Arterial hypertension (AH, arterial hypertension) is a pathological condition that leads to increased blood pressure, as a result of which the structure and function of the arteries and heart are disrupted.
Medical statistics claim that 30-40% of the world's inhabitants suffer from hypertension. Among people over 65 years of age, the disease is registered in 70%.
1
ABPM in the diagnosis of hypertension
2 Diagnosis of hypertension at MedicCity
3 Diagnosis of arterial hypertension
Hypertension significantly affects the quality of life: it causes attacks of headaches and dizziness, and affects performance. With long-term hypertension, irreversible changes occur in human organs and systems that threaten not only health, but also life itself.
Target organs for arterial hypertension:
- heart (left ventricular hypertrophy, heart failure, angina, myocardial infarction, etc.);
- brain (hypertensive encephalopathy, ischemic or hemorrhagic stroke, dementia);
- blood vessels (reduced arterial patency, aortic aneurysm);
- eyes (hemorrhages, retinal lesions, blindness);
- kidneys (renal failure).
1 ABPM for hypertension
2 ABPM for hypertension
3 ECHO-CG for hypertension
Blood pressure indicators for hypertension
The main manifestation of hypertension is a long-term and persistent increase in blood pressure (BP).
There are systolic (or upper) blood pressure, which shows the level of blood pressure at the moment the heart contracts, and diastolic (lower), which shows the level of blood pressure at the moment the heart relaxes.
Normal blood pressure levels are considered to be 120-134/80-84 mmHg, but data may vary due to emotional shocks, physical activity, changes in air temperature, etc. These fluctuations are normal; they reflect the body’s naturally programmed reaction to changes in living conditions. However, constantly elevated blood pressure in the absence of obvious reasons for this is a significant reason to take care of your health.
Arterial hypertension is indicated by a stable increase in blood pressure (systolic - above 140 mm Hg, diastolic - above 90 mm Hg when measured at a doctor’s appointment; 135/85 mm Hg and above - when measured independently) , confirmed by repeated measurements. To establish a diagnosis of arterial hypertension, two measurements with elevated blood pressure in the absence of physical and emotional stress are sufficient.
Diastolic hypertension does not lead to an increased risk of adverse events
In 2021, the American Heart Association and the American College of Cardiology lowered blood pressure (BP) targets to 130/80 mmHg. Art. for all patients, as reflected in the relevant guidelines (ACC/AHA 2017). These same indicators became the threshold for first-degree hypertension.
Some other medical societies disagreed with the new criteria. The authors of the new study were no exception.
They analyzed data from 9,590 participants in the US National Health and Nutrition Examination Survey (NHANES) from 2013 to 2016. In calculations using the ACC/AHA 2017 classification, the prevalence of isolated diastolic hypertension was found to be 6.5%. When using the previous standard as a threshold value, 90 mm Hg. Art., this figure was 1.3%.
If these figures are applied to the entire US population, the difference would be approximately 12 million people, the researchers note.
Long-term outcomes of isolated diastolic hypertension for both measures were examined in another study that included 8,703 participants. Over a 25-year period, such hypertension had virtually no increased risk of atherosclerotic cardiovascular disease, heart failure, or chronic kidney disease compared with normal blood pressure.
“According to our data, from a diastolic pressure of 80 mm Hg. Art. there is no harm if the systolic does not exceed 130 mm Hg. Art.,” one of the authors of the publication, John William McEvoy, a professor at the National University of Ireland in Galway, told MedScape. He believes that the reduction in the normative value of diastolic pressure was based on expert opinion; there is no evidence to support this recommendation.
ACC/AHA 2021 Guidelines Committee Chair Dr. Whelton agreed that systolic blood pressure is a more important indicator for assessing cardiovascular risk and making pharmacotherapy decisions. Studies indicate a significant benefit of treatment with antihypertensive drugs for diastolic pressure above 90 mmHg. Art.
“Trials have not really been conducted in people with isolated diastolic hypertension, and there are no recommendations for treatment of such patients in the 2021 ACC/AHA guidelines. Therefore, the new study, while interesting, is not directly relevant to the 2021 ACC/AHA guidelines,” Dr. Welton said. He also notes that the guidelines include instructions that patients with blood pressure greater than 130/80 mmHg. Art. and those without CVD or high risk for these diseases should not receive pharmacotherapy.
McAvoy disagrees with Welton. He said the study should start a larger discussion and prompt a review of the guidelines. “These guidelines clearly define the threshold for hypertension as 80 mm Hg. Art. for diastolic pressure, and this could be interpreted as a signal to diagnose and treat isolated hypertension in some unneeded patients,” says McEvoy.
Degrees of arterial hypertension
In modern cardiology, several classifications of arterial hypertension are used.
Classification by origin
Arterial hypertension can be an independent disease (hypertension). Or act as a sign of diseases of other organs, systems - endocrine glands (thyroid, adrenal glands), kidneys, heart, blood vessels. And also be the result of taking certain medications. In this case, we will talk about symptomatic (or secondary arterial hypertension).
The classification of hypertension according to blood pressure level, adopted by WHO, distinguishes three degrees of arterial hypertension:
1st degree (soft) - 140-159/90-99; 2nd degree (average) - 160-179/100-109; 3rd degree (severe) - 180/110 and above;
Isolated systolic hypertension is distinguished separately - SBP is above 180, DBP is below 90.
According to the degree of target organ damage, three stages of arterial hypertension are distinguished:
- at the first stage of arterial hypertension, an increase in blood pressure is not accompanied by changes in target organs;
- at the second stage, there is a persistent increase in blood pressure and organic changes in internal organs (however, without significant impairment of their functions). At this stage of the development of hypertension, signs of atherosclerotic damage to large vessels, narrowing of the retinal arteries, hypertrophy of the left ventricle of the heart may be detected; there is an increase in the level of creatinine in the blood and protein in the urine;
- at the third stage of arterial hypertension, a significant increase in blood pressure is associated with pathological changes in target organs and severe impairment of their functions (myocardial infarction, acute cerebrovascular accident, retinal hemorrhages, etc.).
1 Ultrasound of the heart for hypertension
2 ECG for hypertension
3 Diagnosis of hypertension at MedicCity
Modern principles of control of mild arterial hypertension
To radically reduce the incidence of complications associated with hypertension (CHD, strokes), it is not enough to pay attention only to patients with moderate and severe forms of hypertension; it is necessary to actively identify and treat people with mild arterial hypertension
Arterial hypertension (AH), the prevalence of which among the adult population is 20%, remains a serious health problem in most countries, including Russia. Hypertension is one of the main risk factors for the development of cardiovascular diseases and mortality from them, the share of which in the structure of overall mortality reaches 50%. To successfully control hypertension and its complications, it is necessary to promptly identify and treat patients with this pathology. This problem is of particular relevance for Russia. According to the latest data from the WHO working group (1997), in recent years in Russia there has been a catastrophic increase in mortality from ischemic heart disease and cerebral strokes, which are the main complication of hypertension. According to these indicators, Russia ranks among the first in Europe.
The problem of controlling hypertension and its complications is complicated by the fact that most patients with this pathology do not complain and do not actively consult a doctor. Increased blood pressure (BP) in this population is found by chance during routine examinations of the population. This category of people is classified as a group of patients with mild arterial hypertension (MAH). The majority of complications associated with hypertension (approximately 60%) occur specifically in the group of people with MAH. Therefore, it is obvious that to radically reduce the incidence of complications of hypertension, it is not enough to pay attention only to patients with moderate and severe forms of hypertension. Individuals with MAH must be actively identified and treated.
- What are the criteria for MAG?
According to the modern classification of hypertension, recommended by WHO and the International Society for the Study of Hypertension in 1993 [1], mild hypertension is diagnosed in cases where diastolic blood pressure is constantly in the range of 90-105 mm Hg. Art. and/or systolic blood pressure - within 140-180 mm Hg. Art. (Table 1).
Table 1. Classification of arterial hypertension by blood pressure level
| Systolic (SBP) and diastolic (DBP) pressure in mmHg. Art. (kPa) | |
| Normal pressure | SBP 140 (18.7) and DBP 90 (12.0) |
| Mild hypertension | SBP 140 - 180 (18.7-24.0) and/or DBP 90 - 105 (12.0-14.0) |
| Borderline hypertension | SBP 140 - 160 (18.7-21.3) and/or DBP 90 - 95 (12.0-12.7) |
| Moderate to severe hypertension | SBP 180 (24.0) and/or DBP 105 (14.0) |
| Isolated systolic hypertension | SBP 140 (18.7) and DBP 90 (12.0) |
| Borderline isolated hypertension | SBP 140 - 160 (18.7-21.3) and DBP 90 (12.0) |
It should be noted that not all countries adhere to these criteria. For example, in the USA, the Joint National Committee on the Detection, Assessment of Severity and Treatment of Hypertension recommended the following MAH criteria: diastolic blood pressure within 90-99 mm Hg. Art. and/or systolic blood pressure in the range of 140-179 mm Hg. Art. [2]. In a number of countries, when studying the effectiveness of antihypertensive drugs in people with MAH, they also used their own criteria for diagnosing this form of hypertension. However, when identifying and treating hypertension, it is still more correct to use the criteria of the WHO and the International Society for the Study of Hypertension.
- What principles should a doctor follow when treating patients with MAG?
First of all, you need to remember the main thing: treatment and preventive measures for people with MAH are a long process aimed not only at reducing blood pressure levels, but mainly at preventing complications. Therefore, the doctor must monitor not only hypertension, but also other risk factors and concomitant diseases that can cause complications. In table Table 2 presents factors that must be taken into account when assessing the overall cardiovascular risk in patients with MAH. All patients with MAH should first of all be given recommendations for the correction of modifiable risk factors.
Table 2. Risk factors for cardiovascular disease
|
To give up smoking. You should strongly recommend quitting smoking in every conversation with the patient. It must be emphasized that people who continue to smoke remain at increased risk of developing coronary artery disease even after their blood pressure has returned to normal.
Weight loss. Of particular importance is excess fat deposition in the abdominal area, which strongly correlates with lipid metabolism disorders and non-insulin-dependent diabetes mellitus. Weight loss not only leads to a decrease in blood pressure, but also has a beneficial effect on the lipid profile and tissue resistance to insulin. American experts recommend a low-calorie diet low in fat and cholesterol (1200 kcal). Based on a cumulative analysis of many studies, it was found that losing 5 extra pounds leads to a decrease in systolic blood pressure by 5.4 mmHg. Art., and diastolic blood pressure - by 2.4 mm Hg. Art.
Increase physical activity. An analysis of many studies shows that regular physical training reduces systolic and diastolic blood pressure by an average of 5-10 mm Hg. Art. Dynamic isotonic exercises, such as walking, are more effective than static exercises such as barbell exercises. Mild exercise, such as brisk walking for 30-60 minutes three to five times a week, is more physiological than intense exercise (running). Physical activity also helps to lose excess weight and improve the functional state of the body. Epidemiological studies indicate that in the group of physically active individuals, not only mortality from cardiovascular diseases, but also overall mortality decreases. Thus, regular physical activity should become an integral part of the prevention of complications in people with MAH.
| Treatment and preventive measures for patients with mild arterial hypertension is a long-term process aimed not only at reducing blood pressure levels, but mainly at preventing complications. Therefore, it is necessary to control both hypertension and other risk factors and concomitant diseases |
Non-drug correction of these risk factors, along with limiting salt intake (no more than 6 g per day) and reducing alcohol consumption should become an axiom for all patients with MAH, regardless of whether they are prescribed antihypertensive drugs or not. Moreover, drug prevention of complications of hypertension can only be successful when it is carried out in combination with non-drug prevention [3, 4]. It has also been shown that non-pharmacological methods - weight loss, increasing potassium intake and limiting sodium intake - can control blood pressure at lower doses of antihypertensive drugs [5, 6]. At the same time, the side effects of the drug were less pronounced, and the quality of life of patients improved when drug treatment was combined with non-drug treatment [7]. In addition, during long-term treatment of persons with MAH, the physician must take into account concomitant diseases that significantly increase the risk of complications, such as diabetes mellitus and renal disease.
Thus, the main question when determining the management tactics for people with MAH is the question of who to prescribe medications to. To answer this, it is necessary to refer to the recommendations of the WHO and the International Society for the Study of Hypertension [8]. If the initial level of systolic blood pressure is in the range of 140-180 mm Hg. Art. and/or diastolic blood pressure - within 90-105 mm Hg. Art., then before a diagnosis of MAH is made and a plan of treatment and preventive measures is determined, it is necessary to re-measure blood pressure at least twice within four weeks (Fig. 1).
| Picture 1 |
This is very important because both systolic and diastolic blood pressure are subject to natural fluctuations. If the patient's systolic blood pressure falls below 140 mmHg over the next four weeks. Art. and/or diastolic blood pressure - below 90 mm Hg. Art., then it is necessary to monitor blood pressure every three months throughout the year. If in the next four weeks systolic and/or diastolic blood pressure remains at the same level, and the overall risk of developing cardiovascular diseases is high, then drug treatment should be started. A high overall risk is determined primarily by the presence of target organ damage: left ventricular hypertrophy, changes in the arteries of the fundus, impaired renal function (plasma creatinine level 1.2-2.0 mg/dl, the presence of protein in the urine). In addition, a high risk is determined by previous history of ischemic heart disease, cerebral stroke, and hereditary history of hypertension. If these diseases and circumstances undoubtedly determine the prescription of antihypertensive drugs, then for factors such as total cholesterol levels, age, smoking, there are quantitative criteria recommended by three European societies (cardiology, the study of atherosclerosis and the study of hypertension) [9]. The authors recommend prescribing antihypertensive drugs to patients whose absolute risk of developing coronary artery disease within 10 years exceeds 20% (Fig. 2). For example, at the age of 40 years, this degree of risk is observed in smokers with a systolic blood pressure level of 180 mm Hg. Art. and a total cholesterol content in the blood plasma of 300 mg/dl, and at the age of 50 years, non-smokers have the same level of cholesterol with a systolic blood pressure of 160 mm Hg. Art. If the risk is low (less than 20%) and there is no organ damage, it is recommended to carry out non-drug treatment and monitor blood pressure over the next three to six months. If after six months the level of systolic blood pressure remains within 140-160 mm Hg. Art. and/or diastolic blood pressure level - within 90-95 mm Hg. Art., then non-pharmacological intervention and blood pressure monitoring should be continued. However, if during the specified period the systolic blood pressure remains at 160 mm Hg. Art. and higher, and diastolic blood pressure - at the level of 95 mm Hg. Art. and above, you need to start
| Success in the prevention of complications of hypertension is determined by combined drug and non-drug treatment of patients with mild arterial hypertension, as well as adequate cooperation between the patient and the doctor |
drug treatment. Thus, the main points that determine the management tactics of people with MAH are: confirmation of the stability of the increase in blood pressure, assessment of the overall cardiovascular risk and decision on the issue of drug treatment.
- What drugs should a doctor give preference if he decides to treat a patient with MAG with medication?
Before answering this question, it is necessary to take into account the experience of long-term studies examining the effectiveness of medications in preventing complications of hypertension. A summary analysis of 17 such studies conducted in different countries around the world in the 1980s suggests that the effectiveness of drug treatment (short-acting beta blockers and diuretics were used in these studies) was evident only in relation to strokes - their incidence decreased by 36% . However, mortality from IHD decreased by only 14% [10]. Since ischemic heart disease is the main complication of hypertension, the overall effectiveness of drug treatment has been considered insufficient. The explanation for this phenomenon comes down to three main reasons. Firstly, the short-acting beta blockers and diuretics used in these studies did not provide a stable reduction in blood pressure throughout the day and especially in the morning and pre-dawn hours, when myocardial infarction, stroke and sudden death most often develop in people with hypertension. Secondly, these drugs, when used for a long time, caused a number of metabolic changes - impaired lipid metabolism, decreased glucose tolerance, decreased tissue sensitivity to insulin, which could neutralize the effect of lowering blood pressure. And finally, drug prevention was not accompanied by non-drug correction of risk factors, the importance of which was discussed above. Thus, at present, preference in long-term treatment of MAG should be given to those drugs or their dosage forms that provide a stable decrease in blood pressure throughout the day and do not cause metabolic disorders. These drugs include, first of all, long-acting forms of calcium antagonists and ACE inhibitors. As a result of our study, the majority of patients with MAH were able to adequately control blood pressure levels using the calcium antagonist isradipine (trade name “Lomir”) and the ACE inhibitor volsartan (trade name “Diovan”). Both drugs are produced by Novartis Pharma (Switzerland). Moreover, these drugs, like most drugs of the calcium antagonist group, do not cause negative metabolic effects. Other long-acting calcium antagonists that deserve attention are isoptin retard form - 240 mg (Knoll, Germany), altiazem (diltiazem retard form, Berlin-Chemie, Germany), amlodipine (trade name “Norvasc”, Pfiser, USA). Among the ACE inhibitors, the drug ramipril (trade name Tritace, Hoehst, Germany) should be noted. This drug not only steadily reduces blood pressure throughout the day, but also causes a reverse development of myocardial hypertrophy even in the smallest doses (1.25 mg), which are insufficient to reduce blood pressure. Also worthy of attention is a new drug from the group of centrally acting sympatholytic drugs - moxonidine (trade name “cynt” - Elli Lilly, USA), which is an agonist of imidazoline receptors located in the ventrolateral part of the rostral brain stem. According to our research, as well as foreign colleagues, this drug not only causes a stable decrease in blood pressure throughout the day, but also increases tissue sensitivity to insulin.
The antihypertensive drugs listed above cover two of the five classes currently used to treat hypertension. To finally resolve the question of how effective they are than other classes of antihypertensive drugs, long-term studies are needed in terms of the effectiveness of reducing complications of hypertension. So far, such studies have only been conducted with beta blockers and diuretics, as discussed above. Moreover, in certain situations when, for example, hypertension is combined with coronary artery disease, arrhythmia, or heart failure, it is impossible to refuse the use of diuretics and beta blockers, since these drugs improve survival in this category of patients with hypertension. In general, when choosing an initial drug for the treatment of hypertension, it is necessary to be guided by both the presence of metabolic disorders and concomitant diseases and complications (Table 3). If, in the treatment of hypertension in a particular patient, any of the five main groups is ineffective, it should be replaced with another drug. If monotherapy is not effective enough, it is better to add small doses of another drug than to increase the dose of the original one. Given the different mechanisms of action of antihypertensive drugs, the chance of suppressing pathophysiological factors that prevent blood pressure from lowering increases. In addition, combination therapy can also reduce side effects due to the use of small doses of drugs.
Table 3. Recommendations for choosing the initial drug for the treatment of arterial hypertension
| Drug class | Indications | Contraindications | Limited |
| Diuretics | Heart failure. Old age of the patient. Systolic hypertension | Gout | Diabetes. Pregnancy*. Increased sexual activity in men |
| Beta blockers | Angina pectoris. Previous myocardial infarction. Tachyarrhythmia. Pregnancy | Bronchial asthma and chronic obstructive pulmonary diseases. Peripheral vascular diseases. Heart blocks** | Hyperglyceridemia. Insulin-dependent diabetes mellitus. Heart failure. Athletically challenging and physically active individuals |
| ACE inhibitors | Heart failure. Left ventricular hypertrophy. Previous myocardial infarction. Diabetes with microalbuminuria | Pregnancy. Bilateral renal artery stenosis | |
| Calcium antagonists | Angina pectoris. Peripheral arterial diseases. Old age of the patient. Systolic hypertension. Low glucose tolerance | Pregnancy | Congestive circulatory failure*** Heart block**** |
| Alpha blockers | Prostate hypertrophy. Low glucose tolerance | Orthostatic hypotension | |
| * – due to a decrease in plasma volume ** – atrioventricular blocks of the second and third degrees *** – either avoid or prescribe with caution **** – either avoid or prescribe verapamil and diltiazem with caution | |||
An integral part of measures for long-term prevention of complications of hypertension should be educational programs for both doctors and patients. After all, if we assume that for each specific patient with MAH the doctor will develop an ideal program of drug and non-drug treatment, it will be very difficult to implement this due to the low motivation of patients for treatment. As a result, for example, in Central Europe, only 22% of patients with hypertension can adequately control blood pressure, and in Russia - only 12%. The most striking example of the effectiveness of educational programs is the program to control hypertension and its complications, conducted in the United States since the 70s. As a result of active educational work, which was part of the project to control hypertension, the awareness of patients about this disease increased significantly, the coverage of their treatment expanded, and the number of adequately treated individuals increased. This led to the fact that over the 20-year period of the program, mortality from cardiovascular diseases was halved. Well-known American scientists in many publications emphasize the role of the educational program in this achievement.
| When choosing an antihypertensive drug for the treatment of mild arterial hypertension, it is necessary to take into account concomitant complications and diseases, as well as metabolic disorders |
The doctor should inform the patient with MAH about the risk of complications, factors and diseases associated with hypertension, and also talk about methods of drug and non-drug treatment of this disease. Each stage of treatment and prevention must be agreed upon with the patient. It is necessary to find out which medications and methods of non-drug prevention the patient prefers. Such measures should ensure the conscious participation of the patient in the treatment and prophylactic process and increase its effectiveness. In conclusion, it must be emphasized that success in preventing complications of hypertension will be determined by active identification and combined drug and non-drug treatment of people with MAH, subject to adequate cooperation between the doctor and the patient. This will require significant efforts on both sides, without which a fundamental change in reducing the complications of hypertension can hardly be achieved.
References
1. Subcommittee of WHO? (ISH Mild Hypertension Liasion Committee. Summary of the World Health Organization-International Society of Hypertension guidelines for the management of mild hypertension // Br. Med. J. 1993; 307: 1541-6. 2. Joint National Committee on Detection, Evaluation and Treatment of High Blood Pressure (JNC V) // Arch. Intern. Med. 1993; 153: 154-83. 3. Britov A., Elisseeva N., Beloussov S., Golub AG Outpatient experience in Treatment of Pts with Mildness Hypertension in Occupational Groups: From Drug Trial to Practice. New York, 1987; 213-18. 4. Kalinina A. M. The influence of long-term multifactorial prevention of coronary heart disease on some health indicators and life prognosis: Abstract of thesis... Dr. med. . nauk. M.: 1993( 45. 5. Chalmers GP The place of combination therapy in the treatment of hypertension in 1993 // Clin. Exper Hypertens 1993; 15(6): 1299-313. 6. Siani A. et al Increasing the dietary potassium intake reduces the need for antihypertensive medication // Ann. Intern. Med., 1991; 115: 753-9. 7. Neaton JD, et al. Treatment of Mild Hypertension Study. Final Results // J. Am. Med. Ass. 1993; 270(6): 713-24. 8. Fight against arterial hypertension. Dokl. WHO Expert Committee // Trans. from English Joint ed. GNITSPM MZ RF and RKNK MZ RF. Moscow, 1997, p. 93-96. 9. The Task Force of the European Society of Cardiology, European Atherosclerosis Society and European Society of Hypertension // Eur. Heart. J. 1994; 15: 1300-1331. 10. MacMahon S., Rodgers A. The effects of antihypertensive treatment on vascular disease: reapprisal of the evidence in 1994 // J. Vasc. Med. Biol., 1993; 4: 265-71.
Signs of arterial hypertension
Often, hypertension has no symptoms at all other than persistent high blood pressure. At the same time, not every person constantly monitors their blood pressure levels, so arterial hypertension is often detected very late.
Contact your cardiologist immediately if you regularly notice signs of hypertension such as:
- headaches in the occipital region;
- dizziness;
- “flies”, a veil before the eyes;
- noise in ears;
- rapid and increased heartbeat;
- unpleasant tightness or pain in the chest;
- swelling of the arms and legs, puffiness of the face.
Hypertensive crisis is an emergency condition caused by an excessively high level of blood pressure (for example, up to 200/110 mm Hg and above), it is characterized by: headache, tremor, increased heart rate, chills, nausea, vomiting, sudden fear of death, anxiety , facial redness, swelling, sweating, vision distortion.
1 Ophthalmoscopy in the diagnosis of hypertension
2 Ophthalmoscopy for hypertension
3 Taking tests to diagnose hypertension
results
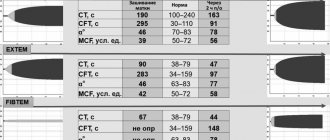
- The analysis included 9590 adults from the NHANES study (mean age 49 years, 52% women) and 8703 adults from the ARIC study (mean age 56 years, 57% women).
- The prevalence of isolated diastolic hypertension was 6.5% in NHANES according to 2017 ACC/AHA criteria and 1.3% according to JNC7 criteria. Absolute difference, 5.2% [95% CI, 4.7%-5.7%].
- According to the criteria, 0.6% of patients required antihypertensive therapy.
- Analysis of data from the ARIC study showed that isolated diastolic hypertension, according to the 2021 ACC/AHA criteria, was not significantly associated with the incidence of atherosclerotic cardiovascular disease (hazard ratio, 1.06 [95% CI, 0.89-1.26]) , heart failure (hazard ratio, 0.91 [95% CI, 0.76-1.09]) or chronic kidney disease (hazard ratio, 0.98 [95% CI, 0.65-1.11]).
Reasons for the development of arterial hypertension
The exact cause of the development of hypertension has not yet been established, however, a clear relationship has been identified between hypertension and the following factors:
- Exposure to stress;
- hereditary predisposition;
- age;
- gender (AH is more common in men);
- abuse of table salt;
- smoking and alcohol;
- endocrine disorders;
- excess body weight;
- physical inactivity;
- kidney diseases;
- increased adrenaline levels;
Complications of arterial hypertension
Under conditions of constantly elevated blood pressure, the walls of blood vessels thicken and lose their ability to relax, which prevents normal blood supply and saturation of tissues and organs with oxygen and nutrients. Various serious complications arise, including the following:
- Hypertensive crisis;
- myocardial infarction;
- stroke;
- angina pectoris;
- heart failure;
- cardiac ischemia;
- chronic renal failure;
- retinopathy;
- atherosclerosis, etc.