Mastitis is an inflammation of the breast tissue. Any woman can get mastitis, regardless of whether she is breastfeeding or not, and even babies, including boys, but since breastfeeding women are mostly affected, mastitis is often declared a companion to breastfeeding.
“Dress warmly, otherwise you’ll catch a cold and get mastitis,” says the caring grandmother to the young mother, who diligently wraps herself up. To be fair, we note that there is some truth in these words - a cold body can more easily catch some disease, a sore throat, for example, and only then an untreated infection can cause mastitis. Prevention of such a disease is a healthy lifestyle in general - hardening and treatment of chronic infections (tonsillitis, caries) BEFORE pregnancy.
Acceptable pressure levels during breastfeeding
Even children know the correct blood pressure indicator - it is 120/80 mm Hg. But not all people correspond to this value, because everyone has always been a little higher, a little lower, a little lower. This is what you should follow. Normal blood pressure is considered a person who feels well.
The period of breastfeeding is a very important time in the life of every young mother, because it is responsible not only for your health, but also for the well-being and development of your baby. That's why a nursing mother should be careful and think that everything is fine. You cannot underestimate your condition, because only when the mother feels comfortable, the child is calm and joyful.
If the pressure increases to 135/85 mm Hg, there may not be any negative consequences.
When it increases above - 140/90 and much more, and the well-being of the deterioration of the deterioration of the deterioration of privacy, this is already treatment in the clinic.
Antipyretics during breastfeeding
09.09.2021
Women, when they learn about their “interesting” situation, and after the birth of a child, begin to be much more anxious
treat your health. In essence, there is nothing surprising in this - now they are responsible for small
a defenseless creature that is affected by any changes in the mother’s health. Therefore, as soon as they appear
Some signs of illness in the mother, this immediately causes panic.
The most common phenomenon during lactation is fever in a nursing mother. Previously, in such cases, the baby
She was immediately weaned off the breast and isolated from her mother until her complete recovery. In fact, this tactic is not correct,
especially in the first months of a child’s life. The later you switch your baby to artificial complementary feeding, the better, because
Mother's milk contains everything a baby needs.
If you have a fever, do not panic. First of all, it is worth understanding what caused its increase.
Most often they are seasonal viral infections, milk stagnation (lactostasis), poisoning, mastitis (inflammation of the mammary gland ),
as well as various possible other infections and inflammations. Each of these ailments has its own symptoms and signs, and in order to
In order not to confuse one with the other, understand this thoroughly. For example, ARVI is characterized mainly by a runny nose , sore throat and
/or dry cough, general weakness of the body, possible enlargement of lymph nodes. Lactostasis is characterized by the appearance of compactions
in the chest , which can be felt, and pain in these places, redness of the skin of the chest , low blood pressure and general weakness.
Mastitis is accompanied by the same symptoms as lactostasis, but other symptoms of mastitis will help to distinguish one from the other: very high
temperature (above 39 degrees), the formation of soft areas the chest the chest , indentations may remain in it.
We believe you are already familiar with the signs of poisoning. Here, in addition to the elevated temperature, nausea and vomiting, abdominal , diarrhea ,
headache, pale skin, drowsiness, fainting, etc.
The above symptoms will help you narrow down your suspicions, but in order to accurately determine the disease, you need to consult a specialist.
Only he has the right to prescribe treatment methods for you. Be sure to tell your doctor that you are breastfeeding : then he will be guided by what
to prescribe you the most harmless drugs possible.
However, if the temperature is already quite high, and there is no time to wait for the doctor , you need to know what medications can be taken during the period
lactation, and which ones are best to abstain from. We strongly do not recommend taking acetylsalicylic acid or aspirin - in children, and especially
in such small children, it can cause a very dangerous reaction, sometimes even fatal. Worthy substitutes for this antipyretic
are ibuprofen and paracetamol. Both of these medicinal substances are not only sold under their own name, but are also included in many
other antipyretics. Based on paracetamol, for example, you can buy Panadol and Tylenol at the pharmacy, and based on ibuprofen -
Advil, Brufen and Nurofen. Both paracetamol and ibuprofen also have analgesic and anti-inflammatory properties.
During breastfeeding you need to be especially vigilant with the dosage. Any antipyretic should be taken no more than 4 times a day, 1 tablet.
The course of such treatment should be minimal - no more than 3 days. If during this period the temperature has not completely subsided, it is necessary to undergo a second
examination: perhaps the cause of the elevated temperature is different than what the doctor , and the treatment is also necessary differently. Not worth it for a long time
time to “sit” on the above-mentioned paracetamol and ibuprofen: in large quantities they negatively affect liver .
If the temperature does not rise much - up to 38-38. 5 degrees - then you can try to “bring it down” with folk remedies. The simplest and most accessible means
lowering the temperature is honey - dilute 1 tbsp in a glass of warm water. l. honey Infusions of cranberries, lingonberries, and raspberries help well. Also reduces well
temperature and nettle: pour a tablespoon of dried nettle leaves with a glass of boiling water, and leave (preferably in a thermos so that the water does not cool) for an hour.
Take this medicinal drink 4 times a day – you will definitely feel better.
Published in Pregnancy and pregnancy management Premium Clinic
High blood pressure during breastfeeding
High blood pressure during breastfeeding is not uncommon today. This phenomenon is associated with the stress on the myocardium during pregnancy, when the muscles of this organ are very taxed to ensure the proper functioning of the body of the woman and her child. Also, changes in the hormonal levels of a pregnant woman contribute to heart disease.
Therefore, at every visit to the appetite clinic, the doctor who notices it measures the blood pressure. Its cost shows to what extent the stern woman's circulatory clamshell is able to function properly.
To alleviate the condition of the elderly, a mother can have an experienced doctor who can prescribe such drugs so as not to harm the child.
The course of treatment for hypertension during breastfeeding will be significantly differentiated, in this case including only approved medications and respectful diets.
Features of treatment
If a woman suffers from cardiovascular diseases, she should purchase a blood pressure monitor, which should always be at hand. It is important that blood pressure can be measured at any time. After calling an ambulance, you should do the following:
- take the most comfortable position for yourself, do not get up, so as not to cause further harm;
- take medications prescribed by the doctor;
- if you feel chills, take measures to warm up;
- Don’t be nervous so that your blood pressure doesn’t increase even more.
If hypertension is caused by gestosis, the woman is admitted to the hospital, where it is easier to control the situation.
Any medications during lactation are prescribed with great caution. Many of them can enter the baby's body along with milk. In some cases, complete abstinence from taking medications is recommended. If the blood pressure is persistently elevated, Nifedipine or Methyldopa is prescribed. Medicines such as Verapamil and Dopegit are also allowed. If there is a sharp jump in blood pressure, you should take valerian or motherwort. As a rule, in such cases a course of treatment is prescribed.
The following drugs are prohibited during lactation:
- diuretics;
- ACE inhibitors;
- beta blockers;
- No-shpa injections.
If high blood pressure during breastfeeding is accompanied by pain, you should drink meadowsweet tea, mistletoe tincture or hawthorn juice.
You can prepare a healing bath. For example, sea or table salt is added to the water, after which a bottle of valerian is poured into it. The duration of the procedure is 10−15 minutes. You can also soak several handfuls of clay in a small volume of liquid and grind the mixture until a homogeneous mixture is obtained. Water is poured into the bath, the temperature of which should not exceed 37 degrees. The resulting mass is placed in it, you also need to add a head of crushed garlic. The clay bath should be taken for 25-30 minutes, during the procedure you can massage the body.
And also read on our website: The effectiveness of exercise therapy: benefits and contraindications for hypertension. Set of exercises
Why does breastfeeding mothers have high blood pressure?
High blood pressure in the paragraph is caused by the following factors:
- Excessive dependence on coffee, tea, licorice root tincture;
- overwork, stress, lack of sleep;
- smoke;
- hereditary predispositions that reveal themselves after pregnancy;
- take medications that increase smooth muscle tension - oxytocin, methylerometry;
- various cardiovascular disorders;
- diabetes;
- Difficult childbirth or complications after it;
- Problems with the endocrine system.
If excess pressure begins to develop, blood pressure readings gradually increase. Regardless of the reasons that led to hypertension, medical care is necessary to prevent the development of the disease. If nothing is done in this direction, after a while you may notice that it is taking effect and finally leading to pathological changes in the body.
Causes of high blood pressure
Normal blood pressure ranges from 120/80 mmHg. Art. It is worth sounding the alarm when reaching 140/90 mm Hg. Art. Due to constant changes, lactostasis may develop, and there is a possibility of congestion in the chest. When infection gets into breast milk, the risk to the baby's health increases.
Often, blood pressure increases due to depression, especially if the birth was not easy and the woman spent a lot of effort. The following provoking factors are identified:
- hormonal imbalance;
- cardiovascular diseases;
- pathologies of the endocrine system;
- polycystic ovary syndrome;
- bad habits, abuse of strong tea and coffee;
- constant stress;
- lack of normal sleep;
- heredity;
- long stay in a stuffy room.
Often, blood pressure increases due to an increase in circulating blood volume caused by an increase in the baby's nutritional needs. Thus, more milk begins to flow, the body functions with increased load.
The situation with increased blood pressure cannot be left to chance. If changes occur frequently, you should definitely visit a specialized medical specialist. It is possible that a woman will have to undergo restorative therapy aimed at correcting her hormonal levels.
Signs of high blood pressure
When the pressure increases, the feeding mother feels the following symptoms:
- Headache;
- nausea;
- Black spots before her eyes;
- chills;
- Fast impulse;
- Breathing and breathing;
- Problems with vision.
Even some of the above-mentioned symptoms indicate improper functioning of the cardiovascular system. It often precedes pregnancy, but even after pregnancy, symptoms of hypertension can persist during breastfeeding.
Diagnostic methods
Since this disease is very serious and can cause both heart attacks and strokes, the dieter must necessarily undergo research to determine the causes in which hypertension occurred so that doctors can prescribe effective treatment.
Complex diagnostics includes the following methods:
- General blood and urine analysis.
- Blood chemistry. They use it to test for anemia from iron deficiency.
- Electrocardiogram (ECG).
- Ultrasound of the thyroid gland, heart and abdominal cavity.
- Echocardiography.
- Computed tomography of the kidneys and adrenal glands.
- Urography and aortography.
Carrying out the necessary tests will not only reveal the fact of hypertension in a nursing mother, but also determine its causes and begin effective treatment.
Lactostasis due to high blood pressure
Lactostasis is a blockage of the milk duct. Most often it occurs in first-time mothers in the first days after starting breastfeeding.
This condition can be caused by high blood pressure, but the problem is complex. Inability to express milk and non-compliance with the frequency of feeding the newborn, as well as tight underwear. The thoracic ducts can become worse due to stress and exposure to cold. All these factors also lead to breast swelling.
Therefore, you should take care of yourself and make sure that inattention and high blood pressure do not cause galactorrhea in the mammary glands.
Development of lactostasis
Often, elevated blood pressure becomes a trigger for the development of lactostasis. This phenomenon is caused by blockage of the thoracic ducts, as a result of which milk can stagnate in the mammary glands. Primipara women often complain of lactostasis; a painful condition is observed in the first week. The provoking factor may be improper feeding and pumping.
And also read on our website: What is stage 2 hypertension, risk of cardiovascular disease 4: causes, symptoms and treatment of the disease
Hypothermia and stressful conditions can provoke stagnation of milk, but not so often. Sometimes pathology is caused by the use of underwear of the wrong size, which pinches the milk ducts.
Due to high pressure, swelling occurs, and if the breasts suffer, lactostasis may appear. In this situation, prompt treatment is required, as the likelihood of developing purulent mastitis, which is even more dangerous, increases. When milk remains in the duct for a long time, fermentation begins, and non-purulent inflammation begins. Such conditions are excellent for the development of infectious processes.
The risk of the disease increases if a woman sleeps on her stomach. During the postpartum period, it is very important not to neglect the hygiene of the mammary glands and genital organs. Not only the care itself plays a role, but also extreme attentiveness to unpleasant sensations.
First aid
In case of a sharp increase in blood pressure, you should immediately try to normalize it and seek medical help. If this is not the first time a nursing woman finds herself in a dangerous condition, you need to get a tonometer and have it at hand.
If the ambulance has not arrived yet, in this situation you should:
- Lie down comfortably so as not to put your health at greater risk;
- ask others to open the windows and let cool, fresh air into the room;
- lower your blood pressure with medications (if this is not the first time and the doctor has previously prescribed them for hypertension)
- Place a hot water bottle on your feet to warm them up if you feel shaky;
- stay calm or drink valerian extract to find emotional balance.
After doing all these steps, wait until the doctor tells him about the medications you took.
Permitted and prohibited drugs
In this situation, the question arises, what can be taken for blood pressure while breastfeeding, since most of the drugs pass into milk?
There are such drugs. Here they are:
- Nifediline.
- Methyldol.
- Verapomil.
- Dolegit.
Although these drugs are not absorbed into breast milk, they may cause decreased milk supply. To normalize blood pressure, the tablet is placed under the tongue. The doctor prescribes the drug, determines the duration of its use and dosage.
There are also drugs that are completely prohibited for use by nursing mothers:
- Beta-blockers (Atenolol, Nadolol).
- ACE inhibitors.
- Atgiotensin receptor blockers (reserpine).
- Diuretics (furosemide).
- Antispasmodics (No-shpa, Dibasol, Papaverine).
A nursing woman bears full responsibility for her health and the health of her child, so she should not take medications without the participation of a specialist.
Drug therapy during breastfeeding
- Levadnaya Anna Viktorovna
- Zhdanova Svetlana Igorevna
Summary
The importance of breastfeeding for the health of mother and child is currently beyond doubt. However, there are many reasons that can prevent full breastfeeding. In particular, drug therapy prescribed during lactation often leads to a temporary cessation of breastfeeding, often unjustified. This may lead to premature termination of breastfeeding. This article highlights the difficulties of prescribing drug therapy during lactation, the contradictions between existing international recommendations and the instructions for the drug, reflects current aspects of the pharmacokinetics of drugs in breast milk and provides practical recommendations on the way to solving the issues listed above.
Key words: lactation, breastfeeding, drug therapy, pharmacodynamics of drugs, pharmacokinetics of drugs, drugs in nursing, antibacterial therapy during lactation, physiology of lactation
For citation: Levadnaya A.V., Zhdanova S.I. Drug therapy during breastfeeding // Neonatology: news, opinions, training. 2021. T. 7. No. 4. P. 79-84. doi: 10.24411/2308-2402-2019-14006 The article was received by the editor on July 6, 2019. Accepted for publication on September 30, 2019.
The importance and necessity of breastfeeding today leaves no doubt. The benefits of breastfeeding for both the child and the mother have been proven by many scientific studies, so the issue of breastfeeding while taking various medications in hospitals is acute [1].
Many mothers are inappropriately advised to stop breastfeeding or avoid taking necessary medications due to fears of adverse effects on their children. This cautious approach is generally not justified because only a small proportion of drugs are truly contraindicated in breastfeeding mothers or are associated with adverse effects on their babies [2].
For example, in Russian practice, breastfeeding is often stopped in mothers with epilepsy who take valproic acid drugs (Convulex), although scientific studies demonstrate low penetration of valproic acid into breast milk and the absence of side effects in children whose mothers took these drugs during lactation [3] .
Domestic and foreign data on the admissibility of using a particular substance by a nursing woman contradict each other. This situation is explained by the fact that it is not economically profitable for the manufacturer to conduct studies of the drug during lactation and go through the full procedure for registering the substance as safe during lactation. According to the instructions, most drugs used in the postpartum period are not recommended during lactation [4].
All medications used by the mother should be reviewed on a case-by-case basis for potential contraindications.
When prescribing medications on the territory of the Russian Federation, the doctor must follow the official instructions of the manufacturer, which is regulated by Order of the Ministry of Health of Russia dated May 10, 2017 No. 203n “On approval of criteria for assessing the quality of medical care” [6]. On the website https://grLs.rosminzdrav.ru you can find instructions for drugs produced by different manufacturers [5]. Most drugs have not been studied by the manufacturer during breastfeeding, and the risks to the baby have not been assessed.
Information for clinicians regarding the extent of excretion of a particular drug into breast milk is necessary but may not be available [7]. To decide whether a particular drug is acceptable to use worldwide, the LactMed database https://toxnet.nLm.nih.gov [8] is used - a free and authoritative guide to the compatibility of drugs with lactation for prescription and over-the-counter drugs, which is published by the National Medical Library of the US National Institutes of Health. This resource contains all currently known data on drug levels in breast milk and infant serum, possible adverse effects on breastfed and lactating infants, and recommendations for alternative medications. The data is based on scientific research into breast milk and the penetration of various drugs into it. This database is updated every 1-2 months. There is also a free application for mobile devices on the LactMed website [9].
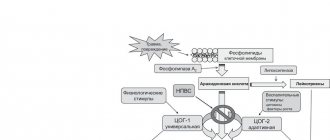
Pharmacokinetics and pharmacodynamics of drugs in breast milk
Drug diffusion into breast milk is driven primarily by concentration gradients that allow passive diffusion of non-ionized and free (non-protein-bound) drugs. Drug concentrations in breast milk are largely determined by drug concentrations in maternal serum [7]. Serum concentrations are generally lower when taking drugs with a large volume of distribution and fluctuate when taking drugs with a short half-life. There is also retrograde diffusion of drug from breast milk, whereby the drug can pass from the milk back into the plasma even if the mother has not emptied the breast [10]. Drugs that are high in protein, have a large molecular weight, or are poorly lipid soluble are rarely excreted in breast milk in clinically significant quantities. In the early postpartum period, large spaces between the alveolar cells of the mammary gland allow some substances to pass into breast milk that may not pass into mature milk. These gaps close by the 2nd week of lactation. Drug exposure during breastfeeding depends on the drug concentration in breast milk and the amount of breast milk consumed by the infant [7, 10]. The pharmacological activity of the drug depends on its absorption, distribution, metabolism and absorption by the child.
Criteria for assessing the risks of using medicines
The extent to which a child is exposed to substances taken by the mother depends on a number of factors.
1. Concentration of the drug in the maternal blood serum. Typically, drugs diffuse into and out of breast milk according to changes in maternal serum concentrations.
2. Penetration and concentration of the drug in milk. It does not depend on the volume of lactation. Drugs that have low lipid solubility or have a high molecular weight do not pass into breast milk. An example is the oral cephalosporin antibiotic ceftibuten. In the instructions.
3. Absorption of the drug in the child’s gastrointestinal tract. If the drug is not absorbed when taken orally, then even its significant concentration in breast milk will not lead to undesirable effects in the child. For example, the aminoglycoside antibiotic gentamicin, which has low bioavailability when administered orally.
4. Toxicity of the drug. Some pharmacological agents, even in small quantities, can have extremely adverse effects on many organs and systems of the child.
5. The risk of developing an allergic reaction in a child.
6. The ability of drugs to accumulate in the baby’s body even when small quantities are ingested.
7. Experience in using drugs in children. Medicines that are approved for use directly in children are usually safe because the doses transferred through breast milk are much lower than the therapeutic doses given to children.
8. Gestational age and age of the child. The risk of drug toxicity is higher in premature and sick infants and is rare in children older than 6 months.
9. Bioavailability of the drug. Young children are not usually affected by medications with low bioavailability, such as insulin or heparin.
The benefits of breastfeeding for both the infant and mother must be weighed against the risk of infant exposure to the drug.
As an example demonstrating the discrepancy in Russian instructions and international approaches when using drugs during lactation, we can illustrate the recommendations for a number of drugs common in hospital obstetric practice (see table).
Practical recommendations
Minimizing the potential risk to children when the mother takes medications may include the following recommendations.
1. Avoid drug therapy whenever possible.
2. Use topical therapy whenever possible.
3. Medicines that are safe for use directly on the baby are generally safe because the doses transferred through breast milk are much lower than therapeutic doses.
4. Medicines that are safe during pregnancy are not always safe for nursing mothers.
5. Use reliable links to obtain information about the use of medications while breastfeeding.
6. If different manufacturers have different instructions for the same drug, in hospitals it is advisable to choose when purchasing drugs from those manufacturers whose instructions allow breastfeeding while taking the drug they produce.
When choosing medications:
■ select drugs with the shortest half-life and highest protein binding capacity;
■ choose medications that have been well studied in children;
■ choose intravenous medications with poorer oral absorption;
■ Select drugs with the lowest lipid solubility.
Dosing of drugs:
■ the longer the interval between taking the medicine and breastfeeding, the lower its concentration in milk;
■ It is necessary to breastfeed the baby before the mother takes medications again. Infant exposure to medications can be minimized by taking medications after breastfeeding and before the infant sleeps for long periods of time.
When prescribing drugs that are not recommended for breastfeeding according to the LactMed database, a woman is recommended to temporarily stop breastfeeding and express to maintain lactation (from two mammary glands for about 15-20 minutes per breast, and in the case of expressing colostrum - 5-7 minutes ; at least every 3 hours (or at least 8 times a day), not focusing on the volume of expressed milk. If necessary, contact a breastfeeding specialist. With the constant use of drugs prohibited during breastfeeding, a collective decision is made to suppress lactation.
As of 2015, the US Food and Drug Administration (FDA) stopped using risk categories (ABCDX) to indicate the perceived safety of drugs during pregnancy. The ABCDX system was replaced by the FDA with the PLLR (Pregnancy and Lactation Labeling Rule) system, obliging the manufacturer to include 3 new categories of mandatory information in the drug instructions: clinical trial data on the effect of the drug on pregnancy and childbirth; lactation; on reproductive potential [27]. This entailed a change in some instructions for drugs registered in the Russian Federation: data from clinical studies began to appear in them, including during lactation. On the one hand, this introduced objectivity, on the other, contradictions appeared in them.
Let us consider this contradiction using the example of valproic acid preparations. The instructions say: “the excretion of valproic acid into breast milk is low, its concentration in milk is 1-10% of its concentration in the blood serum. There is limited data on the use of valproic acid during breastfeeding, and therefore the use of the drug during this period is not recommended. Based on the literature data and limited clinical experience, breastfeeding can be considered during monotherapy with valproic acid, but the side effect profile of the drug, especially the hematological disorders it causes, should be taken into account” [3]. From this instruction it follows that taking valproic acid drugs during lactation is not recommended, but is not prohibited, since existing clinical studies report drugs from this group as one of the safest during lactation [28], which gives reasons to doctors motivated to breastfeeding and mothers should be prescribed these drugs during lactation on a strictly individual basis under the control of the child’s coagulogram and platelets. There are similar contradictions in the instructions for other drugs, in particular in the instructions for ceftriaxone, carbamazepine, methyldopa, etc.
Conclusion
In the Russian Federation, the situation currently remains unresolved and the problem is acute. Strict legal settlement of controversial situations is necessary in order to reduce unfounded cases of refusal to breastfeed, as well as legal protection for doctors who allow breastfeeding while taking prohibited medications. In controversial situations, the decision to breastfeed is made collectively, together with a clinical pharmacologist, and individually, weighing all the risks and benefits of both medications and breastfeeding.
Conflict of interest
. The authors declare no conflict of interest.
Literature
1. Davanzo R. Controversies in breastfeeding // Front. Pediatr. 2018. Vol. 1, N 6. R. 278.
2. Illamola SM, Bucci-Rechtweg C., Costantine MM, Tsilou E. et al. Inclusion of pregnant and breastfeeding women in research - efforts and initiatives // Br. J. Clin. Pharmacol. 2021. Vol. 84, N 2. R. 215-222.
3. Aydin B., Nayir T., Sahin S., Yildiz A. Olanzapine and quetiapine use during breastfeeding: Excretion into breast milk and safe breastfeeding strategy // J. Clin. Psychopharmacol. 2015. Vol. 35, N 2. R. 206-208.
4. Arguello B., Salgado TM, Fernandez-Llimos F. Assessing the information in the summaries of product characteristics for the use of medicines in pregnancy and lactation // Br. J. Clin. Pharmacol. 2015. Vol. 79. R. 537-544.
5. Drug safety
URL: https://grls.rosminzdrav.ru/Default.aspx
6. Order of the Ministry of Health of Russia dated May 10, 2017 No. 203n “On approval of criteria for assessing the quality of medical care.”
7. Rowe H., Baker T., Hale TW Maternal medication, drug use, and breastfeeding // Pediatr. Clin. North Am. 2013. Vol. 60. R. 275.
8. National Library of Medicine LactMed Database. (date of access September 2019)
URL: https://toxnet.nlm.nih.gov
9. URL: https://toxnet.nlm.nih.gov/help/newtoxnet/lactmedapp.htm
10. Hale T. Medications and Mothers' Milk. 14th ed. Amarillo, TX: Hale Publishing, 2010.
11. Kaplan YC, Keskin-Arslan E., Acar S. et al. Teicoplanin use during breastfeeding // Breastfeed. Med. 2021. Vol. 12. R. 124.
12. Fraissinet F., Lesourd M., Naudoux N. et al. Pharmacokinetics of teicoplanin in a breastfeeding mother // Breastfeed. Med. 2021. Vol. 12. R. 244-246.
13. Festini F., Ciuti R., Repetto T. et al. Safety of breast-feeding during an IV tobramycin course for infants of CF women // Pediatr. Pulmonol. Suppl. 2004. Vol. 27. R. 288-289.
14. Boda A. Gentamicin concentration in the milk of a mother after treatment by implants of a Septopal chain // Orv. Hetil. 1990. Vol. 131. R. 2263-2265.
15. Celiloglu M., Celiker S., Guven H. et al. Gentamicin excretion and uptake from breast milk by nursing infants // Obstet. Gynecol. 1994. Vol. 84. R. 263-265.
16. Cherif F., El Aidli S., Kastalli S. et al. Drug induced urticaria via breastfeeding // Fundam. Clin. Pharmacol. 2009. Vol. 23, suppl. 1. R 37.
17. Berens P, Eglash A, Malloy M et al. ABM Clinical Protocol No. 26: Persistent pain with breastfeeding // Breastfeed. Med. 2016. Vol. 11. R 46-53.
18. Manninen AK, Juhakoski A. Nifedipine concentrations in maternal and umbilical serum, amniotic fluid, breast milk and urine of mothers and offspring // Int. J. Clin. Pharm. Res. 1991. Vol. 11. R 231-236.
19. Duke ME, Britten FL, Pretorius CJ et al. Maternal metyrapone use during breastfeeding: Safe for the breastfed infant // J. Endocr. Soc. 2021. Vol. 3. R 973-978.
20. Ryu RJ, Easterling TR, Caritis SN et al. Prednisone pharmacokinetics during pregnancy and lactation // J. Clin. Pharmacol. 2021. Vol. 58. R 1223-1232.
21. Smuin DM, Seidenberg PH, Sirlin EA et al. Rare adverse events associated with corticosteroid injections: a case series and literature review // Curr. Sports Med. Rep. 2021. Vol. 15. R 171-176.
22. Davanzo R., Bua J., Paloni G., Facchina G. Breastfeeding and migraine drugs // Eur. J. Clin. Pharmacol. 2014. Vol. 70, N 11. R 13131324.
23. Anderson PO, Manoguerra AS, Valdes V. A review of adverse reactions in infants from medications in breastmilk // Clin. Pediatr. (Phila.). 2021. Vol. 55. R 236-244.
24. Constantinescu S., Pai A., Coscia LA et al. Breast-feeding after transplantation // Best Practice. Res. Clin. Obstet. Gynaecol. 2014. Vol. 28. R 1163-1173.
25. Flint J., Panchal S., Hurrell A. et al. BSR and BHPR guideline on prescribing drugs in pregnancy and breastfeeding - part I: standard and biological disease modifying anti-rheumatic drugs and corticosteroids // Rheumatology (Oxford). 2021. Vol. 55. R 1693-1697.
26. Gotestam Skorpen C., Hoeltzenbein M., Tincani A. et al. The EULAR points to consider for use of antirheumatic drugs before pregnancy, and during pregnancy and lactation // Ann. Rheum. Dis. 2016. Vol. 75. R 795810.
27. Brucker MC, King TL The 2015 US Food and Drug Administration Pregnancy and Lactation Labeling Rule // J. Midwifery Womens Health. 2021. Vol. 62, N 3. R. 308-316.
28. Crettenand M., Rossetti AO, Buclin T., Winterfeld U. Use of antiepileptic drugs during breastfeeding: what do we tell the mother? // Nerve-narzt. 2021. Vol. 89, N 8. R. 913-921.
Herbal treatment
One way to reduce high blood pressure is by consuming medicinal plants.
The calming properties of herbs give a good effect. They are observed when consuming a decoction from the entire list of herbs.
To prepare it, take:
- Juniper cones (2 tablespoons);
- lemon balm (2 tablespoons);
- fennel seeds (1 tbsp.);
- allspice (3 tablespoons);
- Peppermint (3 tablespoons).
Mix all ingredients in the quantities indicated above and pour 2 tablespoons of the mixture into a thermos. Pour boiled water (1 liter) over these herbs. Set aside for 3 hours, then strain. Drink 0.5 glasses twice a day - morning and evening half an hour before meals.
Feeding the child during this treatment cannot be stopped.
Therapeutic baths
Therapeutic baths are effective as one of the additional measures that help a nursing mother relax and reduce blood pressure.
They are available in 2 versions:
- With the addition of a solution of valerian or sea salt. Give a bottle of sedative or 1 tablespoon of salt in water. Treatment can be continued for up to 15 minutes.
- Clay baths. Add 3-4 handfuls of white clay to the water. Grind until completely dissolved and lumps disappear. Add chopped garlic (1 head). The session should last up to 30 minutes. After bathing, dry with a hard towel.
Diet
Nutrition during pregnancy should also be adjusted. A nursing woman should avoid excess salt, fried, fatty and smoked foods. You should also avoid hot and spicy spices and even sweets. Both the child and his mother are harmful.
Instead of junk food, eat more fruits and vegetables, fresh or minimally heated.
Nursing mothers should prohibit smoking and drinking alcohol. Coffee and tea have a negative effect on the health of women with hypertension; it is advisable to limit them. It is extremely important to maintain optimism and peace of mind.
Proper nutrition and prevention
To normalize blood pressure, it is important to adhere to proper nutrition.
A nursing mother should limit the consumption of fried, salty, fatty, smoked and spicy foods. She should also give up sweets and seafood. And also read on our website: In simple language about the treatment of hypertension in older people. Means of official and traditional medicine
Instead of tea, coffee and alcoholic drinks, it is better to give preference to freshly squeezed juices and water. For high blood pressure, fruits and vegetables are indicated, and minor heat treatment is allowed.
If there is a genetic predisposition to hypertension, you need to constantly measure your blood pressure using a special device. Regular physical activity will stabilize the functioning of the cardiovascular system. But it is important not only to take care of the body, but also to monitor your psychological state. You should be positive and avoid strong emotions.
Recovery should be smooth; things cannot be rushed. A young mother who finds herself at home is not recommended to be confined to a cramped lifestyle when, apart from the baby and the kitchen, she sees nothing else. The following are extremely useful for normalizing blood pressure:
- light jogging in the morning and evening;
- walking and cycling;
- swimming in a pond;
- daily exercise.
Muscular activity relieves the head, improves metabolism, and helps eliminate congestion in the body. During physical activity, hormones are produced that are responsible for a positive attitude. However, it is important to understand that sports only help if nothing bothers you.
Intense activity is contraindicated for a nursing mother with high blood pressure. Physical activity can be considered as a preventive measure, but during an exacerbation it is prohibited.
What to do if a nursing mother has low blood pressure
Having learned that high blood pressure is dangerous, it is necessary to deal with low blood pressure. Blood pressure below normal is also common, so the following recommendations will help normalize it:
- A woman should get plenty of rest. Her sleep should be 8 hours a day. You can avoid stress by taking herbal teas that contain sedatives.
- If low blood pressure occurs due to anemia, it is necessary to raise the hemoglobin level to normal using special medications.
- In case of hypotension associated with a lack of iodine in the body, it is obtained from iodized salt. In addition, many of them contain algae and fish.
If your blood pressure is low, a nursing woman should lie down for a while. When he gets better, he will need unsaturated sweet black tea with something nutritious.
Low pressure
A woman with hypotension gets tired quickly; due to emotional instability, she can flare up over anything. During this period, there is a high probability of falling into deep depression, which is an extremely undesirable condition during lactation. Breastfeeding is of great importance for the baby, who not only receives vital substances along with mother's milk, but is also charged with positive emotions and energy.
When a woman suffers from low blood pressure, one can hardly talk about a positive attitude. Taking care of a baby, keeping the house clean and cooking takes a lot of effort. It is necessary to raise blood pressure in such a way as not to harm the child and yourself. First you need to understand exactly how low blood pressure manifests itself.
The disease is diagnosed in cases where the upper level is less than 90 units. The indicator is average, it does not apply to those for whom 80 is the norm. When blood pressure rises in such people, it is no more than 70-120 mm Hg. Art. Such physiological features are usually noticeable even in childhood.
Hypotension in a young mother manifests itself with the following symptoms:
- high irritability;
- constant weakness and drowsiness;
- chronic fatigue;
- dizziness;
- tremor in the limbs;
- loss of appetite;
- numbness of fingertips;
- blueness under the eyes;
- short-term clouding of the mind;
- emotional depression and apathy for no reason;
- sudden weight loss.
Causes of low blood pressure
A condition in which blood pressure is low is called hypotension. In this condition, the upper limit falls below 90. In a woman with HD, many nutrients are transferred to the growth and development of the child. Therefore, iron deficiency anemia is considered one of the causes of hypotension.
Another deficiency of thyroid hormones is hypothyroidism.
There are also factors that contribute to lower blood pressure, such as postpartum depression, stress, and overwork.
Causes of hypotension
During the lactation period, blood pressure may decrease due to iron deficiency anemia, low blood clotting, thyroid insufficiency, and vegetative-vascular dystonia.
Having determined the true cause, you need to take measures to normalize the pressure. The lack of iron in the body of a nursing mother is due to an increased outflow of vitamins and minerals. Hemoglobin decreases and blood vessels lose their tone. An appropriate blood test must be done to confirm anemia.
Blood quickly passes through the veins and arteries, as a result of which its coagulability decreases. Thus, the organs do not receive enough nutrients. The greatest impact falls on the brain. Due to a lack of iodine in the body, hypothyroidism can develop; the disease is diagnosed after a special analysis.
Vegetative-vascular dystonia occurs due to impaired functioning of the central nervous system (due to past infectious diseases or frequent stress).
Having determined the cause of hypotension, measures must be taken to stabilize the pressure. To raise blood pressure, blood volume should be increased, which can be achieved by drinking plenty of fluids. It is worth focusing on green tea, ginseng, lemongrass, eleutherococcus, such drinks help well.
The drug Regidron perfectly stabilizes the water balance; a treatment course is often prescribed for prolonged recovery. Manual therapy allows you to get rid of physical and mental stress; massage helps to disperse blood and raise blood pressure. A visit to the sauna is also recommended, but certain restrictions must be observed.
Symptoms
You can recognize low blood pressure by the following symptoms:
- lack of breast milk;
- general weakness and drowsiness;
- weight loss;
- blue circles under the eyes:
- dizziness;
- apathy.
Low blood pressure can be recognized by these symptoms. This is a fairly dangerous condition and can lead to fainting if not handled correctly.
Low blood pressure during breastfeeding increases with drinking more fluids. During breastfeeding, a woman should consume more as it is necessary for milk production.
Other symptoms
As a rule, before the pressure increases, young mothers complain of migraines, dizziness, dark circles before the eyes, nausea and vomiting. During the diagnosis, an increase in the concentration of protein in the urine is detected, and the lower extremities swell. Often the pressure rises and falls.
If an increase in blood pressure is observed within 2-3 months, then, most likely, arterial hypertension of the first or second degree has developed. In this case, an urgent examination is required. The kidneys and urinary system as a whole must be checked. There is a high probability of seizures and accelerated development of heart failure.
Women who have experienced surges in blood pressure during lactation must be under medical supervision for at least 3 months. It is important to be able to reduce pressure in a timely manner and control its indicators, not allowing it to exceed 150/90 mmHg. Art. Due to swollen legs, the lungs may also suffer, but many medications are prohibited for use when breastfeeding. Violation of the prohibition can lead to the baby’s refusal to accept mother’s milk.
Consequences of high and low blood pressure during lactation
If we compare low and high blood pressure, the latter condition is much more dangerous because it can cause swelling of the mammary glands, that is, lactastasis. In this case, the woman’s reproductive health will suffer, in particular, refusal to breastfeed.
In addition, arterial hypertension can cause the following consequences:
- stroke or heart attack;
- atherosclerosis;
- complications of diabetes;
- cerebrovascular accident;
- heart failure.
Therefore, monitoring their well-being is the responsibility of every nursing woman, because we are talking not only about her health, but also about the well-being of the newborn.
Symptoms of pathology
Mastitis is characterized by increased body temperature, in contrast to lactostasis, in which the temperature rises in the diseased gland itself and in the surrounding area.
The general state of health worsens, pain in the chest is felt not only when touched, but also when moving, moving the arm, general weakness is noted, and the disease is often accompanied by a headache. After feeding or pumping, the temperature does not decrease.
There are uninfected mastitis, infected mastitis and breast abscess.
Symptoms of uninfected mastitis:
- your health worsens, the inflamed areas hurt, pain can be felt when walking or changing position;
- the temperature can be from 38 degrees and above.
Treatment: With effective breast emptying, the condition improves within 24 hours.
If there is no improvement, then most likely we are talking about infected mastitis:
- part of the chest becomes red and hot, painful when touched;
- the temperature is elevated and lasts for more than 2 days with effective emptying of the breast.
Treatment: you can use compresses, except alcohol (alcohol blocks the hormone oxytocin, which is responsible for the outflow of milk);
antibacterial drugs compatible with breastfeeding are prescribed. Infected mastitis can progress to the abscess stage:
- a cavity with purulent contents forms at the site of compaction;
- high temperature.
Self-diagnosis: to find out whether there is pus in the milk, you need to express the milk onto a cotton swab - the milk will be absorbed, but the pus will not. Treatment: surgical, systemic antibacterial drugs.
Prevention
There are simple and inexpensive preventive measures that can reduce the risk of hypertension in breastfeeding women:
- To do this, if the pressure has already risen many times, you need to monitor its values using a tonometer.
- Move more, breathe fresh air, be physically active.
- Avoid nicotine and alcohol.
- Eat a healthy diet.
- Maintain psychological balance.
Although the diagnosis of hypertension in nursing mothers is quite serious, you should not be afraid, because if you follow the recommendations of specialists, the prognosis is favorable. It is enough to monitor your health and, if necessary, undergo therapy.