Gastrointestinal bleeding is the loss of blood from damaged blood vessels in the walls of the digestive tract or in its immediate vicinity when bleeding occurs into the lumen of the gastrointestinal tract. The source of bleeding can be any part of the digestive tract, from the pharynx to the rectum.
Bleeding can have many different causes and clinical progression depending on the rate and amount of blood lost, as well as the general condition, especially concomitant diseases.
Types of gastrointestinal bleeding
The content of the article
The severity of bleeding can range from microscopic blood loss to massive bleeding with the release of large amounts of blood (usually a mixture of blood, clots, and possibly hematin) through the mouth or anus, which can lead to hypovolemic shock and death.
Microscopic blood loss can only be detected in stool using specialized laboratory tests. The condition can also be identified by the results of peripheral blood tests and decreased iron levels.
Gastrointestinal bleeding is divided into:
- Bleeding from the upper gastrointestinal tract
. Their source is between the pharynx and the ligament of Treitz (duodenal ligament). They are involved in 80% of cases of gastrointestinal bleeding; - Gastrointestinal bleeding from the lower gastrointestinal tract
. Their source is between the ligament of Treitz and the rectum; - Hidden gastrointestinal bleeding
. This form differs from ordinary bleeding in its clinical picture and requires specific diagnostic procedures.
Classification
Peritonitis is of the following types:
- bacterial – caused by microbial flora;
- abacterial - with aseptic or toxic-chemical inflammation of the peritoneum due to its irritation by aggressive non-infected fluids (blood, digestive enzymes and secretions of internal organs, urine);
- special forms - parasitic, rheumatoid, carcinomatous and granulomatous.
According to the course of the disease, peritonitis is divided into acute and chronic.
According to the area of the affected peritoneum, inflammation can be limited, local (with damage to 1-2 anatomical areas), diffuse (covering three or more areas) and general (with total inflammation).
In its development, the disease goes through an early phase (less than twelve hours), late (less than five days) and final (from one to three weeks from the onset of inflammation).
Symptoms of upper gastrointestinal bleeding
Such bleeding can be identified by specific symptoms. The patient is concerned about:
- Vomiting and tarry stools;
- Fusion vomiting - vomiting with blood (hematemesis) with an admixture of hematin, formed by the action of hydrochloric acid on hemoglobin;
- Vomiting “coffee grounds.” It is black or brown in color due to the presence of hematin. With light bleeding, “coffee grounds” may not appear, and then the only sign is tarry stool.
During intense bleeding from the upper gastrointestinal tract, vomiting blood may be accompanied by loose, bloody stools. Information about the appearance of stool can be obtained from anamnesis or rectal examination. It should be borne in mind that there are medications that can cause stools to turn black, for example, iron or bismuth salts.
Is conservative treatment possible?
Depending on the shape and severity of the ovarian cyst rupture, treatment can be conservative or surgical. Conservative treatment is recommended only for mild disease severity. In such cases, the cyst is slightly damaged, and intense bleeding is prevented by a quickly formed blood clot. Therapy consists of taking antispasmodics, anti-inflammatory, analgesic and hemostatic agents. During the treatment period, the woman is recommended to undergo strict bed rest. The duration of the course is until the complaints disappear. To prevent the negative consequences that pathology may entail, the course is supplemented with physiotherapeutic treatment.
Determining the cause and assessing the intensity of bleeding
Often the probable cause of bleeding can be determined by history.
Important things to consider:
- symptoms of dyspepsia (especially at night);
- symptoms of stomach ulcer;
- side effects of medications taken, especially those that inhibit blood clotting, such as non-steroidal anti-inflammatory drugs;
- likelihood of alcohol abuse;
- the presence of hepatitis B or C - these may indicate liver cirrhosis and portal hypertension as possible causes of bleeding.
Physical examination
Physical examination
The gastroenterologist begins the examination from the head - carefully examining the nose, mouth and throat, since sometimes the cause of bleeding can be localized.
Next, they are identified with
symptoms of anemia and hypovolemia. The patient's heart rate and blood pressure are determined. A bad symptom is an acceleration of heart rate and a drop in blood pressure (>10 mmHg). Orthostatic hypotension involves rapid or severe blood loss.
Other signs that may indicate significant blood loss include:
- cool skin;
- oliguria;
- disturbances of consciousness.
Patients with anemia feel weak, dizzy, see spots before their eyes, have chest pain, and may faint. The severity of these symptoms depends on the amount of blood lost and the rate of bleeding.
It is also important to carefully examine the patient's body for symptoms of chronic liver disease. A number of specific symptoms indicate a pathological condition of the liver:
- presence of spider veins on the skin of the breast
- gynecomastia;
- loss of axillary and pubic hair;
- yellowing of the skin;
- palmar erythema;
- enlarged spleen;
- ascites;
- swelling of the legs;
- hand tremors
Signs of internal bleeding
If you determine what signs of internal bleeding a person has, you can determine the severity of a particular case. With minor pathology, weakness and drowsiness appear, the skin and mucous membranes turn pale, the person breaks into a sweat and is tormented by thirst. At the same time, the heart rate increases and the pressure becomes lower.
Weakness and dizziness are common signs of internal dizziness.
But with a mild form, there may be no signs of internal bleeding. Therefore, after blows and severe bruises, falls and fractures, you should always undergo additional tests to eliminate the risk of serious consequences.
If the internal bleeding is of moderate severity, the symptoms are as follows: the victim feels nauseous, his blood pressure drops significantly, and he may faint.
Signs of severe bleeding:
- Cold sweat and shortness of breath.
- Bluish pale skin.
- Tremor, darkening of the eyes.
- Heart rate - 110-160 beats per minute.
- Lack of vision, delirium, confusion of thoughts.
If a fatal form of internal bleeding occurs, the person falls into a coma, the pulse drops to 10 beats per minute, and convulsions begin.
I tell you what not to do when providing medical assistance in the article: The most common mistakes in providing first aid to a victim on a hike
Symptoms of neoplasms
Advanced neoplastic diseases are indicated by:
- underweight;
- enlarged, hard liver with a lumpy structure;
- palpable tumor in the abdominal cavity;
- enlarged and hard lymph nodes.
Other symptoms:
- Subcutaneous emphysema in a patient with persistent vomiting indicates Boerhaave syndrome (esophageal perforation). A prompt consultation with a surgeon is necessary.
- Telangiectasia on the mucous membranes may indicate Randu-Osler-Weber disease.
Complications
Peritonitis in children and adults is dangerous due to the development of multiple organ failure and intoxication of the body. Among the complications of the acute process:
- dehydration;
- renal failure;
- toxic shock;
- pulmonary pathologies;
- liver failure;
- secondary inflammatory processes.
Peritonitis after surgery may be accompanied by the formation of fistulas and abscesses of internal organs, and suppuration of postoperative sutures. The appearance of a number of complications is possible far beyond the abdominal cavity - occlusion of deep veins, inflammation of the lungs and pleura, mediastinitis.
Sigmoidoscopy (rectoscopy)
If necessary, an examination of the rectum is performed. Sigmoidoscopy (rectoscopy) is a method of endoscopic examination of the rectum and distal sigmoid colon by examining their internal surface using a sigmoidoscope inserted through the anus.
Sigmoidoscopy is the most accurate and reliable examination of the rectum and lower sigmoid colon. In the practice of a coloproctologist, sigmoidoscopy is an obligatory component of every proctological examination. The examination allows you to visually assess the internal surface of the rectum and distal third of the sigmoid colon to a level of 20-35 cm from the anus.
Bleeding from the lower digestive tract
Bleeding from the lower gastrointestinal tract accounts for approximately 20% of cases of gastrointestinal bleeding. The main symptom is chestnut or burgundy stool mixed with fresh blood (hematochezia).
The appearance of blood in the stool can indicate where the source of the bleeding is, namely:
- The presence of bright red blood in the stool indicates bleeding in the left side of the colon (up to the flexure of the spleen) or in the rectum;
- If there is bleeding in the right side of the colon, the blood is dark in color and may be mixed with the stool;
- Blood from the rectum may also be clear if it passes quickly from the right side of the colon or if there is a lot of bleeding from the upper gastrointestinal tract. In approximately 13% of patients with fresh blood in the stool, the source of bleeding is in the upper gastrointestinal tract;
- In the case of tarry stools, the most common source of bleeding is the upper gastrointestinal tract. The stool may be the same color if the source of bleeding is the cecum.
Determining the cause and assessing the intensity of bleeding from the lower gastrointestinal tract
Determining the cause and assessing the intensity of bleeding from the lower gastrointestinal tract
Sometimes bleeding from the upper gastrointestinal tract occurs without vomiting with bloody or soil-like contents, but with the removal of bloody contents through the anus.
It is important to consider the patient's age. For example, symptoms of bleeding from the lower gastrointestinal tract in a young person, with abdominal pain and diarrhea, may indicate inflammatory bowel disease. Similar symptoms in an elderly person indicate intestinal ischemia.
Streaks or spots of blood on the surface of the stool, pain in the anal area, and drops of blood on toilet paper or in the toilet indicate an anal fissure or bleeding from the rectum, such as hemorrhoids.
During the physical examination, the doctor pays special attention to symptoms indicating bleeding from the upper gastrointestinal tract and carefully examines the perineum and anal canal (rectally).
Hidden and unexplained gastrointestinal bleeding - classification, causes
In 2007, the American Gastroenterological Association proposed the following nomenclature for conditions associated with chronic gastrointestinal blood loss:
- Hidden bleeding
. This is the most common cause of iron deficiency. In men, it most often occurs in the gastrointestinal tract. In women, menstruation should be taken into account; - Vague bleeding
. It is recurrent or constant bleeding in the gastrointestinal tract, the cause of which cannot be determined despite endoscopic and radiological studies involving the entire gastrointestinal tract. This type of bleeding is divided into obvious and hidden.
The causes of hidden gastrointestinal bleeding are varied. The most common:
- colon cancer;
- esophagitis;
- inflammation or ulceration of the mucous membrane of the stomach or duodenum;
- intestinal inflammation;
- angiectasia;
- hypertensive portal gastropathy;
- diverticula;
- celiac disease.
Less common reasons include:
- esophageal carcinoma;
- stomach cancer;
- bleeding from the bile ducts or pancreatic ducts;
- aorto-intestinal fistulas;
- endometriosis;
- gastrointestinal infections.
Tests for latent blood in the stool may test positive for hemoptysis or nosebleeds.
It is not recommended to collect samples during digital rectal examination, as it may cause microtrauma and give a false-positive result.
Peroxidase test to confirm the presence of guaiacol
This is the most commonly used stool blood test. The test available is called Hemoccult. In this study, a stool sample is distributed into a guaiacol-impregnated cardboard box, which, if the stool contains heme, turns blue (heme causes a reaction similar to peroxidase). The more blood in the stool, the higher the likelihood of a positive result.
The Hemoccult test gives a positive result in 50% of cases when 10 ml of blood enters the gastrointestinal tract during the day. Under physiological conditions, 0.5-1.5 ml of blood is normally extravasated into the lumen of the gastrointestinal tract during the day.
The sensitivity of the first test is estimated to be approximately 30%. Performing 3 tests (which is the standard) increases the confidence to 92%. False negative results are especially common in people taking medications or foods high in vitamin C.
Relatively often, the test gives false positive results when consuming large amounts of red meat and foods high in peroxidase (radish, radish, horseradish). Taking iron supplements does not give false positive results in the study.
Immunochemical tests
Immunochemical tests
Immunochemical tests (HemeSelect, FECA, I-FOBT and Hemoccult ICT), used within European standards, detect undenatured human hemoglobin and give a positive result when it enters the gastrointestinal tract in an amount of 0.3 ml/24 hours.
These tests are not positive if the source of the bleeding is found in the upper gastrointestinal tract—hemoglobin from this source is denatured and degraded before it reaches the stool.
Determining the cause of bleeding - endoscopic and radiological methods
A history and physical examination are performed by a gastroenterologist in accordance with the principles of treatment when analyzing bleeding from the upper or lower gastrointestinal tract.
Further tests for a patient who tests positive for blood in the stool include:
- Peripheral blood analysis - looking for signs of anemia;
- Endoscopic examinations of the gastrointestinal tract - esophagogastroduodenoscopy and colonoscopy. These tests help identify the possible source of bleeding. Colonoscopy may be considered sufficient in the absence of anemia or gastrointestinal symptoms.
Enteroscopy offers great diagnostic and therapeutic options in case of suspicious changes in the small intestine.
When endoscopic examinations do not help determine the source of bleeding, X-ray examination
small intestine with evaluation of the fragment and possibly enteroclysis.
In difficult cases, CT or MRI enterography and endoscopic examination are performed using a special capsule with a built-in video camera, which the patient swallows like a regular pill.
Diagnostics
Laboratory diagnostics
1. Complete blood count - depending on the duration of the bleeding, the blood picture may vary. In the acute phase, a decrease in the level of red blood cells, hemoglobin and the liquid part of the blood (plasma) is observed; the hematocrit “Ht” during acute bleeding remains unchanged, since plasma and formed elements are lost equally. With chronic minor bleeding, a decrease in the level of red blood cells and hemoglobin is also found, “Ht” in this case is reduced, there is an increase in the level of reticulocytes (immature red blood cells) - this is a compensation reaction, replenishing the number of red blood cells. An advanced analysis with determination of platelet levels is necessary for diagnosing thrombocytopenia (possible with various diseases of internal organs, poor nutrition, genetic pathologies).
2. General urine test - necessary to assess the functional ability of the kidneys to secrete urine. With significant blood loss, diuresis may be reduced and even absent altogether (anuria in hemorrhagic shock).
3. Biochemical blood test - determination of the concentration of bilirubin, urea, creatinine, total protein, LDH (lactate dehydrogenase), cholesterol, blood glucose, etc. All these studies are necessary for a thorough differential diagnosis.
4. Determination of blood group and Rh factor - necessary for possible blood transfusion.
5. Coagulogram - analysis of the function of the cascade protein blood coagulation system (prothrombin index, prothrombin time, level of fibrinogen, antithrombin III, D-dimer, etc.).
Instrumental diagnostics
1. X-ray of the abdominal organs and chest cavity - allows you to determine the presence of fluid accumulation in the cavities, displacement of organs, defects of large vessels. Additionally, special contrast agents (for example, barium sulfate) can be used.
2. Ultrasound examination (ultrasound) - used for primary and differential diagnosis of bleeding with other pathologies (cysts, tumors).
3. Computed tomography (CT) - used when the primary diagnosis is questionable. The essence of the method is to obtain a layer-by-layer image of tissues and organs using x-rays.
4. Magnetic resonance imaging is a safe and informative diagnostic method. Used when other graphical research methods are ineffective. Allows you to identify the smallest and “hidden” hematomas.
5. Diagnostic laparoscopy is a method of visualizing the contents of the abdominal cavity by puncturing the abdominal wall with the introduction of a tube with a video camera.
6. Diagnostic laparatomy - an incision is made in the anterior abdominal wall from the xiphoid process to the symphysis pubis (to the extent necessary for diagnosis). The doctor examines the organs and makes a final diagnosis.
Pathologies that rarely cause bleeding
A positive stool blood test should not be associated with pathologies of the gastrointestinal tract, which rarely cause hidden bleeding, namely:
- varicose veins of the esophagus;
- diverticulosis of the large intestine.
In the vast majority of these cases, bleeding is obvious. An exception is the disease of varicose veins of the esophagus, after endoscopic therapy or sclerotherapy procedures. The discovery of such changes in a patient with a positive test result does not exempt him from performing gastrointestinal studies.
Diverticula in the colon produce symptoms in people of the same age similar to organ cancer, which often causes hidden bleeding.
Reasons for false test results
- Anticoagulant treatment. A positive test result for the presence of latent exudate in the stool cannot be taken into account in patients taking medications that suppress blood clotting (acetylsalicylic acid, clopidogrel, acenocoumarol, warfarin, heparins). Also, taking such drugs does not eliminate the need to look for the cause of blood in the stool. Taking acetylsalicylic acid at a dose of 300 mg/24 hours. slightly increases the amount of blood passing into the stool. Neither aspirin nor warfarin interferes with fecal tests;
- Alcohol abuse. Hidden blood in the stool has nothing to do with alcohol consumption. But alcohol abuse increases the risk of developing peptic ulcers and gastrointestinal cancer;
- Menstruation. The most common cause of iron deficiency and anemia in premenopausal women is menstruation. However, when abdominal symptoms coexist, women over 40 years of age may be diagnosed with gastrointestinal cancer. A positive stool blood test requires diagnosis of sources of bleeding.
Pulmonary hemorrhage in a child: how it manifests itself and how to stop it
Pulmonary hemorrhage is the production of blood-stained sputum (hemophthisis) or pure blood (hemoptoea) when coughing. The most acceptable and practically justified classification of conditions associated with the release of blood from the respiratory tract in pediatric practice is the following:
- Hemoptysis - up to 150 ml/day;
- Pulmonary bleeding - 150-400 ml/day;
- Massive pulmonary bleeding - more than 400 ml/day.
However, in both hemoptysis and pulmonary hemorrhage, any amount of blood released can lead to serious respiratory compromise and life-threatening hemodynamic instability.
Pulmonary hemorrhage can develop with infectious diseases (tuberculosis, measles, whooping cough, influenza), bronchitis, bronchiectasis, destructive pneumonia, pulmonary hemosiderosis, angiomatosis, chest trauma, foreign bodies entering the respiratory tract, tumors, primary pulmonary hypertension (Ayers syndrome), diseases of the cardiovascular system (mitral stenosis), ascariasis, taking certain medications, pulmonary infarction, etc.
The clinical picture depends on the severity of the bleeding. If there is blood in the sputum (hemoptysis), the symptoms of the underlying disease (tuberculosis, ARVI, etc.) come to the fore. Heavy bleeding usually begins suddenly or after hemoptysis. Pallor of the skin is noted, blood pressure decreases until collapse. When you cough, bright red frothy blood is released. On auscultation, fine bubbling rales are heard in the lungs.
Treatment. There are three main stages in the treatment of a patient with hemoptysis and pulmonary hemorrhage:
- Cardiopulmonary resuscitation, stabilization of hemodynamics and hemostasis, protection of the respiratory tract are the highest priority;
- Localizing the source and identifying the cause is the second stage;
- In conclusion, specific measures are taken to stop and prevent re-bleeding.
Infusion therapy: the use of blood components and coagulation factors is carried out according to the general rules for the correction of hemodynamics and hemostasis during blood loss. Apply a 12.5% solution of ethamsylate (dicinone) at a dose of 5 mg/kg 2-3 times a day intramuscularly or intravenously; 1% solution of Vikasol: children under 1 year of age - 0.2-0.5 ml, from 1 to 3 years - 0.6 ml, 4-5 years - 0.8 ml, 6-9 years - 1 ml, 10 years and older - 1.5 ml 2-3 times a day intramuscularly - 5% ascorbic acid solution at a dose of 0.5-2 ml intravenously; rutin - orally: up to 1 year of age - 0.0075 g/day, up to 4 years - 0.02 g/day, over 5 years - 0.03 g/day. For heavy bleeding, intravenous administration of a 5% solution of aminocaproic acid at a dose of 1 ml/kg body weight every 6 hours is effective.
Transfusion of plasma replacement solutions (polyglucin, infucol HES, etc.), 10% calcium gluconate solution at a dose of 1 ml/year of life, but not more than 10 ml, and blood products is indicated. A 2.4% aminophylline solution is used: for children under 1 year old - 0.4 ml, 1-5 years old - 0.5-2 ml, 6-10 years old - 2-3 ml, over 10 years old - 5 ml. If the therapy is ineffective, diagnostic and therapeutic bronchoscopy is necessary.
If the cause of bleeding is established, surgical treatment is sometimes indicated, which remains one of the main methods of choice for pulmonary hemorrhage, if the source of bleeding is established, especially in the case of localized bronchiectasis, trauma, parasitic cyst, aspergiloma, arteriovenous malformation, aneurysm.
Treatment of hemoptysis and pulmonary hemorrhage should be carried out against the background of treatment of the underlying disease. In some cases, specific treatment of the underlying disease is decisive in the treatment of bleeding. For example, in Goodpasture's disease there is no need to perform invasive procedures - high doses of glucocorticoids, cytostatic agents and plasmapheresis should be used.
Diagnosis of gastrointestinal bleeding - tests
Diagnosis of gastrointestinal bleeding - tests
First of all, the gastroenterologist needs to detect the source of bleeding. It must be looked for using: endoscopic, x-ray and scintigraphic studies.
- Morphology of peripheral blood.
The analysis is necessary to assess blood loss. Comparing the current result with previous ones helps with this. On the first day of bleeding, analysis should be done every 4-6 hours. In the first few hours of acute bleeding, hemoglobin levels and hematocrit may not change significantly (due to compensatory mechanisms). In addition to the loss of red blood cells, elevated white blood cell and platelet counts are common in this diagnosis, and from days 3 to 7, the reticulocyte count begins to increase (however, this does not occur in people with significant iron deficiency); - Urea concentration and assessment of renal function.
Blood urea levels may rise slightly if there is heavy bleeding from the upper gastrointestinal tract because the protein-containing blood becomes a source of ammonia and urea. In this regard, the patient may have concurrent chronic kidney disease, which increases the risk of death. Acute prerenal kidney injury may be a symptom of hemorrhagic shock; - Liver markers
. Serum transaminase and bilirubin activities help assess the coexistence of liver disease; - Markers of thyroid diseases
. Measuring serum calcium levels can identify hyperparathyroidism, which contributes to the development of gastric and duodenal ulcers; - Assessment of blood clotting.
Tests that evaluate the efficiency of the blood coagulation system - prothrombin time (PT) and activated partial thromboplastin time (aPTT) are important.
The problem occurs in patients taking warfarin or acenocoumarol. It should be assessed whether continuation of treatment, which makes it difficult to control bleeding, or discontinuation of treatment due to the risk of thromboembolic complications, would be more life-threatening. In such a situation, oral drugs are replaced with short-acting low-molecular-weight heparin drugs.
If generalized intravascular coagulation syndrome is suspected, the concentration of D-dimer, fibrinogen and platelet count should be determined.
When a blood transfusion is necessary, the blood type should be determined and cross-matched.
How do blood vessels bleed?
Bleeding can be mild, moderate or severe. His character may be:
- arterial - strong, jet;
- venous - blood loss occurs gradually;
- capillary - minor discharge due to damage to small vessels.
The problem itself can be stable/unstable, recurrent. Vessels of the mucosa, submucosal and intermuscular plexus, as well as those located outside the gastrointestinal tract, can bleed.
The expiration can last for several hours or days. In medicine there are:
- profuse blood loss - the patient loses more than 1 liter of blood in 1-3 hours and needs urgent medical attention;
- acute - less than 1 liter expires in 1-2 days, the patient’s vital signs are relatively stable;
- chronic - develops slowly, often over several weeks or even months, the intensity of symptoms gradually increases.
Other studies for gastrointestinal bleeding
- ECG
. Allows you to diagnose myocardial arrhythmia and ischemia, which may appear or worsen during intense bleeding. If acute coronary syndrome is suspected, blood troponin levels should be measured. - Check weighing
. Weight loss results from a reduced-calorie diet, increased energy expenditure, or energy loss in urine or stool. A loss of >5% body weight over 6–12 months is clinically significant. Losing weight can be either deliberate or unintentional. Unintentional weight loss is the most common symptom (regardless of increased appetite) of a serious illness and requires diagnosis. Intentional weight loss in an overweight patient who is dieting and exercising is not a cause for concern, but can sometimes be a symptom of mental illness.
The mechanisms leading to weight loss are very different:
- In diseases of the gastrointestinal tract, the cause is the inability to eat the required amount of food (dyspepsia, dysphagia) or its insufficient digestion and absorption.
- In neoplastic or chronic inflammatory diseases, anorexia is promoted by increased production of cytokines such as tumor necrosis factor (TNF-α), interleukins 1 and 6, and C-reactive protein (CRP).
Because there are many causes of weight loss, there are no universal diagnostic procedures, so the diagnostic process should be individualized based on the results of a thorough history and physical examination.
Most patients should:
- peripheral blood analysis with leukogram;
- measurement of serum levels: electrolytes (including calcium), glucose, parameters assessing renal function, albumin, thyroid-stimulating hormone (TSH);
- measurement of acute phase parameters (ESR, CRP);
- serological tests for HIV infection;
- chest x-ray.
Further management of the patient depends on the results of these preliminary studies.
If you find an error, please select a piece of text and press Ctrl+Enter
Can the body cope with bleeding?
Nature has provided for the possibility that fragile and delicate living tissues of the body will be injured over a long life. This means that a mechanism is needed to resist the flow of blood from damaged vessels. And people have it. Blood plasma, that is, the liquid part that does not contain cells, contains biologically active substances - special proteins. Together they make up the blood coagulation system. It is assisted by special blood cells called platelets. The result of complex multi-stage blood clotting processes is the formation of a thrombus - a small clot that clogs the affected vessel.
In laboratory practice, there are special indicators that show the state of the blood coagulation system:
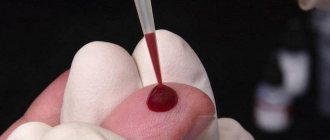
- Duration of bleeding. An indicator of the duration of blood effusion from a small standard injury caused by a special stylet on a finger or earlobe.
- Blood clotting time - shows how long it takes the blood to clot and form a clot. Conducted in test tubes.
Often, trauma or damage to a vessel by a pathological process is too extensive and natural mechanisms to stop bleeding cannot cope, or a person simply does not have time to wait due to the threat to life. Without being a specialist, it is difficult to assess the condition of the victim, and treatment tactics will vary depending on the cause.
Therefore, a patient who has severe bleeding from a vein or artery must be urgently transported to a medical facility. Before this, he must be provided with emergency assistance. To do this, you need to stop the bleeding. Usually this is a temporary cessation of blood flow from the vessel.