Article for the “bio/mol/text” competition: The mechanism for stopping bleeding is essential for the body's survival, but despite decades of research, many details of this system remain unclear. Eight years ago, Mikhail Panteleev told Biomolecule about blood clotting. Since then, a lot of new data has accumulated in this area. In this article we will tell you how a young team of scientists from Moscow State University lifted the veil of secrecy over two mysterious phenomena in the complex system of arterial thrombus formation, showing how dying cells move in it.
Basic functions of platelets
In appearance, platelets are round or oval red plates with a smooth surface. They are formed in the bone marrow. They mature in approximately 8 days. These components constantly circulate in the bloodstream.
The main function of platelets is to ensure blood clotting. In addition, the ability of these blood components to stop bleeding is important. This is ensured by the fact that individual platelets can stick together and stick to sites of vascular damage. The process is automatically started by the human body when there is a risk of bleeding.
An important question is how long platelets live. Their viability time lasts approximately 10 days. Depending on the age of the red plates, their size changes: from 2 to 5 microns in diameter.
The process of platelet renewal in the blood occurs constantly. Therefore, an important factor to ensure the maintenance of blood condition is the balance between the formation of red plates and their death. Otherwise, there may be a tendency to blood clots or increased bleeding.
Concept of platelets
The plates are oval or round in shape. When they reach surfaces on which there is no epithelial layer, the formation of special processes is activated. These branches are intended to stop emerging bleeding and close wounds; their length is 5-9 times greater than the size of a platelet.
The granules of the plates contain platelet enzymes that destroy bacterial membranes and protect the body from harmful microorganisms. The processes serve to accelerate movement in the bloodstream by adhering to foreign bodies; the threads capture elements and digest them. A protective barrier is created by gluing with other platelets, that is, blood clotting occurs.
An important function of platelets is to supply micronutrients to the endothelial layer. Their lifespan ranges from 7 to 12 days, then destruction occurs in the liver, lungs and spleen.
Forms of platelets in the blood:
- degenerative varieties - contained in amounts up to 0.2%;
- stereotypes of irritation - range from 0.8 to 2.3%;
- young cells - from 0 to 0.8%;
- mature forms - from 90.2 to 95%;
- old records - from 2.3 to 5.7%.
Inactivated elements are flattened spherical shapes, in which the semi-axes are located one to the other in a ratio of 2:8. This feature is used in the case of recognizing the optical characteristics of platelets and when regenerating parameters using flow cytometry.
Cell structure
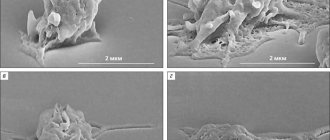
Microscopic studies show that the change in cell shape upon activation is associated with transformation of the tubule ring. This phenomenon is caused by the conversion of the amount of calcium ions.
The structure of platelets is heterogeneous, there is heterogeneity, and the structure contains several layers:
- the outer surface is represented by a three-layer membrane, the thickness of which contains phospholipase A, receptors for adhesion to other elements and tissues;
- the lipid layer is a collection of glycoproteins and helps the plates stay glued together for a long time;
- microtubules in the form of a cellular framework help the structure contract to release the contents of the platelet beyond its boundaries;
- The area of organelles is represented in the structure by various components and factors that promote wound healing.
In the early periods of research, there was no photographic technique and there was no unambiguous terminology, so the time of initial observations of platelets is not precisely established. There is information that the first study was conducted by the inventor of the microscope, the Dutchman van Leeuwenhoek. In England, the cells are now called platelets, a term coined by Bizzocero in 181. He is also credited with the discovery of the relationship of elements with homeostasis and thrombocytosis. In Russian, flat blood cells are called platelets, sometimes the name Bozzocero's plaque is used.
Formation and life cycle
Their formation and maturation begins in the body of the red marrow in the area of the pelvic bones and vertebrae. The spongy substance reproduces stem cells that are incapable of the process of differentiation and are not divided into specific types.
Platelets go through several stages during formation:
- stem cells turn into elements of the megakaryocyte series;
- the formation of a megakaryoblast begins - a large formation of a mesh structure without granules, with 2-3 round nuclei;
- the resulting proplatelet turns into a promegakaryocyte and platelet formation occurs.
Transformations occur as a result of the influence of genetic factors. The lack of cells leads to an increase in the duration of bleeding; the increased volume of elements causes the formation of clots and blockage of blood vessels. As a result of blocked channels, a heart attack, stroke, pulmonary embolism, or vascular plug in other organs of the human body can occur.
Inferiority of platelets or their deficiency is called thrombocytopathy. A low overall indicator of the number of plates in the analysis causes a consequence in the form of thrombotic purpura, in which ischemia of various organs or hemolytic anemia develops, and the number of blockages in the vessels after bleeding increases.
Functions of elements
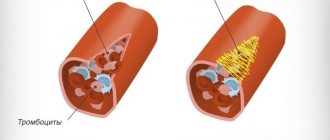
Platelets form the primary plug to tighten the wound of a damaged vessel and accelerate the plasma coagulation reaction. The peculiarity of the plates is that they play a significant role in the healing and restoration of tissues, while releasing polypeptide molecules for cell growth and division. Platelets are quickly activated when needed and enter a new, irreversible state.
The plates are transformed under the influence of pathogens:
- the main protein of connective tissue - collagen;
- the main protein of the coagulation system - thrombin;
- adenosine monophosphate produced by damaged cells - ADP;
- a second-line activator synthesized by platelets to establish vasoconstriction - thromboxane A2.
The modified flat cells attach to the damaged surface and form a plug as a result of adhesion to the walls and each other. As a result, the shape of the plates is updated, and phosphatidylserine and P-selectin are expressed.
In its normal state, the platelet membrane does not support the blood clotting procedure, while phospholipids are located on its inner layer. Activation of flat elements causes excitation of scramblase protein molecules, which transfer phospholipids to the outer shell. As a result, the concentration of phosphatidylserine in both layers is equalized. In the process, transmembrane proteins of the exogenous layer change, which accelerate coagulation through the characteristic coupling of factors.
Blood test for platelets
A complete blood test can determine the platelet count. The main indications for its implementation are the following:
- Increased bleeding of gums.
- Heavy menstruation.
- The appearance of bruises from minor impacts.
- Frequent nosebleeds.
- Difficulty stopping bleeding from minor injuries.
The number of platelets in the blood is measured in thousands per 1 microliter of blood. Counting is carried out in specialized laboratories in various ways that guarantee high accuracy.
The normal platelet count in the blood depends on gender and age and is:
- For men, 200–400 thousand.
- In women, 180–320 thousand, during menstruation the amount can decrease to 75–220 thousand, and during pregnancy to 100–310 thousand.
- In children, indicators depend on age, and the corresponding values are given in special tables.
To conduct a general blood test, blood is taken from a finger. No special preliminary preparation is required before this. To ensure accurate results, it is better to donate blood in the morning on an empty stomach. At the same time, 12 hours before the procedure it is not recommended to consume fatty spicy foods, carbonated drinks, and alcohol.
Additionally, to determine blood clotting indicators, Sukharev and Lee-White tests are performed. They are informative and allow you to obtain the necessary additional data about the pathological condition. This will allow you to carry out correct treatment measures and avoid dangerous consequences.
What we found and how we did it
Biophysical approach
Like any complex system, the formation of a blood clot in an artery needs to be managed. Identifying the mechanisms that regulate biological processes is one of the traditional tasks of biophysics, so the problem of regulating arterial thrombus formation has long attracted the attention of not only doctors and physiologists, but also biophysicists. For more than two decades, the Department of Biophysics of the Faculty of Physics of Moscow State University has been developing a direction related to the analysis of the principles of the structure and regulation of the hemostasis system: for example, in the classic works of Professor F.I. Ataullakhanov and his students demonstrated the autowave nature of the propagation of the blood plasma coagulation process in the absence of flow [5], [6].
Establishing the mechanisms that regulate thrombus formation in arterial blood flow is one of the main tasks of our research team, whose members are Professor of the Department of Medical Physics M.A. Panteleev, Professor of the Department of Biophysics F.I. Ataullakhanov, senior researcher Department of Biophysics D.Yu. Nechipurenko, as well as students and graduate students of the Faculty of Physics.
In vitro and in silico study
Recent studies carried out by us in collaboration with colleagues from France and the USA made it possible to link the surface distribution of dying platelets with the process of thrombus compression [7]. Using confocal microscopy in in vitro thrombus experiments, we showed that procoagulant platelets form in various parts of the growing thrombus and then move to its surface (Fig. 1).
Figure 1. Dynamics of movement of procoagulant platelets in a thrombus. a — Confocal micrographs of thrombi at different time points. Green color corresponds to the fluorescence of dying cells (a fluorescent marker of cell death is used). b — Blood clots at different points in time. Green color corresponds to the fluorescence of dying cells, purple color corresponds to the fluorescence of platelets attached to the thrombus (a fluorescently labeled antibody to the surface proteins of the platelet is used). c — The main quantities used to analyze the movement of platelets are the movement vector d , the translocation angle α between the direction of movement and the initial radius vector of the center of the dying cell, drawn from the center of the thrombus. d — Results of analysis of the modules of average movement speeds and translocation angles of dying cells (green) and “fresh” platelets attached to the surface of the thrombus (purple). Scale: 10 micrometers.
[7]
This redistribution is accompanied by the formation of fibrin on the surface of the thrombus. Since dying (procoagulant) platelets interact rather weakly with other cells and do not participate in the contraction process, it has been suggested that their redistribution is the result of mechanical displacement during the process of active compression of the thrombus. To test this hypothesis, a computer model of platelet aggregate compression was created, which demonstrated the functionality of the formulated hypothesis (Fig. 2).
Figure 2. Simulation of cell aggregate contraction. a — Platelet aggregate before and after compression. Spheres imitating procoagulant cells, which do not participate in the contraction process and interact relatively weakly with other spheres, are marked in green. Contraction is described as a decrease in the equilibrium length of the pair potential (Morse) interaction between the centers of the spheres. b — Aggregate before and after contraction, in which the “procoagulant” spheres, initially located inside the aggregate, had different radii. The spheres that remained inside the aggregate after contraction are marked in purple, and those outside the aggregate in green. c — The value of the absolute values of the movements of procoagulant platelets in experiments (ex vivo) and “procoagulant” spheres in the model (in silico). d — The fraction of spheres displaced as a result of compression of the aggregate onto its surface. Calculation results for spheres of different radii are shown.
[7]
An important evidence base for the work was experiments with the blood of unique genetically modified mice, whose platelets are deprived of the ability to exhibit mechanical activity and, therefore, ensure thrombus contraction. In accordance with the predictions of the model and the formulated hypothesis, dying cells did not move to the surface of the thrombus in the absence of contraction (Fig. 3). The lack of surface distribution of dying platelets was also accompanied by the lack of surface localization of fibrin.
Figure 3. Comparison of the distribution of procoagulant cells and fibrin for normal and genetically modified mice. a — Distribution of procoagulant platelets (green) in normal mice (top panel) and modified mice (bottom panel). The outline of the thrombus, constructed from the image in the differential interference contrast mode, is marked in yellow. b — Analysis of the ratio of the total fluorescence of the surface of dying cells located outside the dense part of the thrombus to the fluorescence of the same surfaces inside the thrombus for normal (WT) and genetically modified mice (MYH9). c — Distribution of procoagulant surfaces (green) and fibrin (purple) in thrombi from wild-type mice (top panel) and thrombi from genetically modified mice (bottom panel). Scale: 10 micrometers.
[7]
Increased platelet levels
Elevated platelets are a pathological condition. It is called thrombocytosis. The main danger of the pathology is the increased risk of blood clots.
The cause of an increase in the level of platelets in the blood can be various diseases. Most often thrombocytosis occurs against the background of:
- Malignant neoplasms.
- Infectious diseases.
- Helminthic infestations.
- Surgical operations.
- Autoimmune pathologies.
- Kidney failure.
High levels of platelets in the blood are observed in older people. Temporarily, indicators may increase after heavy physical exertion, for example, after playing sports.
The symptoms of thrombocytosis are characteristic, but mild. It is imperative to conduct a general blood test if the following symptoms are noted:
- Pain in the fingers and toes.
- Itching of skin surfaces.
- Unreasonable weakness, which leads to decreased performance.
- Lack of appetite.
Competition "bio/mol/text"-2019
This work was published in the “Own Work” category of the “bio/mol/text” competition 2019.
The general sponsor of the competition and partner of the Skoltech nomination is the Skoltech Center for Life Sciences.
The nomination partner is the Russian Science Foundation.
Competition sponsor: the largest supplier of equipment, reagents and consumables for biological research and production.
The audience award was sponsored by BioVitrum.
"Book" sponsor of the competition - "Alpina Non-Fiction"
Specialists and non-specialists are well aware of the ominous word “thrombosis”. The word “thrombus” is traditionally perceived as something dangerous. However, not all blood clots are dangerous. If the vascular wall is damaged, the body must quickly form something like a plug that will prevent blood from flowing out of the artery or vein. Thus, the formation of plugs, or, in scientific terms, hemostatic blood clots , is a key task that is solved by the human hemostasis system (and, of course, not only humans). However, sometimes this system fails, and damage to the vessel leads to the formation of a massive intravascular thrombus, which almost completely blocks blood flow. If this process occurs in a large artery that supplies blood to a vital organ, such a blood clot can cause serious complications and even death. Myocardial infarction and ischemic stroke are perhaps the most well-known and common complications caused by arterial thrombosis, which are today the most common cause of death and disability in people in developed countries [1].
Why in some cases, in response to damage, the hemostasis system works excessively and forms a deadly plug in the vessel? Despite many decades of research, this question remains unanswered. The lack of understanding of the mechanisms that regulate the formation of a blood clot leads to the fact that today there is no reliable way to prevent thrombosis: taking existing antithrombotic drugs is associated with a fairly high risk of bleeding, including life-threatening ones.
Decreased platelet levels
Low platelet levels, the norm of which differs between men and women, provoke the development of a condition known as thrombocytopenia. Very often it occurs against the background of uncontrolled use of medications: antidepressants and antibiotics.
The reasons for a decrease in the level of platelets in the blood can be various infectious diseases: ARVI, hepatitis, herpes, etc. Thrombocytopenia can be observed when a large number of blood thinning products are included in the diet. These are ginger, cherries, garlic, onions, etc.
Non-infectious factors that reduce the level of platelets in the blood include pregnancy, vitamin deficiency, alcohol or heavy metal poisoning.
Thrombocytopenia can be suspected based on the following signs:
- Heavy menstruation.
- Frequent nosebleeds.
- The appearance of hematomas.
With a constant pathological decrease in the level of platelets in the blood, the risks of developing severe bleeding and stroke conditions, which are life-threatening, increase.
Restoring platelet levels in the blood
You can normalize the level of platelets in the blood with a balanced diet. It is important to saturate your diet with foods high in materials and microelements. You need to give up spicy food, alcohol, fast food and sweet carbonated drinks, lead a healthy lifestyle and maintain a drinking regime.
If it is not possible to normalize the indicators using natural methods, then you need to undergo a full examination by a hematologist. If platelet levels are elevated, special medications may be prescribed - anticoagulants or antiplatelet agents. They thin the blood and minimize the risk of blood clots. But at the same time, they should be taken only as prescribed by a doctor. It should be understood that stabilization of the condition is possible only after eliminating the underlying causes that provoke deviations from the norm.
Consequences of low platelet count
In a state of low platelet count, disorders subsequently develop, which include frequent bleeding (menstrual and nosebleeds), while the bleeding time increases significantly and becomes difficult to stop. Sudden gum bleeding may develop (not everyone does). Blood clots may be found in urine or stool. Petechiae (red dots resulting from damage to the capillary wall) appear on the skin of the lower extremities, most often the legs. Even minimal damage leads to the formation of ecchymoses (bruises), when normally a bruise would not appear.
The severity of symptoms directly depends on the platelet count. The fewer platelets, the more severe the clinic. If the platelet count is very low, internal bleeding into the digestive tract or even bleeding into the brain may occur.
Even in the presence of a mild clinic, it is recommended to consult a general practitioner in order to prevent this condition.