General information
Platelets are granulocytic blood cells without a biconvex nucleus, formed from plasma cells of the bone marrow. They are presented in different forms - young, adult and mature. The diameter is directly proportional to age: 2-4 microns. Platelets contain granules that create blood clotting proteins, lytic enzymes, phosphatase and cathepsin, create serotonin, calcium ions and ATP, and contain lysosomal enzymes.
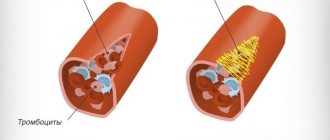
One of the most important functions of blood platelets is participation in blood clotting (primary hemostasis).
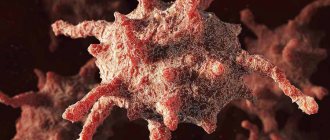
Platelets bind clotting factors, making blood clots thicker. As a rule, in an inactive state, when the vessel wall is damaged, platelets are directed to the damaged area. Thanks to the pseudopods located on the surface of the body, they are attached to each other and the vascular wall, forming a blood clot, which is an excellent barrier to bleeding. In the active state, platelets are able to change the shape of the body, due to which they increase their area, and this allows them to completely close the damage.
In addition, platelets are able to protect the body from foreign bodies by catching them with the help of pseudopods, and then digesting them with the help of the enzyme lysocine, which is formed from platelet factors (thrombin, thromboxane), from platelet granules. Thus, platelets are important for the immune response, being “killer” cells for foreign agents entering the body.
Blood plates serve as a storage site for serotonin, providing antitumor and radioprotective effects.
Thus, a violation of the number of platelets leads to inhibition of their functions, this certainly leads to disruption of the body’s activity and entails negative symptoms.
Cytoskeleton and shape change
The platelet cytosol is permeated by a three-dimensional network of water-insoluble protein threads (filaments), which forms the cytoskeleton. The filaments consist of polymerized actin protein and ensure that the platelet changes shape when activated. In addition, just below the plasma membrane is a membrane skeleton associated with the cytoplasmic “tails” of some receptors. It consists of short actin filaments connected to each other using special proteins. The membrane skeleton not only supports the plasma membrane, regulating the contours of the cell, and stabilizes it, preventing fragmentation, but also regulates the distribution of receptors attached to it in the plane of the membrane. It is also suggested that it plays an important role in the regulation of various intracellular events that are triggered upon activation.
Rice. 5.
Scanning electron micrographs of the process of spreading an activated platelet (
a–d
) over the surface []
Interestingly, the cytoskeleton is a dynamic structure, thanks to which a platelet can not only change shape, but also grow “tentacles” (filopodia). With their help, it spreads over the surface of the damaged vessel (Fig. 5) and more easily adheres to other platelets (Fig. 6). Relatively recently, it was discovered that upon strong activation (by thrombin alone or together with collagen), platelets are divided into two groups (subpopulations), very different in properties and even shape, which suggests a fundamentally different organization of the cytoskeleton in them. Some of them (“regular” activated) have the appearance of amoebas - lumps with filopodia, others (procoagulant, since there is a lot of phosphatidylserine on the outer surface of their membrane) - balls without “tentacles”. The data obtained in our laboratory indicate that some membrane receptors responsible for binding cells to the surface and to each other are unequally attached to the cytoskeleton in platelets from the two subpopulations. This means that they can interact differently with the damaged vascular wall and with each other in the forming blood clot.
The sequence of processes during the restructuring of the platelet cytoskeleton has generally been studied quite little, but here is a new question: why do some cells become “amoebas” when activated, and others become “balls”?
Normal platelet count in blood
The number of platelets in the body should normally vary from 180 to 320*10^9 for women and from 200 to 400*10^9 for men per liter of blood. Moreover, the number of platelets in women can change during menstruation to 75 * 10^9 per liter of blood, can decrease in the third trimester in pregnant women and, regardless of gender, increase in response to an inflammatory reaction, which seems to be a physiological norm and is not a deviation, without carrying negative symptoms.
In children, the normal platelet count depends directly on the age of the child. For a newborn, the norm will be 100-420*10^9 per liter of blood, and at two weeks of age and up to a year it is 150-350*10^9 per liter of blood. Up to five years, the amount changes slightly to 180-350*10^9 per liter of blood. By the age of seven, the norm reaches 180-450*10^9 per liter of blood.
For prevention, you need to take a blood test at least once a year in order to identify a possible pathology as early as possible and begin its treatment as soon as possible at an early stage, before the development of a severe clinical condition. If a deviation is detected, a blood test is performed more often.
They live in the body for only 9-10 days, after which they are renewed, destroyed in the liver or spleen and re-proliferate in the bone marrow.
Online consultation with infectious disease specialist, allergist-immunologist Natalia Nikolaevna Gordienko
Cost of online consultation: 3500 rubles
Online consultation
During the consultation, you will be able to voice your problem, the doctor will clarify the situation, interpret the tests, answer your questions and give the necessary recommendations.
How to treat pathology
Scientists do not know why the bone marrow begins to produce more megakaryocytes, which increase the production of blood platelets, and what to do to normalize their number. This means that therapy comes down not to eliminating the cause of the pathology, but to treating the consequences. Excess blood cells are treated with medication. Appointed:
- drugs that reduce blood clotting (anticoagulants);
- medications that prevent platelets from sticking together (antiplatelet agents);
- interferon, which stimulates the immune system;
- Anagrelide is a drug that inhibits the formation of platelets from megakaryocytes.
Advertising:
In some cases, when there is a tendency to further increase, doctors resort to the procedure of plateletpheresis. The blood is separated to reduce the excess level of blood cells. It must be remembered that blood viscosity increases:
- hormonal drugs;
- contraceptives;
- diuretics;
- smoking;
- alcohol.
Information about these factors should be reported to your doctor.
Causes of low platelet count in blood test
A decrease in the number of platelets in a general blood test below normal to 150*10^9 per liter of blood and below is a pathological condition and is called “thrombocytopenia”. Since this is a condition, not a disease, it only characterizes, being a symptom of a specific disease.
There can be many reasons for a decrease in platelets, and they are all different from each other, so it can sometimes be very difficult to name one at once.
The main causes of thrombocytopenia are:
- Increased platelet destruction.
- Increased platelet consumption.
- Insufficient platelet production.
These three conditions can be the result of an inherited condition in which enzyme activity is impaired, but more often it is an acquired condition due to:
- Suppression of bone marrow activity.
- Hemoblastosis (tumor disease of hematopoietic or lymphoid tissue).
- Disseminated vascular coagulation syndrome (due to various bacterial infections or brain injury).
- Vitamin B12 deficiency.
- Folic acid deficiency.
- Hypersplenism syndrome (an increase in the size of the spleen, as well as an increase in the destruction of blood cells).
- Hemorrhagic diathesis (increased bleeding).
- Immune thrombocytopenia.
- Thrombocytopenic purpura.
- Leukemia (malignant disease of the bone marrow, otherwise called blood cancer).
- Paroxysmal nocturnal or cold hemoglobinuria.
- Collagenosis (connective tissue damage).
Additional reasons for a decrease in platelets in the blood may also be:
- Violation of medication regimen (vancomycin, heparin, sulfamethoxazole, drugs for the treatment of diabetes mellitus).
- Use of chemotherapy drugs.
- Massive blood transfusion.
- Cirrhosis of the liver.
- Myelofibrosis.
- Hepatitis C virus.
- Human immunodeficiency virus (HIV).
- Epstein-Barr virus (infectious mononucleosis).
- Hyperthyroidism.
- Hypothyroidism.
- Hemolytic-uremic syndrome.
- Alcoholism.
Correction
Conservative therapy
In most cases, to correct thrombocytosis, it is enough to eradicate the cause, i.e. treatment of the underlying disease. Short-term thrombocytosis that develops due to stress or drug administration does not require intervention. In case of persistent long-term thrombocytosis, consultation with a hematologist is necessary to identify the cause and prescribe appropriate treatment. Therapy for thrombocytosis has several areas, including:
- Fighting infection
. To eliminate the infectious agent, antibacterial (amoxicillin), antifungal (fluconazole), and antiparasitic agents (mebendazole) are used. Treatment of viral hepatitis requires long-term use of peligated interferon in combination with antiviral drugs. - Treatment of iron deficiency anemia
. Correction of iron deficiency is carried out with tablet preparations (iron sulfate). For children, there are forms of syrup and drops for oral administration. The addition of ascorbic acid promotes better absorption. - Therapy of autoimmune diseases
. Treatment of autoimmune diseases is carried out using medications that suppress inflammation - glucocorticosteroids (prednisolone), immunosuppressants (cyclophosphamide). - Targeted therapy
. For myeloproliferative diseases, specific targeted treatment is prescribed to slow down the progressive growth of the malignant tumor. These drugs include Janus kinase inhibitors (ruxolitinib), tyrosine kinase inhibitors (imatinib, dasatinib). - Symptomatic treatment
. To relieve high thrombocytosis, medications are used that suppress the activity of the megakaryocyte lineage, and, consequently, the production of platelets - anagrelide, interferon-alpha, hydroxyurea. For polycythemia, regular bloodletting is successfully used as a treatment method to remove excess formed elements. - Blood thinning
. In case of high thrombocytosis, antiplatelet agents (acetylsalicylic acid) are prescribed to prevent thrombosis. In case of contraindications (peptic ulcer of the stomach, duodenum), platelet receptor blockers (clopidogrel, ticagrelor) are used. In people at high risk of thrombosis (elderly, patients with diabetes mellitus or atrial fibrillation), anticoagulants (warfarin, dabigatran) are used.
Specialized treatment
The only method that allows achieving complete recovery from a malignant hematological disease is allogeneic bone marrow transplantation. This requires HLA typing to select a compatible donor. However, due to the high risk of developing life-threatening complications, this method is used only if conservative treatment is ineffective.
Consequences of low platelet count
In a state of low platelet count, disorders subsequently develop, which include frequent bleeding (menstrual and nosebleeds), while the bleeding time increases significantly and becomes difficult to stop. Sudden gum bleeding may develop (not everyone does). Blood clots may be found in urine or stool. Petechiae (red dots resulting from damage to the capillary wall) appear on the skin of the lower extremities, most often the legs. Even minimal damage leads to the formation of ecchymoses (bruises), when normally a bruise would not appear.
The severity of symptoms directly depends on the platelet count. The fewer platelets, the more severe the clinic. If the platelet count is very low, internal bleeding into the digestive tract or even bleeding into the brain may occur.
Even in the presence of a mild clinic, it is recommended to consult a general practitioner in order to prevent this condition.
Platelet diagnostics
At the first appearance of relevant clinical symptoms (bleeding and bruising), it is necessary to consult a specialist, in this case it is a general practitioner. There is no need to postpone going to the doctor until the clinic gets worse, because in this case the treatment will be more difficult and the outcome will be less favorable.
To diagnose thrombocytopenia, you must first take a blood test. If the analysis reveals a low platelet count, the general practitioner may refer you to a hematologist, who will prescribe additional tests, such as:
- Coagulogram with determination of clotting time.
- Blood biochemistry for LDH, ASAT, ALAT and bilirubin.
- Antibody test.
- MRI.
- Ultrasound of the abdominal organs.
- Genetic studies (to exclude hereditary thrombocytopenia).
After conducting research and identifying the true cause of thrombocytopenia, a general practitioner or hematologist prescribes appropriate treatment, which includes eliminating the cause of the decrease in platelet count.
Online consultation with infectious disease specialist, allergist-immunologist Natalia Nikolaevna Gordienko
consultation cost: 1000 rubles
Online consultation
During the consultation, you will be able to voice your problem, the doctor will clarify the situation, interpret the tests, answer your questions and give the necessary recommendations.
Tibetan healing methods
Diagnostics in Tibetan medicine, in addition to traditional methods, includes:
- Inspection
. The specialist examines the general appearance of the patient: body features, posture, how he walks, how he speaks. Carefully examines the condition of the eyes, tongue, skin, and lymph nodes. - Survey
. The doctor collects a detailed medical history: finds out what events preceded the onset of the disease, what lifestyle the patient leads, how he reacts to stressful situations, and what food preferences he has. - Pulse diagnostics
. Based on the nature of the pulse, a doctor of Tibetan medicine determines the condition of each individual organ and the body as a whole, and identifies the disease in its very infancy.
Depending on the diagnosis, the patient is prescribed individual treatment. In oriental medicine centers, it consists of a set of therapeutic measures and procedures that make it possible to eradicate the real cause of the disease, and not just eliminate visible clinical symptoms. Much attention is paid to correcting the patient’s lifestyle, including a transition to proper nutrition, the introduction of reasonable physical activity and achieving a balanced state of the nervous system.
A set of external procedures, including energy acupressure, acupuncture, stone therapy, moxotherapy, vacuum therapy, restores energy balance, normalizes regulatory and metabolic processes, activates organ functions, and improves blood circulation. Herbal medicine is an effective method of treating thrombocytosis. Tibetan herbal remedies and Baikal herbs cleanse the blood and tone the walls of blood vessels.
Prevention
There is no specific prophylaxis for thrombocytopenia. It is recommended to lead a healthy lifestyle, including proper nutrition, normal sleep, not to overload yourself with work, abstain from drinking alcohol and tobacco products, treat infectious diseases in a timely manner and carry out routine vaccinations. Consult a doctor promptly if there is a sudden disturbance in the body’s functioning.
Author: infectious disease doctor. Allergist-immunologist Natalia Nikolaevna Gordienko
Summarizing
Our study made it possible to describe a new mechanism of cell redistribution within the thrombus: during contraction, “slippery” procoagulant platelets are mechanically squeezed onto the surface of the thrombus, forming a heterogeneous structure of its outer part.
But the point has not yet been made in determining the role of procoagulant platelets in hemostasis. The formation of a weakly adhesive, that is, unsuitable for the adhesion of new cells, layer of dying cells and fibrin on the surface of the thrombus can help stop its growth by reducing the efficiency of fixation of non-activated platelets brought by the blood stream. However, this hypothesis requires further research.
It is pleasant to note that an important contribution to this work was made by young co-authors - students of the Department of Biophysics of the Faculty of Physics of Moscow State University - Roman Kerimov and Alexandra Yakusheva, as well as a student of the Faculty of Fundamental Medicine of Moscow State University Taisya Shepelyuk (Fig. 4). The results of the work were published in one of the leading journals of the American Cardiovascular Association and reported at several international conferences, including the Gordon Conference on Hemostasis.
Figure 4. Roman Kerimov, Alexandra Yakusheva, Taisya Shepelyuk and Dmitry Nechipurenko
This version is a modification of a note that was published in the physics department newspaper “Soviet Physicist”.
The author expresses gratitude to Anastasia Masaltseva and Yuri Nechiporenko for their assistance in editing the article, as well as to all his colleagues - co-authors of the original work.