Classification
The upper limit of normal platelet count varies from 350,000 to 400,000 per microliter depending on the reference intervals of the specific laboratory performing the analysis. According to the degree of increase, the following types of thrombocytosis are distinguished:
- Soft
: from 350-400 to 700 thousand. - Moderate
: from 700 to 900 thousand. - Heavy
: from 900 to 1000 thousand. - Extreme
: over 1,000,000.
The cause of extreme and severe thrombocytosis is oncohematological pathologies. According to the origin of thrombocytosis there are:
- Primary
(tumor, clonal). They account for approximately 10-15% of all cases of thrombocytosis. The cause is tumor diseases of the blood system. - Secondary
(reactive). The most common variety (about 85%). The cause is infectious, systemic inflammatory processes, and anemia. - False
(pseudothrombocytosis). The reason is an error in the hematology analyzer, which mistakes tumor cell fragments during treatment with chemotherapy drugs, small red blood cells, or red blood cells that have undergone hemolysis as platelets. Pseudothrombocytosis is also observed with cryoglobulinemia. - Hereditary
(family). This is a rare genetic disease, the cause of which lies in a mutation of the genes encoding the synthesis of thrombopoietin and its receptors (THPO, MPL).
General blood test - transcript online
Using the online test interpretation service, you can check your results in a general blood test.
We take into account both the patient's gender and age, since the results can vary greatly in these cases. All parameter maps were compiled using medical literature. To start working with the service, indicate the gender and age of the person and select the parameters that interest you. Do not self-medicate. At the first signs of illness, consult a doctor.
The reasons why platelets in a child’s blood are higher than normal can only be determined through diagnostic measures. The clinical picture for a violation of this nature will be rather nonspecific, therefore it is strongly not recommended to independently compare the clinic and therapeutic measures. This is extremely dangerous for a child and can lead not only to complications, but also to death.
Diagnostically, an increase in platelets in a child’s blood is determined by laboratory tests. Instrumental diagnostics are carried out if necessary, depending on the current symptoms.
The prognosis is entirely individual, since everything will depend on the provoking factor and the age of the child, the state of his immune system.
Causes of thrombocytosis
Physiological conditions
An elevated platelet level does not always indicate pathology. There is physiological (short-term, transient) thrombocytosis, caused by various circumstances, for example, stress, intense physical activity. The reason is the mobilization of blood platelets, or rather their transition from the marginal position to the central blood flow in the vessels of the spleen and lungs.
In addition, minor physiological thrombocytosis is observed in children from the neonatal period to 11 years. There is also a so-called hemoconcentration thrombocytosis, which is caused by dehydration. This phenomenon is due to a decrease in the volume of the liquid part of the blood (plasma) and a relative increase in formed elements (platelets, erythrocytes, leukocytes). In this situation, it is necessary to focus on the hematocrit - with dehydration it is increased.
Infections
This is the most common cause of thrombocytosis (about 40%). An increase in the level of blood platelets develops when:
- Bacterial infections
. In adults, thrombocytosis occurs mainly with local (pneumonia, pyelonephritis, meningitis, endocarditis) and systemic (sepsis, tuberculosis) bacterial infections. - Viral and fungal infections
. Thrombocytosis occurs less frequently during infection with viruses (hepatitis B, C) and pathogenic fungi (aspergillosis). - Helminthiasis.
In children, parasitic infestations (toxocariasis, ascariasis) are recognized as a common cause of an increase in the number of blood platelets.
There are two pathogenetic mechanisms for the development of thrombocytosis in response to an infectious disease. First, during the fight against pathogens, leukocytes produce a large number of inflammatory mediators, including interleukin-6, which stimulates bone marrow megacaricytopoiesis (the formation of platelet precursors). Secondly, platelets themselves are part of the anti-infective immunity - they are able to produce bactericidal substances, capture, neutralize, and even phagocytose certain types of bacteria, viruses, and foreign particles.
Platelets facilitate the migration of leukocytes to the site of infectious inflammation by interacting with endothelial cells of the vascular wall. Thrombocytosis during infections occurs abruptly, correlates with the severity of the disease, and quickly resolves after the pathogen is eliminated from the body and the inflammatory process subsides. Thrombocytosis is usually mild or moderate; in septic conditions it can reach a severe degree; in children it is somewhat more pronounced than in adults.
Autoimmune diseases
Another common cause of thrombocytosis is considered to be chronic rheumatological pathologies that occur with autoimmune inflammation. The mechanism for increasing the content of blood platelets is the overproduction of substances such as interleukin-6, colony-stimulating factors, which activate bone marrow platelet formation. The degree of thrombocytosis corresponds to the activity of inflammation (minimal during remission, maximum during relapse).
In diseases such as rheumatoid arthritis, systemic lupus erythematosus (SLE), inflammatory bowel diseases (Crohn's disease, ulcerative colitis), a mild or moderate degree is observed. In systemic vasculitis with necrotizing destruction of vessel walls, severe thrombocytosis occurs, since in vasculitis, in addition to other inflammatory mediators, tumor necrosis factor is synthesized in large quantities, which also has a stimulating effect on platelet formation. High platelet counts are especially common in children.
Anemia
Iron deficiency anemia is often the cause of thrombocytosis, especially in children. The exact mechanisms of this phenomenon have not yet been clarified, but an inverse relationship has been clearly established between reduced levels of iron metabolism (ferritin, iron-binding capacity of serum) and an increased level of blood platelets. Iron is thought to have an inhibitory effect on the maturation of megakaryocytes (precursor cells).
In addition, some pluripotent stem cells in the bone marrow are unable to transform into red blood cells under conditions of iron deficiency. As a result, a kind of “bypass” occurs and a larger percentage of stem cells begin to mature along the megakaryocyte pathway. Thrombocytosis in iron deficiency anemia is mild, sometimes moderate. Platelets quickly return to normal after correction of iron deficiency and an increase in hemoglobin.
However, as anemia worsens, platelet levels drop to a state of thrombocytopenia. The cause of iron deficiency can be a lack of iron in food, increased iron consumption (growth period in children, pregnancy, lactation) or chronic blood loss (long menstruation, bleeding from the gastrointestinal tract due to gastric ulcer).
Malignant blood diseases
The cause of approximately 15% of all thrombocytosis is hemoblastosis - chronic myeloid leukemia, Ph-negative myeloproliferative pathologies (essential thrombocythemia, polycythemia vera, and primary myelofibrosis). The increase in the number of blood platelets in these diseases is due to clonal (tumor) transformation of the megakaryocyte lineage of the bone marrow due to various mutations, which leads to hyperproduction of platelets.
These diseases are more common in adults and older people, in children - only in exceptional cases. Initially, thrombocytosis is moderate, as it progresses it increases, reaching a severe or extreme degree, which is why microcirculation disorders, arterial and venous thrombosis of various localizations often occur. The concentration of blood platelets normalizes very slowly, only after courses of specific myelosuppressive treatment.
Splenectomy
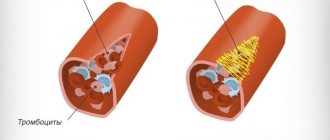
The spleen, being an organ that deposits blood, retains a large number of formed elements, including platelets. The spleen is also directly involved in thrombocytopoiesis, secreting the hormones thrombocytopenin and splenin, which suppress bone marrow maturation of megakaryocytes. Therefore, thrombocytosis after splenectomy is caused by two mechanisms: the release of platelets, normally located in the splenic depot, into the circulating blood, and the phenomenon of “disinhibition of the bone marrow,” i.e. increased platelet production.
An increase in the number of blood platelets does not occur immediately, but approximately a week after splenectomy, reaches a maximum by the 13-14th day (up to 700-800 thousand), often becoming the cause of venous thrombosis of the portal vein, and then slowly returns to normal over several weeks or months .
Injuries and surgeries
Massive tissue damage (wound during abdominal surgery, fracture, extensive burns) causes activation of the blood coagulation system, namely the vascular-platelet unit, which is the first stage of hemostasis. It involves vasospasm, as well as adhesion and aggregation of platelets at the site of damage to the vascular wall. The consumption of platelets stimulates their active release from the depot and a compensatory increase in their bone marrow production. The extent of damage correlates with the degree of thrombocytosis. This type of thrombocytosis usually does not require treatment.
Oncological diseases
The cause of thrombocytosis in solid (non-hematopoietic) tumors is the ability of cancer cells to produce interleukin-6, which stimulates thrombocytopoiesis. This feature was found in small cell lung cancer, colon adenocarcinoma, and malignant mesothelioma. In addition, tumor disintegration often causes bleeding, leading to iron deficiency anemia. The degree of thrombocytosis is usually moderate, in children it can be severe, and regresses after long-term treatment with chemotherapy.
Rare causes
- Functional asplenia
: sickle cell anemia, chronic alcoholism, celiac disease. - Use of medications
: vincristine, adrenaline. - Rebound phenomenon
: development of thrombocytosis 1-2 weeks after treatment of thrombocytopenia or discontinuation of medications that cause thrombocytopenia (methotrexate, vitamin B12, prednisolone).
Functions of platelet cells
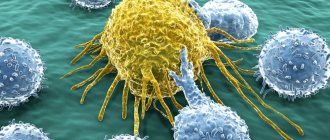
A specific feature of blood platelet cells is their ability to stick together and attach to the vascular intima due to special outgrowths (pseudopodia).
As a result, primary platelet clots are formed, which play an important role in the process of stopping bleeding.
Normally, the number of platelet cells in the blood can change significantly due to stressful situations, physical activity, exposure to a painful stimulus, viral and bacterial diseases (high platelets in a child under one year old are often associated with a past infection), etc.
It should be noted that in the implementation of the main function of platelets (participation in hemostasis processes), the presence of platelet cells on the granules and membrane surface plays an important role:
- specific platelet factors (partial thromboplastin, antiheparin factor, thrombostenin);
- vasoconstrictor factors (serotonin, adrenaline, norepinephrine);
- thromboxane;
- circulating immune complexes, etc.
The participation of platelets in the formation of immune responses is due to their phagocytic activity, the content of IgG, lysozymes and beta-lysines (lysozyme and beta-lysine are capable of destroying the membranes of some bacterial cells).
- Platelets - their role in the body and what threatens a deviation from the norm (increase or decrease in platelets)
Platelets also contain specific peptide factors that can stimulate the transformation of “null” lymphocyte cells into mature T- and B-lymphocyte cells.
Due to this, in case of vascular injuries, platelet cells not only help stop bleeding, but also prevent pathogenic microorganisms from entering the body.
Watch this educational film about platelets with your child:
Diagnostics
Thrombocytosis is detected in a clinical blood test. Although very high platelet counts are more common in hematologic diseases, platelet levels alone cannot determine the cause of thrombocytosis. Therefore, if it is detected, you should visit a therapist. The doctor carefully asks about the patient’s complaints, how long ago the symptoms occurred, and conducts a general examination of the patient. Then, based on the data obtained, an additional examination is prescribed, including:
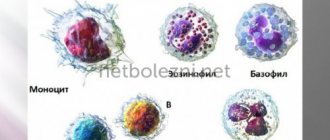
- Blood tests
. In a general blood test, the content of other formed elements (erythrocytes, leukocytes) is determined, and the leukocyte formula is calculated. The concentration of inflammatory markers (ESR, CRP) is measured. The indicators of serum iron, TBC, ferritin are assessed. The presence of autoantibodies (RF, ACCP, antibodies to the cytoplasm of neutrophils) is checked. In case of endocarditis and sepsis, an analysis for procalcitonin and presepsin is performed. - Pathogen identification
. To identify the pathogen, microscopy, bacterial culture of urine and sputum are performed. If tuberculosis is suspected, an intradermal test with tuberculin is prescribed. Using an enzyme immunoassay, antibodies to viruses, parasites, and fungi are detected, and using the polymerase chain reaction method, their DNA and RNA are detected. To diagnose meningitis, a cerebrospinal fluid analysis is informative. - Genetic research
. In patients with myeloproliferative pathologies, mutations of Janus kinase (JAK2V617F), thrombopoietin receptors (MPL), and erythropoietin are determined using fluorescent hybridization (FISH) and PCR. Sometimes chromosomal abnormalities are detected - trisomies, deletions. In chronic myeloid leukemia, cytogenetic analysis reveals the Philadelphia chromosome (Ph). - X-ray
. On an X-ray of the lungs, in case of pneumonia, foci of darkening and infiltrates are noted, in case of tuberculosis - enlargement of the mediastinal lymph nodes, expansion of the roots of the lungs, rounded shadows (cavities) of the upper lobes of the lungs. In patients with arthritis, x-rays of the joints show a narrowing of the joint space, areas of erosion, and marginal osteoporosis. - Ultrasound
. Ultrasound of the abdominal organs in case of pyelonephritis determines compaction and expansion of the pyelocaliceal system, and in case of blood diseases - splenomegaly. In bacterial endocarditis, cardiac echocardiography reveals vegetations of the valves and sometimes effusion into the pericardial cavity. - Endoscopy
. In patients with inflammatory bowel pathologies, fibrocolonoscopy is performed, which reveals hyperemia of the mucous membrane, lack of vascular pattern, erosion, and ulcerative defects. Crohn's disease is characterized by the "cobblestone pavement" symptom - alternating deep ulcers with unchanged mucous membrane. - Histological studies
. In bone marrow aspirate for malignant hematological pathologies, hyperplasia of the megakaryocyte lineage of hematopoiesis is noted (in polycythemia vera - all three lineages), a large number of blast cells (in myeloid leukemia), proliferation of reticulin and collagen fibers (fibrosis). In case of vasculitis, a biopsy of a vessel reveals pronounced perivascular infiltration with lymphocytes and plasma cells.
Platelet count according to Fonio
Correction
Conservative therapy
In most cases, to correct thrombocytosis, it is enough to eradicate the cause, i.e. treatment of the underlying disease. Short-term thrombocytosis that develops due to stress or drug administration does not require intervention. In case of persistent long-term thrombocytosis, consultation with a hematologist is necessary to identify the cause and prescribe appropriate treatment. Therapy for thrombocytosis has several areas, including:
- Fighting infection
. To eliminate the infectious agent, antibacterial (amoxicillin), antifungal (fluconazole), and antiparasitic agents (mebendazole) are used. Treatment of viral hepatitis requires long-term use of peligated interferon in combination with antiviral drugs. - Treatment of iron deficiency anemia
. Correction of iron deficiency is carried out with tablet preparations (iron sulfate). For children, there are forms of syrup and drops for oral administration. The addition of ascorbic acid promotes better absorption. - Therapy of autoimmune diseases
. Treatment of autoimmune diseases is carried out using medications that suppress inflammation - glucocorticosteroids (prednisolone), immunosuppressants (cyclophosphamide). - Targeted therapy
. For myeloproliferative diseases, specific targeted treatment is prescribed to slow down the progressive growth of the malignant tumor. These drugs include Janus kinase inhibitors (ruxolitinib), tyrosine kinase inhibitors (imatinib, dasatinib). - Symptomatic treatment
. To relieve high thrombocytosis, medications are used that suppress the activity of the megakaryocyte lineage, and, consequently, the production of platelets - anagrelide, interferon-alpha, hydroxyurea. For polycythemia, regular bloodletting is successfully used as a treatment method to remove excess formed elements. - Blood thinning
. In case of high thrombocytosis, antiplatelet agents (acetylsalicylic acid) are prescribed to prevent thrombosis. In case of contraindications (peptic ulcer of the stomach, duodenum), platelet receptor blockers (clopidogrel, ticagrelor) are used. In people at high risk of thrombosis (elderly, patients with diabetes mellitus or atrial fibrillation), anticoagulants (warfarin, dabigatran) are used.
Specialized treatment
The only method that allows achieving complete recovery from a malignant hematological disease is allogeneic bone marrow transplantation. This requires HLA typing to select a compatible donor. However, due to the high risk of developing life-threatening complications, this method is used only if conservative treatment is ineffective.
Thrombocrit - what is it?
Thrombocrit is a blood test indicator that indicates what proportion of whole blood consists of platelets. The value of this general analysis parameter is determined only by the hematology analyzer and is calculated using the formula:
platelet count * mean platelet volume (MPV) * 10-4.
The value of the PCT indicator is directly affected by the average platelet volume MPV, as well as factors such as smoking, lack of vitamins B12, B9, B6, and depressive disorders.
Knowledge of the study results allows us to assess the effectiveness of the blood coagulation system. The test indicator reflects the human body’s tendency to bleed or form blood clots.
A thrombocrit test is prescribed as part of a comprehensive examination:
- heart and blood vessels;
- kidney;
- reproductive organs;
- endocrine system;
- respiratory organs;
- immune system.
Based on the test results, the risk of possible complications during organ transplantation is assessed and the course of diseases during treatment with immunosuppressive drugs is predicted.
Knowing the PCT value allows one to assess the risk of thrombosis when prescribing medications that affect the parameters of the coagulation system. Such an assessment is necessary for drawing up a treatment regimen and predicting the outcome of the disease in bedridden patients, with artificial ventilation, and before surgery.
- What is thrombocrit (PCT), the norm in a blood test
Forecast
The outcome depends on both the underlying pathology and the degree of thrombocytosis. For example, acute viral infection and iron deficiency anemia are characterized by a benign course. Patients with essential thrombocythemia, with proper selection of pathogenetic and symptomatic treatment, can live more than 80 years. People with chronic myeloid leukemia, on the other hand, live about 5-10 years from diagnosis.
Since reactive thrombocytosis almost always occurs in children, their prognosis is favorable. Thrombosis is not typical for mild to moderate thrombocytosis. In extreme or severe cases, there is a very high probability of fatal thrombosis leading to myocardial infarction, pulmonary infarction, and ischemic stroke.