Ischemia or coronary disease is a decrease or cessation of blood supply (blood circulation) in organs, the occurrence of “oxygen starvation” - hypoxia in them.
The cause of coronary artery disease is associated with vascular factors: atherosclerotic damage to blood vessels, narrowing, blockage of the lumen of arteries, compression of vessels from outside. If the heart, intestines, brain, kidneys or other organs encounter this problem, then such circumstances lead to temporary dysfunction or chronic damage to the organ or its individual tissues: for example, cardiac-type muscle tissue, kidney tissue.
Blockage, narrowing of blood vessels, and then the development of coronary artery disease can be caused by lipid metabolism disorders, thrombosis, blood diseases, injuries, vascular spasms, regularly high blood pressure, disturbances in blood glucose levels, excess body weight, end-stage renal failure, when filtration capacity kidney disease drops to its minimum, as well as hereditary predisposition: for example, among the causes of intestinal ischemia is hereditary microspherocytic (hemolytic) anemia.
Injuries, adhesions, neoplasms, and enlarged lymph nodes can cause compression of veins and arteries from the outside.
Classification
Depending on which organ is affected, the following types of ischemia are distinguished:
- Cerebral ischemia.
- Intestinal ischemia.
- Ischemia of the lower and upper extremities.
- Coronary heart disease (CHD).
- Renal ischemia.
According to clinical manifestations, various types of ischemia are distinguished:
- Angina pectoris (stable exertional angina, unstable angina, vasospastic angina, post-infarction angina). In the non-medical environment, this heart pathology is often known as “angina pectoris.”
- Myocardial infarction (death of the heart muscle). It can be large-focal or small-focal.
- Coronary syndrome, combining unstable angina and myocardial infarction. One of the most dangerous types of ischemia.
- Torpid (sluggish form) of renal nephropathy.
- Kidney infarction (acute nephropathy).
- Rapidly progressive nephropathy (renal infarction + renal failure).
- Ischemic stroke (cerebral infarction).
- Ischemic cerebral hypoxia (usually occurs with traumatic brain injury).
- Cerebral ischemia of newborns.
- Peripheral arterial disease of the lower extremities.
- Raynaud's disease. Impaired blood flow to the hands and fingers.
- Mesenteric intestinal ischemia (blockage of blood flow to intestinal vessels).
- Ischemia of the colon (ischemic colopathy, ulcerative ischemic colitis).
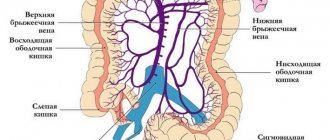
Anatomy of visceral circulation
The celiac trunk is the largest visceral artery with a diameter of about 8 mm. It departs from the aorta at the level of the XII thoracic vertebra in the area of the aortic opening of the diaphragm and is divided into 3 branches: the left gastric, the common hepatic and the splenic. The celiac trunk supplies blood to the liver, spleen, pancreas, stomach and the initial part of the duodenum.
The superior mesenteric artery arises from the aorta just below the celiac trunk, passes between the inferior border of the pancreas and the horizontal part of the duodenum, enters the mesentery of the small intestine and descends to the right iliac fossa. A number of branches extend from it. The first of them - the inferior pancreatic duodenal artery goes up behind the head of the pancreas and connects with the superior pancreatic duodenal artery. They supply the head of the pancreas and are the main collateral pathway between the celiac trunk and the superior mesenteric artery. From the left wall of the superior mesenteric artery, 10–16 branches extend to the jejunum and ileum. A series of larger ropes arise from the right wall of the superior mesenteric artery.
The inferior mesenteric artery departs from the aorta at the level of the lower edge of the third lumbar vertebra, goes behind the peritoneum down and to the left to the sigmoid colon. The left colic artery arises from it, which goes up to the left flexure and anastomoses with the descending branch of the middle colic artery, forming the arch of Riolan - the main collateral path between the systems of the superior and inferior mesenteric arteries.
Between the systems of the three unpaired branches of the aorta there is a network of fairly large anastomoses through which blood can move in any direction. Thanks to this, blood circulation in all three visceral arteries is interconnected and represents, as it were, a single vascular pool. With stenosis or occlusion of one or more arteries, the direction of blood flow along the collaterals changes. However, compensation for collaterals is not always complete.
Forms of ischemic disease (acute and chronic)
Acute ischemic disease is associated with blockages of arterial blood flow. Occurs when there is rapid blockage of blood vessels (usually large ones). It develops very rapidly, so other vessels simply do not have time to connect to the blood supply. The most famous acute forms are heart attack and stroke.
Chronic forms are pathologies that develop gradually. Most often, the disease develops due to constant compression of blood vessels and the proliferation of atherosclerotic plaques. In this case, auxiliary vessels actively try to compensate for the problem. They help supply the organs with oxygen, but the load on them increases, the performance of the organs decreases, and a number of unpleasant symptoms appear. For example, chronic ischemic heart disease is fraught with the development of heart failure, atrial fibrillation, and chronic cerebral ischemia negatively affects thought processes and is fraught with memory deterioration.
Causes
There are two large groups of ischemia that occur for specific reasons:
- Occlusive ischemic disease. The pathology is provoked by thrombosis of the veins and venous channels, thrombosis, embolism of the mesenteric arteries, when atypical bodies are present in the blood. Predisposing factors are:
- heart valve replacement surgery;
- heart defects;
- atrial tachyarrhythmia.
Thrombosis usually causes a reduction in the evacuation function of the heart and atherosclerosis. Blockage of the mesenteric veins is a rare phenomenon that occurs due to peritonitis, increased clotting factor, increased pressure in the portal vein, and inflammation of internal organs.
- Non-occlusive ischemic disease. Refers to frequent occurrences. Most likely reasons:
- abnormal heart rhythm (arrhythmia);
- arterial hypotension;
- cardiac dysfunction;
- taking a certain group of medications;
- dehydration.
There are also acute, caused by thrombosis, and chronic, caused by atherosclerosis, forms of ischemia.
Symptoms
- The following symptoms are characteristic of IHD: shortness of breath (in severe forms - both in motion and in a quiet position, in developing, chronic forms - in motion), rapid heartbeat, disruptions in blood pressure, pain in the chest, pain in the heart.
- Brain pathologies are characterized by deterioration of brain activity, and at the same time, memorization, concentration, the appearance of irritability, problems with sleep (in chronic forms), confusion, loss of vision, impaired sensitivity of the arms and legs, vomiting, nausea (in acute forms) .
- With ischemic intestinal pathologies, pain appears in the navel, upper abdomen, diarrhea, intestinal bleeding, bloating, tachycardia, abdominal tension, drop in blood pressure, diarrhea, vomiting.
- Symptoms of renal ischemia include frequent urge to urinate at night, severe swelling of the face, legs, arms, weakness, fatigue, and the smell of ammonia from the mouth.
- Symptoms of ischemic limb disease are intermittent claudication, a feeling of numbness in the arms and legs, a feeling that the arms and (or legs) are constantly cold, and ulcers on the legs. Patients also often notice that their nails begin to grow more slowly.
Very often (especially in chronic diseases, especially kidney pathologies), the symptoms are very “smeared” for a long time. Without a comprehensive diagnosis, a disease can easily be confused with another. In some patients, the symptoms affect only one organ, while in others the problem is more extensive, and there are problems with the heart, intestines, and kidneys at the same time.
Symptoms requiring immediate medical attention
Chronic intestinal diseases, such as diverticular disease, ulcerative colitis, Crohn's disease, polyps, if prolonged without proper treatment, can lead to life-threatening complications and cancer.
According to clinical guidelines, there are “alarm symptoms” or “red flag symptoms” that require an urgent visit to a doctor:
- unmotivated weight loss;
- diarrhea or abdominal pain at night;
- constant severe abdominal pain;
- onset of symptoms in old age;
- the appearance of mucus and blood in the stool;
- diarrhea lasting more than two weeks;
- episodes of constipation repeated within 2 months;
- blood relatives with inflammatory bowel disease or colon cancer.
Cerebral ischemia
Cerebral ischemia (dyscirculatory encephalopathy, cerebrovascular insufficiency) is a pathology that develops due to a lack of blood flow to the brain. The carotid artery, whose role is to supply blood to most parts of the brain, is especially affected.
Impaired blood flow leads to damage to nerve tissue. If nerve cells die, a stroke occurs.
The mechanism of development of the disease varies from person to person; some are immediately faced with an acute form of the disease, others with a chronic form of the pathology. Much depends on the specific vascular network. In some people, blocked vessels are compensated by neighboring ones, including smaller ones, while in others such compensation does not occur. Neuroses, allergic reactions, neoplasms, and infections can also increase the rate of cell death.
Consequences
Complications of the disease include pathological conditions such as:
- Necrosis or death of intestinal tissue. The necrotic process progresses in the complete absence of oxygen supply to cells. The pathology must be eliminated urgently and surgically. To do this, dead areas are removed and a colostomy is created (an opening in the abdomen for self-cleaning of the intestines, bypassing the anus).
- Narrowing of the intestines. During ischemia, tissue actively scars, which over time narrows the lumen of the organ. Surgery is needed to correct the defect.
Intestinal ischemia
Intestinal ischemia refers to a whole group of diseases that are caused by both chronic and acute processes. But all pathologies are united by a common factor. This is a decrease in blood flow to the gastrointestinal tract and directly to the intestines.
Mesentral embolic ischemia poses a great danger. It comes suddenly. It is characterized by a “sharp belly.” Without the use of comprehensive diagnostic tools, symptoms can be confused with symptoms of acute pancreatitis, appendicitis, or perforated ulcers. But the nature of this pathology is different - a sudden formation of obstruction (occlusion) in the mesenteric vessel - tissue that is involved in attaching the intestine itself to the abdominal wall. This may be a response to infection, injury, blood diseases, portal hypertension - increased pressure in the portal vein, taking certain medications (for example, contraceptives). If the pathology is not promptly diagnosed and measures are not taken, the intestinal walls may begin to necrosis (die).
Another type of pathology is ischemia following mesentral thrombosis (thrombosis of mesenteric vessels). It is characterized by intense, cramping pain. At the initial examination, the symptoms are similar to intestinal colic and intestinal obstruction. But again, the further prognosis depends on the speed of diagnosis. As a rule, the problem is solved by diagnosis and resection. If they are not done on time, death is likely in 70-90% of cases.
But the most common option is colonic ischemia, which develops against the background of vascular atherosclerosis, aortic dissection or the presence of an aneurysm. The disease is accompanied by severe exhaustion. 80% experience weight loss.
Mesenteric venous thrombosis
This condition develops against the background of blockage of a vein by a blood clot. The veins come from the intestinal tissues, therefore, when they are blocked, the blood does not find a way out of the organ. As a result, blood accumulates in the vessels, their walls thicken. Bleeding may occur in this area. Causes:
- infection of the peritoneum;
- severe abdominal injury;
- tumor formation in the gastrointestinal tract;
- certain types of hormonal treatments;
- intestinal inflammation such as Crohn's disease, diverticulitis, ulcerative colitis;
- pathologies that prevent the formation of blood clots.
Limb ischemia
Rarely occurs on its own. More often – a manifestation of obliterating atherosclerosis. Deposition of LDL (“bad” cholesterol) on the walls of blood vessels and atherosclerotic plaques provoke blocking and narrowing of the arteries. Blood cannot fully move through the arms and legs.
In the initial stages, we are talking purely about discomfort (hands and feet are constantly cold). Then cracks in the skin and trophic ulcers appear. With advanced disease, there is a high risk of necrosis and gangrene.
A significant breakthrough in the diagnosis of the disease began with the widespread use of duplex scanning of veins and arteries. Timely diagnosis allows you to start treatment as early as possible and avoid amputation of legs and arms.
Diagnostic program for abdominal ischemia
Diagnosis of the disease must take into account the patient's symptoms and have a combined approach. The doctor clarifies the patient’s complaints, asks about the time of their occurrence and characteristics. To assess the function of the abdominal vessels, auscultation is performed - that is, listening to noises. They can occur when the celiac and mesenteric arteries are narrowed. Sometimes phonoenterography is used - this is an image of vascular murmurs on a graph.
Research methods used for abdominal toad
- vascular angiography, which will confirm or exclude the presence of stenosis and occlusion;
- plain radiography of the abdomen, which can determine calcification of the aortic walls;
- endoscopic studies that will help visualize changes in the mucous membrane, erosion, ulcers;
- analysis of feces will show digestive disorders, in which the amount of mucus and undigested particles in the feces is increased.
Also, methods such as scintigraphy, ultrasound duplex scanning, ultrasound of the abdominal organs, and flowmetry are used. Sometimes, in the process of diagnosing abdominal ischemia, diagnoses are made: gastritis, peptic ulcer, cholecystitis, pancreatitis.
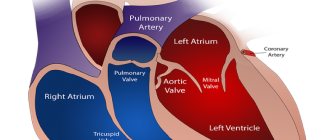
Cardiac ischemia (CHD)
IHD is an acute or chronic disorder of the blood supply to the muscle tissue of the heart - the myocardium. The mechanism of coronary artery disease is triggered when the coronary arteries are damaged, arterial blood is unable to flow to the heart or goes there in limited quantities.
IHD is one of the main factors of mortality; IHD accounts for 30% of all deaths in the world. Including sudden coronary death (sudden cardiac arrest)
More often, people aged 40–65 years suffer from ischemic heart disease. Men suffer from ischemic heart disease more often than women.
Those at greatest risk are those who abuse smoking (due to constant narrowing of blood vessels), fatty foods (higher risk of plaque formation), and people with high levels of LDL (“bad” cholesterol), which narrows the lumen in the blood vessels. Constant worries and stress are also dangerous (like smoking, they can cause vasoconstriction).
But with the development of diagnostics and treatment methods, the number of deaths is decreasing, life expectancy in chronic patients is increasing, and the quality of life is improving.
Thanks to modern functional diagnostic equipment and the development of laboratory diagnostics, it is possible to identify even asymptomatic forms of IHD at an early stage.
Modern methods of treating abdominal ischemia
In the early stages of the disease, conservative therapy is used. it involves modification of eating habits. Patients are advised to eat small portions and also avoid rough foods and foods that stimulate the production of gases. Medication assistance consists of taking antispasmodics that expand the lumen of the vessel, anticoagulants, and blood circulation stimulants. Such assistance is sufficient at the compensation stage. Regular use of medications and compliance with recommendations will prolong the compensation stage.
For subcompensated and decompensated abdominal ischemia, surgical intervention is indicated. This can be a conditionally reconstructive operation - impact on the legs of the diaphragm, removal of cords. Reconstructive surgery - decompression, vascular bypass. their dilatation and stenting. Minimally invasive intervention on the vessels of the abdominal cavity - angioplasty and stenting). Surgical and minimally invasive treatment methods ensure the restoration of blood supply to the suffering organ. expansion of the lumen of the vessel, and installation of a stent is the prevention of relapse of the disease. The operation is performed under anesthesia. Modern techniques allow it to be carried out in a short time and with minimal trauma.
Diagnosis of coronary disease
The main diagnostic measures are aimed at examining the vessels of a particular organ directly. Auscultation of blood vessels with a stethoscope is performed (to detect noise), Doppler ultrasound (USDG) of arteries and veins, CT scan of the examined area, ultrasound, including the brachiocephalic arteries (the main arteries of the brain). Modern methods make it possible not only to study and detect the lumen of blood vessels, but also to examine its walls.
Laboratory diagnostics are of no small importance: general blood test, hemostasiogram, biochemical blood test: lipid spectrum, urea, creatinine, total protein, electrolyte metabolism (potassium, sodium chlorine) are especially important.
If kidney damage is suspected, extended urine tests are relevant: a general urine test according to Nechiporenko, a Rehberg test to determine the glomerular filtration rate, a Zimnitsky test to analyze the concentration and excretory capacity of the kidneys.
When diagnosing the limbs, the calculation of the ankle-brachial index is of great importance (it is important not to miss the difference in blood pressure on the lower leg and on the shoulder).
For ischemic heart disease and ischemic stroke, Holter-ECG is prescribed, and for problems with cerebral vessels, electroencephalography is prescribed.
Operation
Several techniques are used:
- Bypass surgery to bypass the blocked area with removal of the necrotic part of the wall or thrombus. The shunt can be made in the form of a synthetic prosthesis or made from the patient's femoral vein.
- Angioplasty with bypass to widen the narrowed area.
- Transaortic endarterectomy with removal of atheromatous plaques through the abdominal cavity.
- Stenting with the installation of a stent (wire cylinder) at the site of narrowing, which prevents re-narrowing. The technique can be used as an adjunct to angioplasty.
After intestinal surgery, treatment is carried out with medications.
Treatment of coronary disease
Medicinal and surgical methods are used for treatment. Among medications, an important role is played by medications that normalize and maintain blood pressure. This is important regardless of what is in the area of attention - the heart, kidneys or blood vessels of the legs.
Among the actively used drugs for ischemia of various types are drugs that allow you to quickly dilate blood vessels. These include, for example, the well-known nitroglycerin - an indispensable assistant during attacks with ischemic heart disease.
If the cause is thrombosis, drugs aimed at reducing blood viscosity are necessarily used.
As for surgical intervention, it all depends on the pathology of a particular organ.
In case of coronary artery disease, coronary artery bypass surgery is performed (installation of prostheses to bypass the site of narrowing of the coronary vessel), myocardial revascularization (actually a type of bypass surgery on a beating heart), stenting of the coronary arteries - installation of special stents. This could be an absorbable balloon, a metal stent, or a medicated stent. The task of any of them is to prevent repeated narrowing of the lumen of the vessel - stenosis.
In case of cerebral ischemia, blood flow in the vessels is most often surgically restored by shunting. The operation allows you to redirect the blood, “circle” it around the blockage, and preserve or restore blood supply to the brain.
In case of ischemic pathologies of the kidneys and intestines, resection is used as a surgical method to solve the problem. The most gentle for the body is laparoscopic resection.
Physiotherapy, exercise therapy, including exercise on exercise bikes, and hypobaric oxygenation in pressure chambers are also important. The role of oxygenation in pressure chambers is especially important in rehabilitation after ischemic stroke.
Clinical manifestations
Clinical manifestations of small intestinal pathology caused by vascular pathology have similar symptoms. This is explained by the fact that the basis for damage to the small intestine in these diseases is predominantly ischemia of the intestinal wall.
Acute ischemia. The main causes of acute ischemia of the small intestine can be embolism of the superior mesenteric artery, thrombosis of the mesenteric veins and arteries, and non-occlusive mesenteric ischemia.
Embolism of the superior mesenteric artery. The superior mesenteric artery supplies the entire small intestine, cecum, ascending colon, and part of the transverse colon.
The causes of embolism are most often diseases of the cardiovascular system, primarily atherosclerosis, as well as heart defects, endocarditis, myocardial infarction, portal vein thrombosis, thrombophlebitis of peripheral veins. The sources of embolism can be blood clots in the left cavities of the heart. Depending on the speed of development of arterial obstruction, the prevalence of thrombosis, the size of the intestinal infarction, and concomitant diseases, the onset can be acute or gradual, sometimes in two stages (the appearance of pain, its weakening and reappearance). A painless onset is also possible.
Abdominal pain is the main symptom of this pathological condition. It is characterized by particular sharpness, persistence, and is difficult to tolerate. At the beginning of the disease, the pain has an intermittent, cramping character, and then becomes more uniform, constant, and its intensity does not decrease. The pain may be less severe or absent. Nausea and vomiting are observed almost constantly, often mixed with blood. Constipation or diarrhea develop, and stool is often mixed with blood. During palpation in the first hours, the abdomen is usually soft, slightly swollen, no muscle protection is noted, the abdominal wall is involved in breathing, and the pain is mild. Subsequently, as necrotic changes occur in the intestinal wall, peritonitis develops.
Thrombosis of the superior mesenteric artery. Its most common cause is widespread atherosclerosis. The clinical picture of thrombosis of the superior mesenteric artery is for the most part similar to the previously described embolism clinic. But there are some differences - abdominal pain is less intense and is not cramping in nature. Mesenteric thrombosis may remain latent for some time. But as ischemia increases, the clinical picture also increases, intestinal infarction develops, and then peritonitis.
Non-occlusive mesenteric ischemia. The most common cause of non-occlusive mesenteric ischemia is heart failure of various etiologies.
The clinical picture of this type of ischemia is similar to that of embolism or thrombosis of the superior mesenteric artery. However, the severity of clinical manifestations is much less, including pain. Characterized by diarrhea, rumbling in the stomach, flatulence, weight loss.
Thrombosis of mesenteric veins. Thrombosis of the mesenteric veins can develop without any reason, although more often it occurs after trauma to the abdominal cavity, with purulent processes in the abdominal cavity, cirrhosis of the liver with portal hypertension, with neoplasms, acute pancreatitis, and in severe stages of chronic circulatory failure.
Thrombosis of the mesenteric veins is accompanied by damage to the intestinal wall, which, depending on the degree of blockade, ranges from more or less widespread edema to necrosis and perforation of the intestinal wall. The most severe form of damage is intestinal infarction of venous origin.
The clinical picture of mesenteric vein thrombosis is the same as for arterial thrombosis, but appears more slowly. Severe symptoms are observed with the development of intestinal infarction: abdominal pain, diarrhea, nausea, vomiting, bloating, unexpressed muscle protection.
Chronic ischemia. Obstruction of the visceral arteries that slowly progresses over a long period of time can lead to the development of collateral circulation and is not accompanied by severe disorders and does not manifest clear symptoms. Thanks to compensatory mechanisms that redistribute blood flow in the intestinal wall, intestinal functions remain normal almost until the moment when the damage becomes irreversible. Collateral circulation ensures that even with complete occlusion of the visceral arteries in the intestine, symptoms of vascular insufficiency do not occur. However, as arterial inflow further decreases, ischemia of the intestinal muscle layer and associated pain occurs because blood flow becomes insufficient to support the increased peristalsis caused by food intake. Blood circulation in the mucous membrane remains normal for some time, and the absorptive function of the intestine is not impaired. With further progression of the process, blood flow decreases below the level necessary to protect the mucous membrane from bacterial damage, and focal or massive infarction develops.
Clinical manifestations of chronic ischemia of the small intestine are diverse. This is explained by the fact that the clinical picture of this condition is similar to the clinical manifestations of a number of diseases.
In most patients, the main symptom is pain. A distinctive feature of pain syndrome in chronic intestinal ischemia is its clear connection with food intake. With a severe attack, sharp convulsive (burning, cutting) pain appears in the abdomen (mainly in the epigastric region). Pain usually occurs at the height of digestion (no earlier than 15–30 minutes or later after eating) and lasts for 1–3 hours. The pain may also be more short-term (from 1–2 to 15–20 minutes). It is not associated with physical stress, is localized in the abdominal area, and does not radiate. At the initial stage of the disease, pain can be relieved with nitrates and antispasmodics. Initially, pain appears only after a heavy or evening meal, then it becomes a constant symptom, so patients abstain from eating (symptom of “fear of food”).
An attack of pain is accompanied by bloating, constipation, and often belching. In the future, along with pain and flatulence, foul-smelling diarrhea may occur 2-3 times a day. Feces contain undigested food particles and unabsorbed fat. The urge to defecate occurs soon after eating and follows every meal.
Progressive weight loss is associated both with the refusal of patients to eat due to pain, and with a violation of the secretory and absorption functions of the small intestine. In patients, the pulse quickens and blood pressure often increases.
Due to meteorism, the diaphragm is high. The abdominals are tense. Auscultation of the abdomen can often reveal a characteristic systolic murmur, determined at a point located 2–4 cm below the xiphoid process in the midline (from gentle blowing to rough scraping, low timbre), and increased bowel sounds after eating. With severe stenosis or occlusion of the visceral arteries, systolic murmur may be absent. The most informative is auscultation with the patient lying down, on an empty stomach and on exhalation. It is also advisable to carry it out with the patient standing and squatting, because with extravasal compression of the celiac trunk in this position, a noise may appear above its projection.
Mild, but long-term forms of mesenteric circulation failure lead to temporary ischemia of the tissues of the walls of the small intestine, the development of symptoms of atony and flatulence. Mesenteric insufficiency increases during periods of increased digestive function, often accompanied by a variety of dyspeptic symptoms. As a result of malnutrition of the intestinal wall (constant, but moderate, with periods of intensification), the secretory and enzymatic activity of the glands, motor and evacuation functions change, which leads to the appearance of the above complaints.
Damage to the small intestine due to vasculitis. Involvement of the gastrointestinal tract (GIT) in the pathological process in vasculitis most often represents part of a systemic process. Most often, vasculitis of the gastrointestinal tract develops with polyarteritis nodosa, Churg-Strauss syndrome, Henoch-Schönlein purpura, and Takayasu arteritis. Symptoms of gastrointestinal tract damage in systemic vasculitis are caused by mesenteric ischemia. The onset of clinical symptoms may be acute and severe (eg, mesenteric infarction) or chronic (with gradual development of mesenteric ischemia). Chronic mesenteric ischemia can manifest with a variety of symptoms. Acute symptoms of small bowel obstruction may occur due to strictures similar to those in Crohn's disease, or intussusception, or massive gastrointestinal bleeding. Signs of damage to the gastrointestinal tract are similar to each other, regardless of the systemic vasculitis that caused them. For successful diagnosis, attention should be paid to individual specific syndromes.
Polyarteritis nodosa is a systemic necrotizing vasculitis of the type of segmental damage to small and medium-sized arteries with the formation of aneurysmal protrusions. Mostly men aged 30–40 years are affected. The disease begins with general symptoms, among which are fever, progressive weight loss (30–40 kg over several months) and muscle-joint pain. However, sometimes, already at the beginning of the disease, clear signs of damage to internal organs, including the gastrointestinal tract, appear.
Abdominal syndrome is the second most common and prognosis disease. Morphologically, it is characterized by acute vascular ulcers of the intestine (usually the small intestine) or stomach with perforation and bleeding; Thrombosis of mesenteric vessels, infarction of the pancreas, liver, and spleen are possible. Clinically, pain and dyspeptic symptoms are noted. The pain is diffuse, prolonged, persistent, and increasing in intensity. Diarrhea (up to 6–10 times a day) mixed with mucus and blood is often observed. Characterized by anorexia, sometimes nausea, vomiting. When the ulcer perforates, peritonitis develops. Bleeding is possible.
Churg-Strauss syndrome (allergic granulomatosis and angiitis) is a disease that affects various systems and organs, which is characterized by a triad of symptoms: allergic rhinitis, bronchial asthma and severe eosinophilia.
The most common type of gastrointestinal lesion in Churg-Strauss syndrome is eosinophilic gastroenteritis, characterized by:
— abdominal pain (up to 60% of cases);
- diarrhea (up to 33% of cases);
- gastrointestinal bleeding (up to 20% of patients);
- colitis.
Symptoms of damage to the gastrointestinal tract can either precede the vasculitic phase of the disease or develop simultaneously with its other symptoms.
Henoch-Schönlein purpura (hemorrhagic vasculitis) is a systemic inflammatory disease of predominantly capillaries, arterioles and venules, mainly the skin, joints, abdominal cavity and kidneys. The disease most often develops in children, but can debut at any age. The most characteristic symptom of the disease is a skin papular hemorrhagic rash located symmetrically on the lower extremities, buttocks and, less often, on the torso. The second symptom is articular syndrome, manifested by intermittent pain and swelling of predominantly large joints. The gastrointestinal tract is affected in half of the patients.
Abdominal syndrome, resulting from hemorrhage into the intestinal wall or mesentery, is one of the most severe manifestations of hemorrhagic vasculitis. In approximately 35% of patients, it predominates in the clinical picture of the disease, and sometimes precedes skin rashes, which complicates diagnosis. Patients are bothered by cramping abdominal pain similar to intestinal colic (usually around the navel), bloody vomiting, and sometimes intestinal bleeding, often simulating acute surgical diseases of the abdominal cavity. Purpuric lesions may be visualized on endoscopic examination, most commonly in the duodenum, stomach, and colon (Figure 1).
The pain may wax and wane over several weeks and often resolves on its own. The most common gastrointestinal complication of Henoch-Schönlein purpura is intussusception, which in 60% of cases is limited to the small intestine (with idiopathic intussusception, ileocolic intussusception predominates). Rarer complications include acute pancreatitis, gallbladder disease, colonic perforation and, in children, protein-losing enteropathy.
Takayasu arteritis is a systemic disease characterized by inflammatory and destructive changes in the wall of the aorta and its branches, which are accompanied by stenosis and organ ischemia; 80–90% of cases develop in women, usually between the ages of 10 and 40 years.
The basis for damage to the gastrointestinal tract in Takayasu arteritis is chronic mesenteric ischemia. Thanks to the developed system of collaterals (between the celiac trunk, the superior and inferior mesenteric arteries), the clinical manifestation of mesenteric ischemia develops only in the case of occlusion or subtotal stenosis of two of the three arterial trunks supplying the intestine. Clinically, the lesion is manifested by abdominal sore throat: diffuse postprandial (arising after eating) pain, loss of body weight, loss of appetite; Abnormal bowel movements and nausea are rare.
Damage to the small intestine in diffuse connective tissue diseases. Systemic scleroderma (SSc) is a systemic disease of connective tissue and small vessels, characterized by widespread fibrosclerotic changes in the skin, stroma of internal organs and symptoms of obliterating endarteritis. The clinical picture of SSc is characterized by polysyndromy, a combination of signs of fibrosis and generalized endarteriolitis. One of the earliest and most persistent signs of SSc is Raynaud's syndrome. Scerodermic skin lesions are characteristic.
Early signs include damage to the gastrointestinal tract. The esophagus is affected in almost all patients. Changes associated with the development of smooth muscle atrophy and/or submucosal fibrosis are also observed in the small intestine. Damage to the small intestine is accompanied by bloating, distension, pain, and as the disease progresses, the development of malabsorption syndrome, diarrhea and weight loss.
Complication
Intestinal ischemia is fraught with the formation of strictures (narrowing of intestinal sections). And a number of patients may develop short bowel syndrome, which results in fear of eating.
The most serious risk with renal ischemia is complete occlusion of blood vessels and blockage of blood vessels. The main danger is the cessation of excretion of waste products from the body. The result is complete kidney failure, which can be fatal.
Serious consequences and complications are possible if coronary brain disease is not taken under medical control in a timely manner. Damage to brain tissue is fraught with limitation of motor activity (up to paralysis), loss of mental abilities, loss of legal capacity and disability.
Comprehensive rehabilitation helps to effectively reduce the risk of complications. For example, a special program “Rehabilitation after ischemic stroke” is available at hospital No. 5. The two-week course includes consultations, a comprehensive examination, individual exercise therapy, physiotherapy, drug therapy, massage, and acupuncture.
Risk factors
Common provoking factors for the development of intestinal ischemia are:
- diabetes mellitus, hypercholesterolemia syndrome, high blood pressure, smoking, old age, which cause atherosclerosis;
- strong pressure deviations below/above normal;
- cardiac dysfunctions such as arrhythmia, chronic failure;
- drug abuse;
- clotting factor impairment in antiphospholipid syndrome, hereditary hemoglobinopathy.
Forecasts
Despite the fact that ischemia is a very serious disease, timely medicine allows us to do everything to ensure the most favorable prognosis.
The sooner an accurate diagnosis is made to the patient and a treatment regimen (medical, surgical) is selected, the higher the likelihood of a successful result.
Even with the most complex brain pathologies, with timely help, it is possible to preserve the maximum number of nerve cells, which means preserving or restoring the functions of the body.
Of great importance is how patient care is provided during the treatment process (especially after surgery). It is important to ensure that the patient has the correct body position, nutritional regimen, and catheter care. Massage helps significantly speed up recovery.
The 5th hospital has an experienced team of specialists: including neurologists, neurosurgeons, surgeons, and cardiologists. The clinical diagnostic laboratory, the RK and MRI department, the department of clinical and functional diagnostics are equipped with high-quality equipment, with the help of which high-precision studies can be quickly carried out. Here you will receive competent assistance for coronary heart and cerebral vascular disease. Treatment and rehabilitation programs are available for both citizens of the Republic of Belarus and foreign citizens. The doctors at Hospital No. 5 have extensive experience treating patients from Moscow and other Russian cities.
Features of the postoperative period
After the operation, the patient is under the supervision of medical personnel for some time. The state of health and digestion processes are gradually normalized. In the early period after surgery, it is recommended to take medications and correct the condition after anesthesia.
If the patient has a stent installed, anticoagulant and antiplatelet drugs are indicated, which are necessary to prevent thrombus formation.
In order to evaluate the result of treatment, the attending physician conducts a study of the condition of the blood vessels and observes the patient over time. It is necessary to attend prescribed consultations and studies, as there is a risk of relapse of the pathology.
In order to receive treatment, you must consult a doctor. After the diagnostic methods have been carried out and an accurate diagnosis has been made, the doctor will, if necessary, set a date for intervention.