Atherosclerosis is a chronic disease of the arteries, which occurs due to disturbances in fat and protein metabolism and is accompanied by the deposition of cholesterol and lipoproteins on the inner walls of blood vessels. These deposits form in the form of plaques. Due to the subsequent proliferation of connective tissue (sclerosis) and calcification of the vessel walls, deformation and narrowing of the lumen occurs, leading to blockage of the vessel. The main danger of atherosclerosis is a significant increase in the risk of developing coronary heart disease. Due to the fact that the disease is becoming the main cause of this and other serious health problems, the prevention and treatment of atherosclerosis must be given due attention.
Treatment of atherosclerosis is complex and includes a number of measures related to lifestyle correction, dietary changes, giving up bad habits, as well as drug treatment that helps restore normal metabolism in the body.
What it is
Atherosclerosis is one of the most common chronic arterial diseases. Because of it, an atherosclerotic plaque of cholesterol (cholesterol) forms in the wall of the vessel. These plaques narrow the lumen of the vessel, which affects blood flow, and in extremely advanced cases, plaques can completely block the blood flow. If this happens in a large artery, then the situation is fraught with serious complications, including death: cardiovascular diseases have been one of the main causes of mortality for many years. In addition, the presence of a plaque in a vessel changes the flow of blood: turbulence appears, which contributes to the formation of blood clots (platelet sticking together). The appearance of blood clots poses a risk of their breaking off and clogging the vessel in a narrow place.
Literature
1. Pavlova O.S. Modern possibilities of effective cardiovascular prevention in patients with arterial hypertension and dyslipidemia. Honey. news. 2012; 1:62–68. 2. Arterial hypertension, lipid metabolism disorders and atherosclerosis. V.V. Kukharchuk. In “Guide to Arterial Hypertension” / Ed. E.I.Chazova, I.E.Chazova. M.: Media Medica, 2005; 289–299. 3. Klahr S., Morrissey JJ The role of vasoactive compounds, growth factors and cytokines in the progression of renal disease. Kidney Int. 2000; 57; Suppl 75:7–14. 4. Wolf G. The Renin-Angiotensin System and Progression of Renal Disease. Jn: Contributions to Nephrology. Editor G. Wolf. 2001. 5. Delcayre C., Swynghedauw B. Molecular mechanisms of myocardial remodeling. The role of aldosterone. J. Mol. Cell. Cardiology. 2002; 34:1577–1584. 6. Ross R. Atherosclerosis an inflammatory disease. N Engl J Med. 1999; 340:115–26. 7. O'Donnell VB. Free radicals and lipid signaling in endothelial cells. Antiox Redox Signal. 2003; 5: 195–203. 8. Wolfrum S., Jensen KS, Liao JK Endothelium-dependent effects of statins. Arterioscler Thromb Vasc Biol. 2003; 23: 729–36. 9. Kaplan M., Aviram M. Oxidized low density lipoprotein: atherogenic and proinflammatory characteristics during macrophage foam cell formation. An inhibitory role for nutritional antioxidants and serum paraoxonase. ClinChem Lab Med. 1999; 37:777–87. 10. Campese VM, Bianchi S., Bigazzi R. Association between hyperlipidemia and microalbuminuria in essential hypertension. Kidney Int. 1999; 56(Suppl 71):S10–3. 11. Diagnosis and treatment of arterial hypertension. Systemic hypertension. 2010; 3:5–26. 12. Oshchepkova E.V., Dmitriev V.A., Titov V.N. et al. Indicators of nonspecific inflammation in patients with hypertension. Ter. Arch. 2007; 12: 18–25. 13. Breiser A., Recinos A., Eledrisi M. Vascular inflammation and the renin-angiotensen system. Atherioscler. Thromb Vasc. Biol. 2002; 22; 1257–1266. 14. Verma S., Bucshanan M., Anderson T. Endothelial function testing as a biomarker of vascular disease. Circulation. 2003; 108:2054–2059. 15. Sesso H., Burning J., Rifai N. et al. C-reactive protein and the risk of developing hypertension. JAMA. 2003; 290:2945–2951. 16. Niscanen L., Laaksonen D., Nyssonep K. et al. Inflammation, abdominal obesity and smoking as predictors of hypertension. Hypertension. 2004; 44(6):859–865. 17. Fliser D., Buchholz K., Haller H. For the European Trial on Olmesartan and Pravastatin in Inflammation and Atherosclerosis (EUTOPIA) Investi Circulation. 2004; 110:1103–7. 18. Stumpe KO, Agabiti-Rosei E., Zielinski T. et al. Carotid intima-media thickness and plaque volume changes following 2-year angiotensin II-receptor blockade. The Multicentre Olmesartan atherosclerosis Regression Evaluation (MORE) study. Ther. Adv. Cardiovasc. Dis. 2007; 1:97–106. 19. Smith RD, Yokoyama H, Averill DB et al. The protective effects of angiotensin II blockade with olmesartan medoxomil on resistance vessel remodeling (The VIOS study): rationale and baseline characteristics. Am J Cardiovasc Drugs. 2006; 6 (5): 335–42. 20. Smith RD, Yokoyama H., Averill DB, Schiffrin EL, Ferrario CM Reversal of vascular hypertrophy in hypertensive patients through blockade of angiotensin II receptors. J Am Soc Hypertens. 2008; 2: 165–172. 21. Hirohata A., Yamamoto K., Miyoshi T. et al. Impact of olmesartan on progression of coronary atherosclerosis a serial volumetric intravascular ultrasound analysis from the OLIVUS (impact of OLmesartan on progression of coronary atherosclerosis: evaluation by intravascular ultrasound) trial. J Am Coll Cardiol. 2010; 55 (10): 976–82. 22. Naya M., Tsukamoto T., Morita K. et al. Olmesartan, but not amlodipine, improves endothelium-dependent coronary dilation in hypertensive patients. J Am Coll Cardiol. 2007; 50 (12): 1144–9. 23. Lorenzen JM, Neuhoeffer H., David S. Angiotensin II receptor blocker and statins lower elevated levels of osteopontin in essential hypertension – results from the EUTOPIA trial. Atherosclerosis. 2010; 209(1):184–8. 24. Takiguchi S., Ayaori M., Uto-Kondo H. et al. Olmesartan improves endothelial function in hypertensive patients: link with extracellular superoxide dismutase. Hypertens Res. 2011; 34 (6): 686–92. 25. Pimenta E., Oparil S. Impact of olmesartan on blood pressure, endothelial function and cardiovascular outcomes. Integr Blood Press Control. 2010; 3:113–23. 26. Hirohata A., Yamamoto K., Miyoshi T. et al. Four-year clinical outcomes of the OLIVUS-Ex (impact of Olmesartan on progression of coronary atherosclerosis: evaluation by intravascular ultrasound) extension trial. Atherosclerosis. 2012; 220(1):134–8. 27. Brunner HR The new oral angiotensin II antagonist olmesartan medoxomil: a concise overview. J Hum Hypertens. 2002; 16(Suppl. 2):S13–16. 28. Corsini A. et al. Blood Pressure. 1998; 7(Suppl 2): 18–22. 29. Catapano A. Cardiologia. 1997; 42(Suppl 3): 19–26.
Causes and prevention of atherosclerosis
The cause of atherosclerosis is a disorder in fat metabolism - the accumulation of cholesterol (namely low-density lipoproteins) in excess quantities. Cholesterol is necessary for the body because... participates in many important processes such as the production of certain hormones, and is also part of the cell membrane. With a genetic predisposition to the accumulation of cholesterol, with an unbalanced diet, this substance becomes too much, the body cannot cope with its breakdown, and the excess begins to be deposited in the walls of blood vessels, leading to atherosclerosis.
Factors contributing to the development of atherosclerosis are considered to be: high blood pressure, diabetes mellitus, excess weight, stress, smoking, alcohol, age over 50 years. It is worth noting that the development of the disease often begins at a young age, and by the age of 50-60 the main symptoms appear.
A good method of preventing atherosclerosis is an active lifestyle, balanced physical activity and the fight against excess weight, if present.
Most resources also offer a balanced diet, or more precisely, reducing the consumption of animal fats as the main method of preventing atherosclerosis, i.e. the appearance of excess cholesterol. But some studies indicate that vegetable fats and carbohydrates can provoke an increase in blood cholesterol levels. Therefore, in your approach to your own nutrition, you should be guided by common sense and moderation. Both animal and vegetable fats are necessary for the body to function comfortably, and their excess (like an excess of any other substances) can lead to lipid metabolism disorders. But all researchers agree that consuming vegetables and fruits, adding fish to the diet, and moderate calorie intake are key and proven methods for preventing problems with blood vessels and more.
Nicotinic acid derivatives
Niacin, or nicotinic acid for atherosclerosis, is one of the most “deserved” drugs that has been used to treat hyperlipidemia since 1955 [6]. It acts only after being converted into nicotinamide in the body and subsequent binding to the coenzymes codehydrase I and codehydrose II, which transfer hydrogen.
The distinctive effects of nicotinic acid compared to other lipid-lowering drugs are the ability to significantly increase HDL levels, as well as a vasodilating effect.
The lipid-lowering effect of niacin requires higher doses than necessary for the vitamin effect to occur. On average, the dose of nicotinic acid as a lipid-lowering agent is 100 times higher than as a vitamin [1].
The mechanism of action is based on inhibition of triglyceride lipolysis in adipose tissue. Niacin reduces the synthesis of VLDL, reduces the level of total cholesterol, LDL, triglycerides and increases the content of HDL by 15-30%. The drug also has antiatherogenic properties [5].
Along with the hypolipidemic effect, nicotinic acid dilates small vessels (including cerebral vessels), improves microcirculation, and has a weak anticoagulant effect.
Triglyceride levels begin to fall within 1–4 days after starting to take nicotinic acid, while cholesterol levels drop on days 5–7 of using the drug.
Side effects
Along with quite powerful lipid-lowering properties, niacin is poorly tolerated. Up to 40% of patients refuse to take it due to side effects [6]. One of the side effects associated with low compliance is a feeling of heat and flushing due to the release of prostaglandins. This effect can be reduced by gradually titrating the dose and administering acetylsalicylic acid at a dose of 250 mg half an hour before taking nicotinic acid.
With the use of high doses of nicotinic acid (usually 2–6 g per day), skin itching and dyspepsia—vomiting and diarrhea—may occur. There is a risk of peptic ulcers, liver dysfunction, and increased levels of glucose and uric acid in the blood. Due to the possible development of hyperuricemia, nicotinic acid is contraindicated in gout. It is also not recommended for use in diabetes mellitus and metabolic syndrome [1, 3].
Due to the poor tolerance of nicotinic acid, its derivatives were synthesized with a higher safety profile. Xanthinol nicotinate has become one of the most prescribed.
What should I warn the client about?
Niacin, due to its vasodilating effect, can potentiate the effect of antihypertensive drugs and lead to a sudden decrease in blood pressure, so it should be used cautiously during antihypertensive therapy, after consultation with a doctor [7].
Nicotinic acid is recommended to be taken with meals.
Diagnostics
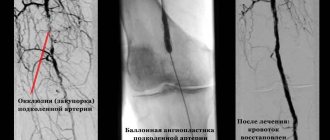
To diagnose atherosclerosis, both laboratory and instrumental methods can be used:
- general blood analysis;
- blood cholesterol level test;
- angiography (injection of a contrast agent into the blood, which reflects X-ray radiation and gives the specialist a detailed map of the condition of the vessels of the entire body);
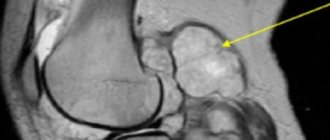
- CT, MRI;
- coronary angiography (to study the coronary arteries);
- ECG, echocardiography (echocardiography);
- Holter ECG monitoring (to detect disturbances in heart rhythms);
- Ultrasound (to study the condition of the aorta, kidney vessels, heart).
Diagnostics usually does not cause problems for an experienced doctor - for this, our center has all the necessary equipment. After all, modern high-tech devices will be required - the better the equipment, the more detailed the examination data will be, which will help the doctor choose the optimal treatment method.
Treatment
Treatment of atherosclerosis of the coronary vessels of the heart requires a heterogeneous, complex approach and a long period of time. After accurately compiling the clinical picture of the disease, medications and therapeutic measures are prescribed, which include:
- Hypolydemic drugs for removing excess lipids and fluid from body tissues from blood vessel cells;
- Beta blockers, inhibitors to reduce the heart's oxygen demand. During treatment, this reduces myocardial activity and the severity of symptoms.
- Anticoagulants to eliminate the possibility of blood clots.
- Prescribing a special diet;
- Prohibition of smoking and alcoholic beverages;
- Moderate therapeutic physical activity to prevent stagnation;
- Weight loss to normalize metabolic processes and remove toxic substances from the body.
Atherosclerosis of the cerebral arteries
When cholesterol plaques form and the arteries of the brain narrow, the brain cells experience a lack of blood and nutrients. The following symptoms may indicate this condition:
- periodic dizziness,
- noise in ears,
- headache,
- increased fatigue,
- disturbances in coordination of movements.
The narrowing of the main carotid artery supplying the brain is identified as a separate diagnosis - carotid artery stenosis. Damage to the vessels supplying the brain carries the threat of a serious disease - ischemic stroke of the brain.
Stages of disease development
There are 3 stages in the pathogenesis of atherosclerosis. Systemic arterial damage occurs against the background of changes in protein and lipid metabolism.
First
At the initial stage, a fat spot is formed. In areas of vessel branching, microcracks appear on the walls, and a local slowdown in blood circulation occurs. The walls of blood vessels swell and become loose, but thanks to protective mechanisms the body still manages to dissolve lipids.
When these resources are depleted, complex compounds of lipids and proteins are formed. They are deposited on the inner surface of the vascular walls.
Second
In areas of lipid deposits, connective tissue begins to grow: an atherosclerotic plaque is formed. At an early stage of formation, it has a semi-liquid form and undergoes dissolution.
But there is also danger at this stage. Due to their loose structure, plaques can spread and clog arteries. The vascular walls lose their elasticity and become ulcerated, which leads to the formation of blood clots.
Third
The plaque thickens and calcium salts accumulate in it. Gradually it grows, narrowing the arterial lumen. The blood supply to the organ that the artery supplies is disrupted. When the lumen of a vessel is blocked by a blood clot or plaque decay products, a heart attack or gangrene develops.
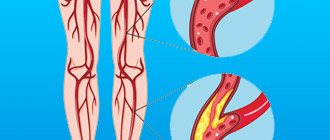
Atherosclerosis of the arteries of the lower extremities
Damage to the arteries of the lower extremities is called obliterating atherosclerosis. People over 65 years of age, especially men, are susceptible to it. This disease manifests itself in the following symptoms:
- pain in the calves, cramps at rest;
- pain when walking, causing you to limp;
- numbness in the legs, fatigue when walking;
- the appearance of non-healing wounds, and in advanced cases - ulcers.
If you do not consult a doctor in the presence of such symptoms, then there will be a threat of limb amputation as the only treatment measure for extremely advanced cases of obliterating atherosclerosis.
Atherosclerosis of the coronary arteries
Atherosclerosis of the coronary arteries (which bring blood to the tissues of the heart) is one of the main causes of coronary heart disease and myocardial infarction: when the disease affects the vessels of the heart, heart muscle cells begin to die due to insufficient nutrition. And the risk of blood clot formation and vessel blockage only aggravates the situation. This condition is extremely dangerous, life-threatening and requires consultation with a doctor. You should pay special attention to possible symptoms:
- chest pain;
- feeling of heaviness, tightness in the chest;
- arrhythmia, i.e. fast or slow heartbeat;
- feeling of a sinking heart.
Do not underestimate the above symptoms. Let us remember that the risk of developing atherosclerosis is present in many people. Complications of the disease without proper treatment are so dangerous that you should consult a doctor, even if you are afraid of a confirmed diagnosis or surgery. Modern medicine has advanced far in the treatment of atherosclerosis of various localizations.
Symptoms
The danger of atherosclerosis of the coronary vessels of the heart lies in the absence of symptoms in the first stages of development. The disease can “silently” destroy arteries over many years. As a rule, the first signs appear in middle age, after 45 years. During this time, negative processes in the vessels reach a critical level and are manifested by the following symptoms:
- Pain in the heart area, left shoulder and under the shoulder blade;
- Discomfort, burning sensation under the ribs;
- Shortness of breath while walking and in a completely horizontal position;
- General weakness, dizziness;
- Constant slight nausea.
Nonspecific symptoms of cardiac atherosclerosis are often mistaken by patients for the manifestation of other diseases that have similar symptoms. This makes it difficult to make a diagnosis in the early stages, when the prognosis for treatment is favorable in the vast majority of cases.
Progressive atherosclerosis of the heart vessels is manifested by more serious symptoms:
- Angina pectoris. Short-term attacks of pain in the heart area, radiating to the shoulder blade, arm, abdominal cavity and lower jaw. Occur after physical activity, eating spicy food or emotional stress. They last no more than 15-20 minutes, the symptoms disappear after resting or taking sedatives, for example, validol.
- Cardiosclerosis. The process of development of atherosclerosis is in the active stage - scarring and replacement of muscle tissue with inferior compounds occurs. It manifests itself as constant mild to moderate pain, swelling of the extremities, shortness of breath, fatigue, and decreased physical activity.
- Arrhythmia. The frequency and sequence of heartbeats is disrupted. The patient experiences paroxysmal pain, a feeling of cardiac arrest, dizziness, fainting, and abnormal tremors in the chest area.
Heart failure. The rupture of a cholesterol plaque is accompanied by the formation of a blood clot, which clogs the artery. The blood stops carrying oxygen and nutrients. The heart stops working normally. Severe, burning pain in the chest, nausea appear, the patient feels short of air, limbs swell, and clouding of consciousness appears.
Important! With acute failure, the risk of developing myocardial infarction increases to 90%. If an attack is accompanied by a rupture of an aneurysm, death occurs.
Depending on how quickly the patient seeks medical help, the prognosis of atherosclerosis will be positive or unfavorable. If the pathology is advanced to such an extent that foci of necrosis begin to form in the myocardium, then a significant threat to life arises.