Bleeding stops on its own in approximately 80% of cases. Continued bleeding requires stopping it endoscopically as soon as possible. If this is not possible, then resort to active surgical tactics. In some cases, endovascular intervention or conservative treatment is performed.
The main tasks assigned to an anesthesiologist-resuscitator in the treatment of patients with gastrointestinal tract:
- Carrying out the prevention of recurrent bleeding after it has stopped;
- Restoration of systemic hemodynamics and other indicators of homeostasis. Naturally, the volume of assistance provided can vary widely: from resuscitation measures to simple dynamic monitoring of the patient;
- Providing assistance during endoscopic intervention or surgical intervention (if necessary);
- Timely detection of recurrent bleeding;
- In relatively rare cases, conservative treatment of bleeding is performed.
Sequence of assistance
If the patient received anticoagulants before bleeding occurred, they should, in most cases, be discontinued. Assess the severity of the condition and the estimated amount of blood loss based on clinical signs. Vomiting blood, loose stools with blood, melena, changes in hemodynamic parameters - these signs indicate ongoing bleeding. Arterial hypotension in the supine position indicates large blood loss (more than 20% of the blood volume). Orthostatic hypotension (a decrease in systolic blood pressure above 10 mm Hg and an increase in heart rate by more than 20 beats per minute when moving to a vertical position) indicates moderate blood loss (10-20% of blood volume);
In the most severe cases, tracheal intubation and mechanical ventilation may be required before endoscopic intervention. Provide venous access with a peripheral catheter of sufficient diameter (G14-18); in severe cases, install a second peripheral catheter or perform catheterization of the central vein.
Take a sufficient volume of blood (usually at least 20 ml) to determine the group and Rh factor, combine blood and conduct laboratory tests: general blood count, prothrombin and activated partial thromboplastin time, biochemical parameters.
Symptoms: how to recognize the presence of pathology
Any first aid - pre-medical or medical - cannot be provided to a patient until the presence of specific symptoms of pathology has been established, the degree of damage and the level of its threat to life have not been determined.
General symptoms of gastrointestinal bleeding are represented by the following manifestations:
- weakness, severe dizziness;
- increased sweating;
- darkening of the eyes;
- cooling the extremities;
- blanching of the skin and mucous membranes.
However, a characteristic sign that allows one to identify a specific type of bleeding is the admixture of blood in the stool, as well as in the vomit. At the same time, blood in the stool may be present in a changed or unchanged form.
Infusion therapy
Begin infusion therapy with the introduction of balanced salt solutions.
Important! If there are signs of ongoing bleeding or unstable hemostasis has been achieved, blood pressure should be maintained at the minimum acceptable level (SBP 80-100 mm Hg), i.e. infusion therapy should not be too aggressive. Blood transfusions are carried out if adequate infusion therapy fails to stabilize the patient’s hemodynamics (blood pressure, heart rate). Consider the need for blood transfusion:
– when the hemoglobin level decreases below 70 g/l. when bleeding has stopped;
– with ongoing bleeding, when hemoglobin is below 90-110 g/l.
In case of massive blood loss (more than 50-100% of the blood volume), transfusion treatment is carried out in accordance with the principles of “Hemostatic resuscitation”. It is believed that each dose of packed red blood cells (250-300 ml) increases hemoglobin levels by 10 g/l. Fresh frozen plasma is prescribed for clinically significant coagulopathy, including drug-induced coagulopathy (for example, the patient is receiving warfarin). And in case of massive blood loss (>50% of blood volume). If reliable hemostasis is achieved, there is no need to administer FFP even with significant blood loss (more than 30% of the blood volume). Dextrans (polyglucin, rheopolyglucin), hydroxyethyl starch (HES) solutions may increase bleeding and their use is not recommended.
Antisecretory therapy
Optimal conditions for the implementation of vascular-platelet and hemocoagulation components of hemostasis are created at pH > 4.0. Proton pump inhibitors and H2-histamine receptor blockers are used as antisecretory drugs.
Attention! It is not advisable to prescribe H2-histamine receptor blockers and proton pump inhibitors at the same time.
Medicines of both groups suppress the production of hydrochloric acid in the stomach and thereby create conditions for stable hemostasis of the bleeding vessel. But proton pump inhibitors show more consistent results in reducing gastric acidity and are significantly more effective in reducing the risk of recurrent bleeding. The antisecretory effect of proton pump inhibitors is dose-dependent. Therefore, the use of high doses of drugs is currently recommended, so the prescription regimens indicated below are not a typo by the author.
Patients are prescribed an intravenous infusion of one of the following proton pump inhibitors:
- Omeprazole (Losec) 80 mg IV as a loading dose, followed by 8 mg/hour.
- Pantoprazole (Controloc) 80 mg IV as a loading dose, followed by 8 mg/hour.
- Esomeprazole (Nexium) 80 mg IV as a loading dose, followed by 8 mg/hour.
The loading dose of the drug is administered in approximately half an hour. Intravenous administration of the drug is continued for 48-72 hours, using, depending on possibilities, a bolus or continuous route of administration. In the following days, they switch to oral administration of the drug at a daily dose of 40 mg (for all of the proton pump inhibitors listed in this paragraph). The approximate duration of the course is 4 weeks.
Attention. The administration of proton pump inhibitors should be started before endoscopic intervention, as this reduces the likelihood of recurrent bleeding.
In the absence of proton pump inhibitors, or patients intolerant of them, intravenous H2-histamine receptor blockers are prescribed:
- Ranitidine 50 mg IV every 6 hours or 50 mg IV followed by 6.25 mg/hour IV. After three days, 150-300 mg orally 2-3 times a day;
- Famotidine 20 mg IV drip every 12 hours. Orally for treatment use 10-20 mg 2 times/day or 40 mg 1 time/day.
First aid for ulcer bleeding
In 5-15% of patients suffering from erosion of the gastric mucosa, sooner or later ulcerative bleeding begins, the intensity of which directly depends on the size of the damaged vessel. Bleeding occurs suddenly, regardless of the degree and severity of the pathology. Most often, bleeding is preceded by symptoms of exacerbation of a peptic ulcer: pain in the epigastric region (especially when hungry and at night), nausea and vomiting (especially after eating), heartburn. But it happens that bleeding occurs against the background of a completely satisfactory state of health of the patient. The bleeding itself, if it is minor, can also occur without obvious signs. It all depends on its intensity. If severe weakness, cold sticky sweat, pale skin, rapid pulse, and cold extremities are observed, this indicates a serious degree of blood loss. A striking symptom is bloody vomiting, the vomit has the appearance of “coffee grounds.” With a degree of blood loss of 25-45%, hemorrhagic shock develops: blood pressure decreases, the amount of urine excreted sharply decreases, shortness of breath appears, and the patient is agitated. Blood loss of 50 percent or more of the volume of blood circulating in the body poses a serious danger to the patient’s life. In this case, the skin acquires a waxy tint, lips are bluish, the pulse is thready, the patient notices flashing “floaters” before the eyes, tinnitus, dizziness, and often loses consciousness. Attention! Minor ulcer bleeding can become massive and life-threatening within a few hours. In case of ulcerative bleeding, emergency care is the main condition not only for maintaining health, but also life. How to provide first aid to a patient : first of all, you need to lay him in a horizontal position on his back with his legs raised 10-15º and urgently call an ambulance! Then, to constrict blood vessels and reduce bleeding, place a heating pad with cold water or a plastic bag with ice (or frozen foods) on the patient’s stomach. You can also give the patient a small piece of ice to swallow; the cold stops the bleeding. If the patient has lost consciousness, but has a pulse and breathing, observe the basic functions - monitor the pulse and breathing. If blood circulation and (or) cardiac activity stops, begin resuscitation measures - artificial respiration and chest compressions. What you should absolutely not do : give him water, allow him to get up, walk, take painkillers. The patient is transported to the ambulance on a stretcher. As a rule, such patients are taken to the surgical department to provide timely and emergency care. Any surgical intervention is stressful for the body, so contact your doctor in time, follow all their recommendations and try to prevent the formation of stomach and duodenal ulcers. If you already have such an ulcer, then it must be treated so that complications do not arise in the form of ulcerative bleeding or perforation. Listen carefully to your feelings and, at the slightest suspicion of bleeding, seek medical help immediately. Alexander Vladimirovich Sumarokov, director, surgeon of the highest category at Alanda Surgery. You can make an appointment and ask all your questions by calling: +7, 47-98-89, 47-98-90.
Preparation for gastroscopy
After relative stabilization of the patient’s condition (SBP more than 80-90 mm Hg), it is necessary to conduct an endoscopic examination, and, if possible, determine the source and stop the bleeding.
The following procedure can facilitate gastroscopy against the background of ongoing bleeding. 20 minutes before the intervention, the patient is given intravenous erythromycin by rapid infusion (250-300 mg of erythromycin is dissolved in 50 ml of 0.9% sodium chloride solution and administered over 5 minutes). Erythromycin promotes rapid evacuation of blood into the intestine, and thereby facilitates the identification of the source of bleeding. With relatively stable hemodynamics, 10 mg metoclopramide is used intravenously for the same purposes.
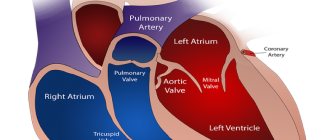
In patients with valvular heart disease, antibiotic prophylaxis is recommended before performing gastroscopy. Sometimes, to remove blood clots from the stomach (to facilitate endoscopic examination), a large-bore gastric tube (24 Fr or larger) must be inserted. It is recommended to lavage the stomach with water at room temperature. After the procedure is completed, the probe is removed.
Using a gastric tube for the purpose of diagnosing and controlling bleeding (if endoscopic examination is possible), in most cases, is considered inappropriate.
General characteristics of the pathology, reasons for its formation
Content:
- General characteristics of the pathology, reasons for its formation
- Symptoms: how to recognize the presence of pathology
- Types of gastrointestinal bleeding according to their severity
- First aid rules
Gastrointestinal bleeding is a condition that in gastroenterology is considered one of the most common, along with gastritis, pancreatitis, and appendicitis.
The source of bleeding can be localized in any part of the gastrointestinal tract, so for convenience, doctors divide them into upper (from the upper parts of the digestive organs, namely the esophagus, stomach and duodenum), and lower bleeding (from the small and large intestines, rectum) , and the first type occurs in 80-90% of all cases. In addition, bleeding can be ulcerative and non-ulcerative, chronic and acute, one-time and recurrent.
Most often, the pathology affects men, as well as people over 45-50 years of age. In women and young people, this type of lesion is detected less frequently. Approximately 9% of all people admitted to medical institutions for hospitalization are there due to bleeding from the digestive tract.
As for the causes of bleeding, they include various diseases of internal organs, the vascular system, bacterial lesions, and many others. There are more than a hundred such reasons in total. All etiological prerequisites for the appearance of pathology are divided into several groups.
The first includes diseases of the gastrointestinal tract. The second is represented by vascular damage. Portal hypertension is indicated as a separate group. Another group of causes of gastrointestinal bleeding are blood diseases.
The division of bleeding into ulcerative and non-ulcerative just belongs to the first group. Of these, the most common are:
- stomach and duodenal ulcers;
- esophagitis in chronic form;
- reflux esophagitis;
- nonspecific ulcerative colitis.
The development of peptic ulcers, and therefore bleeding, is influenced by stress, long-term use of certain types of medications, and problems in the functioning of the endocrine system.
Non-ulcer bleeding from the intestinal and gastric mucosa can be caused by erosions, diverticulosis, anal fissures and hemorrhoids, diaphragmatic hernia, benign and malignant tumors in the gastrointestinal tract, parasitic lesions, inflammatory processes, and some infectious diseases.
Bleeding can also cause the following vascular disorders:
- atherosclerosis;
- systemic lupus erythematosus;
- hemorrhagic vasculitis;
- periarteritis nodosa;
- phlebeurysm.
As for portal hypertension, it is one of the most dangerous complications of liver cirrhosis, hepatitis, thrombosis of the hepatic and portal veins.
Blood diseases that are among the causes of gastrointestinal bleeding:
- acute and chronic leukemia;
- aplastic anemia;
- hemophilia;
- von Willebrand's disease.