem very seriously. Pulmonologists and so on.
My task today is to talk about possible parallels between the formation of fibrosis of the heart and liver. Are there such parallels or are these fictitious attempts to connect different processes together?
I would like to pay attention to the role of the renin-angiotensin-aldosterone system in the pathogenesis of fibrosis formation. We have already seen today this ubiquitous angiotensin-2, which interacts with angiotensin type 1 receptors. It will identify all the adverse effects (in particular, by affecting insulin resistance, it increases the pressure of obese hypertensive patients).
Now let's look at it from a slightly different angle. From the perspective of fibrosis development.
What it is. Definition. Fibrosis is a thickening of connective tissue with the appearance of scar changes. We are very familiar with areas of fibrosis after, for example, a myocardial infarction.
These scar changes can occur in various organs. They arise, as a rule, at the site of chronic inflammation: atrophy or dystrophy.
A molecular definition can be given. We can say that fibrosis is the excessive accumulation of fibroblasts and extracellular matrix proteins, including collagen, in tissues.
Today, within 20 minutes, we must trace the fate of collagen, which is the main structural unit of tissue fibrosis.
The history of the study of the issue dates back to 1872, when William Gull and Henry Sutton described arteriocapillary fibrosis, which develops in kidney disease.
Nobel laureates have already worked in the 1930s of the twentieth century. They worked to uncover the structure of collagen. It was revealed.
03:22
In the 1960s, John Ross and Eugene Braunwald began to study the effect of angiotensin on cardiac function. Then the first works appeared on the relationship between diabetes mellitus and myocardial fibrosis. Or a hypertrophied left ventricle due to arterial hypertension and myocardial fibrosis.
Previously, Georgy Fedorovich Lang , the indisputable authority of the Russian medical school, had already found “gentle fibrosis” (as he said) in the hearts of patients suffering from arterial hypertension.
More recently, quantitative and qualitative assessment of fibrosis has become possible. Of course, we strive to develop more and more non-invasive methods in our diagnostic capabilities. Of course, liver biopsy and myocardial biopsy are not always available.
Liver biopsy is available, but myocardial biopsy is difficult. Now they are struggling with which method will be comparable in its sensitivity and specificity to the morphological one.
The main characters are whom we should know by sight when talking about fibrosis. These are fibroblasts, collagen. And here we are interested in collagen of the first and third types. These are components of the extracellular matrix. We will mainly talk about proteoglycans here.
The matrix metalloproteinases themselves and their inhibitors (that is, the ratio of matrix metalloproteinases that are responsible for collagen degradation and matrix metalloproteinase inhibitors) will be targets that can be targeted with various therapeutic agents in order to either increase collagen synthesis or have a greater effect on its degradation.
Profibrotic markers. The most famous are, of course, TGF beta (growth marker).
05:28
What is collagen? Collagen is a triple helix. This triple helix of collagen makes up 1/3 of all the proteins in the human body. It is formed by protein chains. When these triple helices of collagen, which are extended by protein chains, converge and stitch together, rod-shaped collagen molecules are formed. They form very strong, inextensible collagen fibrils. Their strength is comparable to that of steel.
You understand how difficult it is to reverse fibrosis, for example. In my opinion, it is better to do everything possible to prevent fibrosis from forming.
How does collagen synthesis occur? Collagen synthesis is a process that requires cellular and extracellular synthesis. The collagen precursor is synthesized on ribosomes on the surface of the endoplasmic reticulum. It's called preprocollagen. Post-tranquilizer modification then occurs in the Golgi complex. Some signal peptides are cleaved off.
Procollagen appears, which still carries a long propeptide at one end. This is followed by hydroxylation and glycosylation. Oxidation of cystoine residues leads to the formation of intermolecular disulfide bonds.
The very last stage is condensation with the formation of intra- and intermolecular bonds. When all these stages are completed, we get collagen.
(Slide show).
Section of the left ventricular myocardium of any patient. It is important that the connective tissue framework of the myocardium consists of three main components: epimysium, endomysium, perimysium. The endomysium surrounds a large muscle fiber. These are dense bundles of collagen that make up the connective tissue layer surrounding the entire myocardium. Epimysiums are part of the epicardium and endocardium.
Endomysiums are collagen fibers that surround each muscle fiber and form a mesh sheath. Around these muscle fibers there are also capillaries. This is also very important. Interpersonal relationship between muscle fiber and capillary.
08:48
Endomysium and epimysium connect perimysium. The role of perimysium is extremely important in relaxation processes. The perimysiums are rather thick bundles. They thicken, shorten during systole and lengthen, almost turning into a continuous ribbon during diastole. The more elastic the perimysium is, the more elastic our heart will be.
Thus, in the process of myocardial fibrosis, which we will talk more about today, these three bundles play a great importance. Epimysium, endomysium, perimysium.
(Slide show).
Ultrastructural level. On the left is an electron micrograph of a fragment of the left atrium. We see how collagen fibers are located between the fibroblast and the capillary. Most likely, we are talking about endomysium here.
The adjacent image shows how the cardiomyocyte is separated from the capillary by a thin plate of fibroblast growth. If the fibroblast is activated (we will recall once again below what agents it can be activated), this will lead to the fact that the fibroblast process will gradually be replaced by connective tissue.
Let's make the complex simple. Let's ask ourselves: what is the process of collagen formation? Or what fibrosis is. Fibrosis is the predominance of collagen synthesis over its breakdown.
Collagen synthesis and conversion requires lysyl oxidase activity. Then metalloproteinase comes into play. Metalloproteinase inhibitors will reduce the effect of the latter metalloproteinases. Collagen degradation occurs.
We must not confuse what we see (fibroblast). We must understand that this is not just a predominance of collagen synthesis over its breakdown. This is also the process of collagen structuring. Only structured collagen is important in the development of fibrosis, and not just bundles of collagen that will be scattered throughout the myocardium.
11:27
We know very well the different types of fibrosis, which indicate which path the tissue will take: apoptosis or necrosis. Normal tissue consists of cardiomyocytes that are connected to each other end to end.
If myocardial infarction suddenly occurs and reparative fibrosis forms at the site of the scar, then normal cells begin to alternate with cells - sections of connective tissue. Such reparative fibrosis occurs at the site of dystrophic changes. Here, arttrophy and tissue degeneration underlie this type of fibrosis.
Reactive fibrosis is something we see much more often. These are all hypertensive patients (many, in any case) with a long history of arterial hypertension (AH), with poorly treated hypertension. Reactive fibrosis. Here there is an increase in the intercellular matrix. Collagen bundles become thicker.
Vladimir Leonidovich spoke today about arrhythmias. My deep conviction is that, apparently, fibrosis processes are to blame for arrhythmias (especially supraventricular ones). In particular, perhaps, in the atria.
We will have 20 minutes of discussion. I think everyone can have their say on this matter.
Many experimental studies have proven that fibrosis can serve as the basis for the development of tachyarrhythmia. The most arrhythmogenic zone is the zone of the mouth of the pulmonary veins. They try to limit this zone during minor surgical interventions for rhythm disturbances.
(Slide show).
With tachyarrhythmias, the slices take on this shape. White is areas of fibrosis. The more fibrosis, the more prepared such an atrium will be for takiarrhythmia.
13:51
Here we see disorganized bundles of myocardial sleeves. They very densely envelop the mouths of the pulmonary veins. Accordingly, there are even works that suggest that the manifestations of fibrosis and its prevalence and localization may have prognostic significance for the choice of tactics for managing a patient with arrhythmia.
What affects fibrosis? What is beneficial for us, on the contrary, is to stimulate in order to prevent the development of fibrosis. We are interested in fibrogenesis stimulators and inhibitors.
Angiotensin-2 is a fibrogenesis stimulator. There are intimate connections between angiotensin-2 and TGF beta. These connections are not fully disclosed. Today we will try to talk about them again.
Other growth factors. The second character we know well is aldosterone. The more angiotensin-2 and aldosterone in our patient's plasma or tissue system, the greater the potential for him to have fibrosis of the heart and (as I will show later) liver.
Endothelins, catecholamines, adhesion molecules, galectin-3. There is now a lot of work being done on the role and specificity of galectin-3, which increases during fibrosis. On the other hand, an increase in the synthesis of nitric oxide, an increase in the activity of natriuretic peptides, bradykinin, and prostaglandins leads to the fact that fibrosis in such patients (if the activity of these agents is high) will occur to a lesser extent.
Well-known hormones (growth hormone, thyroxine, angiotensin-2 and aldosterone). If we compare their effect on several stages in the development of fibrosis (collagen synthesis, collagen degradation and collagen accumulation), note that growth hormones and thyroxine affect collagen synthesis and degradation. In these practically equally directed processes, conditions are not created for collagen accumulation to occur and connective tissue to accumulate.
On the contrary, the influence of angiotensin-2 and aldosterone predominates on collagen synthesis. Angiotensin also reduces collagen degradation, which has a very pronounced effect on collagen accumulation. Aldosterone primarily acts on collagen synthesis without affecting collagen degradation. Accordingly, accumulation also occurs, but to a much lesser extent.
16:59
(Slide show).
A well-known scheme was published in 2008. Cardiomyocytes and fibroblasts. Muscle fiber contains cardiomyocytes and fibroblasts. Cardiomyocytes are shown in pink. Fibroblasts are depicted as ugly shapes in blue with a nucleus.
In response to mechanical distension (for example, increased pressure in the left ventricle because systemic arterial pressure (BP) rises or for some other reason), the pressure inside the ventricle increases. According to the pressure gradient, there will be an increase in the system, for example, the left atrium. This results in mechanical stretch, which stimulates TGF beta activity.
At the same time, angiotensin-2, influencing the same mechanisms and mechanisms that occur in fibroblasts, also activates TGF beta activity. All this leads to an increase in the organization of collagen and other proteins of the intercellular matrix and fibrosis occurs.
What can affect fibrosis. Something that can block the renin-angiotensin-aldosterone system. There have been many novel models that have shown that angiotensin-converting enzyme inhibitors lead to a significant reduction in fibrosis.
Today I will dwell more on Lisinopril, since I also added liver fibrosis to this fibrosis.
If we talk about liver fibrosis, the mechanism was similar. Again we see TGF beta in the arena, which will be activated by angiotensin-2. You have the right to ask me: where does angiotensin-2 come from in the liver? Liver tissue (like any tissue) is equipped with blood vessels. There are many vessels. It is with the processes of changes in blood vessels that the processes of fibrogenesis begin to occur in the liver. I will show this a little later.
There are certain parallels in the development of fibrosis of the liver and heart. These parallels lie in the same clinical predictors of the development of fibrosis and cirrhosis of the liver and cirrhosis and fibrosis of the heart.
Firstly, this is age. Secondly, it is an increased body mass index. Thirdly, these are comorbid conditions such as, for example, insulin resistance and diabetes mellitus. Today we also talked about how angiotensin-2 acts on insulin resistance. This is a change in transaminase levels and an increase in triglyceride levels.
20:08
In the heart, reactive fibrosis is observed in hypertension and abdominal obesity. Epicardial fat, which is visceral fat and a springboard for the secretion of adipokines and faster myocardial fibrosis, which is also initially associated with impaired diastole. This means fibroformation, which increases in such patients.
Thus, we can say with some confidence that epicardial fat is a new marker of cardiovascular disease (CVD). It correlates with both visceral fat and subclinical atherosclerosis, the outcome of acute coronary syndrome (ACS) and, finally, the diagnosis of metabolic syndrome.
A few more words about fibrosis of the liver and heart. Common pathophysiology. We need to focus on the very interesting agent galectin-3. Now there is a lot of work that shows that galectin-3 increases in liver fibrosis.
Personal attention is given to an oral caspase inhibitor and an apoptosis inhibitor. These studies are still in progress.
I promised to prove that the liver and blood vessels are by no means mutually exclusive. The liver is permeated with blood vessels. It is with the calillarization of the sinusoid that the processes of fibroformation begin. If normally the basement membrane is a membrane with pronounced spaces of Disse (that is, fenestrations are detected between the sinusoids), then with mechanical damage the sinusoids lose fenestrations. Exchange with the capillary and blood flow changes. This is how fibrosis forms.
Otherwise, ACE inhibitors have something to act on in the liver of such a patient.
The last component is vascular fibrosis. Vascular fibrosis is a process that is obligatory in an elderly person. It increases with age. This is the main reason for the increase and stiffness in hypertension. It is possible to draw a logical connection that a stable increase in blood pressure leads to the activation of fibroblasts and a decrease in the activity of metalloproteinases.
12:47
The only thing that is not clear is what initiates the process of fibrosis. It is possible that the role of immune cells or immune cells that infiltrate the vascular wall perform this unpleasant role.
Perivascular fibrosis due to diabetes mellitus. There are a lot of such patients.
Dear colleagues, remember your workday yesterday, your workday today. You probably remember patients with diabetes who come with chest pain. On coronary angiography, their coronary arteries are clear. What's the matter?
The fact is that this anginal status may be a consequence of extravasal compression of the coronary arteries, because glucose promotes the formation of collagen “crosslinks”. In patients with diabetes mellitus, perivascular fibrosis is very pronounced.
The effects of blockers that inhibit the renin-angiotensin-aldosterone system are pathogenetically justified for the prevention of fibrosis, both in the heart and in the liver. They act on TGF beta and on the activity of some metalloproteinases. For example, metalloproteinases of the first type.
All this confirms the term: what is good for the heart is also good for the liver. There is no longer any doubt about this. I'll touch on this briefly.
Non-alcoholic fatty liver disease. It would seem a completely safe, harmless state. But not so harmless. These patients have the opportunity to die from CVD many times more often than without such suffering.
Increased risk of carotid atherosclerosis. The kinetics of the thrombus changes. Non-alcoholic fatty liver disease is a predictor of CVD, independent of other risk factors. The ways of applying and correcting this condition, which at first glance seems harmless, are changing.
If we are talking about fibrosis, then ACE inhibitors, statins, and renin-angiotensin receptor blockers must be used in such a patient.
25:14
What to choose. What to prescribe to an obese hypertensive patient from the perspective that fibrosis exists in both the heart and liver. Probably, drugs that do not require additional metabolization in the liver and that circulate in the plasma link of the renin-angiotensin-aldosterone system come to the fore here.
From this point of view, Lisinopril has proven itself to be very good. We use the drug “Diroton” in our practice. When you ask doctors if there is an original drug, Lisinopril, they all answer that it is Diroton. He has proven himself so well. Its metabolic neutrality and lack of transformation in the liver are captivating.
Very often, a patient who has fibrosis (this is a high-risk patient) needs combination therapy. Today we talked a lot about this combination (extremely interesting, metabolically neutral). Calcium antagonists and things that block the renin-angiotensin-aldosterone system.
There is a combination “Equator”, which consists of “Lisinopril” and the beloved “Amlodipine”, which we also use in patients.
In this regard, I would like to recall and refer to the results of a study that we conducted earlier. We tried to see what Lisinopril would do in a patient with concomitant liver pathology.
We took patients with hypertension (mild and moderate). There were 25 patients. We looked after them for 12 weeks. The dose of Lisinopril was titrated from 5 mg to 20 mg per day. It turned out that during a routine examination...
There were 4 visits, at each visit the patient’s clinical status was examined in detail: electrocardiogram, echocardiogram, dose titration and blood pressure monitoring were performed. The patients were distributed as follows. These were mainly patients with moderate hypertension. The experience wasn't very long. Experience prevailed from one to five years.
According to concomitant liver disease, patients were distributed as follows: mainly included patients who had alcoholic liver damage. At the third visit, a significant decrease in blood pressure levels was already noted with Lisinopril. This was all accompanied by a decrease in the levels of transaminases, glutamine transpeptidase and alkaline phosphatase.
All patients demonstrated excellent tolerability. One patient discontinued lisinopril in this study due to headache.
28:14
So, what can we say about fibrosis of the liver and heart. First, this problem is urgent. Secondly, these two processes in two completely different organs (vessels should be added here) have many similar indicators. This makes it possible and necessary to use drugs that have proven themselves in terms of their effects on the cardiovascular system and liver.
Principle: What is good for the heart is also good for the liver.
The last conclusion: the reduction of fibrosis is a process that is now very much developing. We need to read, watch, understand that such drugs as Relaxin, statins, inhibitors of the renin-angiotensin-aldosterone system. Good experience has been accumulated with Diroton. Destroyer of cross-links of proteins. Oxidase inhibitors, which interfere with collagen organization. Phospholipase D inhibitors. Genetic therapy. Especially micro-RNKs. I think that this will help solve the problem of fibrosis in the next 100 years.
Thank you for your attention.
What it is?
You can understand what fibrosis of the mitral valve leaflets is by looking at the features of its structure and functioning.
The essence of the operation of the valve apparatus is to allow blood to pass (in one direction) when a certain section contracts. The main role is played by the valves, which are represented by loose connective tissue. Their nutrition is carried out through the smallest vessels. The aortic valve has three leaflets (right, left, posterior), and the mitral valve has two (posterior, anterior). Under the influence of irritating factors, the connective tissue becomes coarser, which is why it ceases to fully perform its functions (maintain the flexibility of the valves). Over time, the number of blood vessels supplying the valve is significantly reduced. The cells that make up it begin to die, being replaced by fibrous tissue. It is one of the types of connective tissues, which is characterized by high strength.
Causes
{banner_banstat0}
The main etiological factors of aortic thickening:
- Atherosclerosis is the main cause of the pathology. According to its structure, the aorta belongs to the vessels of the muscular-elastic type. They are the ones most exposed to LDL. Lipids are deposited on the inner lining of the aorta and lead to the development of rough fibrous tissue. Plaques form, protruding into the lumen of the vessel and growing with scar tissue. Compaction of the aortic root is always accompanied by spasm of the coronary arteries, which leads to the development of hypoxia and myocardial ischemia.
serious atherosclerotic changes in the aorta with the formation of a life-threatening aneurysm
- Systematic hypertension is another cause of this disease. With hypertension, blood moves through the aorta under high pressure, the walls of the vessel gradually become denser and lose their elasticity due to the formation of fibrous structures. The rigidity of the aortic walls changes, their thickness increases.
- Infectious pathology leads to hardening of the aorta: acute and chronic streptococcal infection, rickettsiosis, brucellosis, sepsis.
- Autoimmune systemic diseases accompanied by long-term aortitis - scleroderma, rheumatoid arthritis, periarteritis nodosa.
- Long-term use of certain medications: antibiotics, sulfonamides. The thickening of the walls of the aorta over time leads to its expansion and atrophy.
- Tuberculosis infection.
- The heart is enlarged to the left, the aorta is compacted - signs of natural aging of the body.
Syphilitic infection occupies a special place among the causative factors of pathology. Thickening of the aorta is a late clinical sign of a long-term syphilitic process, developing 10-20 years after infection.
aortic valve seal
Factors contributing to aortic thickening:
bad habits, foods high in cholesterol, hereditary predisposition, systematic overeating. Under the influence of these factors, the aorta automatically thickens and becomes highly sensitive to traumatic damage. The consequence of the pathology is sclerosis of the valve leaflets and the aortic ring. They lose their mobility, aortic stenosis and aortic regurgitation develop.
Fibrosis of the mitral valve leaflets
Fibrosis of the mitral valve leaflets is a rather dangerous and serious condition. The reasons for its occurrence are very diverse. It is worth considering them in more detail.
Causes
Quite often, this disease appears after the patient has suffered a myocardial infarction. A common cause is age-related changes in the human body. Over the years, tissues and organs wear out. Heart tissue and urinary tract can be damaged due to hormonal changes, rapid slowdown of metabolism, etc.
- Life against the tide. Mitral valve prolapse and what is behind it
Mitral valve fibrosis can also be caused by the following reasons:
- Hypertension.
- Lung dysfunction.
- Heart defects.
- Infectious or viral infection of the connective tissues of the heart.
- Strong physical activity, etc.
This disease, in the absence of timely intervention by specialists, can develop into myocardial fibrosis. Otherwise it is called myocardiofibrosis.
Treatment and observation of a patient with fibrosis of the valve apparatus
Often on forums you can read the question of whether fibrosis can be treated using folk remedies. The answer is clear: there are no such recipes. This process is quite difficult in therapy even for modern medicine.
It is important to know that the prescription of medications is indicated only for the clinical picture of heart failure, in which the following are used:
- cardiac glycosides - Celanide, Digoxin, Strophanthin;
- diuretics - Trifas, Indap, Veroshpiron;
- if indicated, antihypertensive and antiarrhythmic drugs.
Medicines only minimize the symptoms caused by fibrosis without affecting the progression of the disease.
Radical treatment consists of the following methods:
valve prosthetics to replace the diseased structure with a mechanical or biological analogue. As a rule, a median sternotomy using a heart-lung machine is used;- mitral commissurotomy, closed or open, with the task of dissecting pathological connections between the valve leaflets;
- coronary artery bypass grafting;
- endovascular prosthetics. The essence of the method is to insert a catheter with an implant through the femoral vessels without general anesthesia. Indicated for patients with severe chronic diseases;
- valve transplantation (a relatively new technique).
Indications for surgical intervention in fibrosis:
- neglect of the process;
- wrinkling of valves, tendon threads;
- the presence of pronounced calcification.
After the operation, the patient should be under medical supervision of a cardiologist. The patient is indicated for annual examinations and treatment in a cardio- or cardio-rheumatological sanatorium.