Antiphospholipid syndrome (APS) is an autoimmune process of non-inflammatory origin.
During this process, immune cells produce antibodies aimed at destroying phospholipids - structural formations of vascular and nerve cells, as well as platelet membranes. Of particular danger are complications of antiphospholipid syndrome in pregnant women - stillbirth, premature birth, miscarriages, severe preeclampsia. To prevent this, even at the stage of preparation for pregnancy, the necessary diagnostics must be carried out, acquired or hereditary thrombophilia must be excluded through a blood test.
There are the following types of this pathology:
- catastrophic APS - thrombus formation in various organs in a short period of time (up to seven hours);
- primary – without manifestations of lupus erythematosus or concomitant infectious diseases;
- secondary – against the background of systemic lupus;
- syndrome without specific antibodies;
- APS, manifested by symptoms characteristic of other forms of thrombophilia.
Types of APS caused by the presence or absence of antiphospholipid antibodies:
- seropositive form - in addition to specific antibodies, a lupus anticoagulant was detected in the blood;
- seronegative form – absence of lupus anticoagulant, absence of antibodies to cardiolipin.
Diagnosis of antiphospholipid syndrome and its form is possible only in a modern laboratory equipped with highly sensitive technical equipment and high-quality reagents.
What is AFS?
APS is an autoimmune condition when antibodies to phospholipid complexes present in a variety of human organs begin to attack the tissues of their own body, because they perceive them as foreign and, as a result, try to resist an imaginary threat.
Despite the fact that theoretically any system can be affected, most often APS causes thrombosis (both arterial and venous), resulting in the development of such dangerous pathologies as thromboembolism, stroke and heart attack. In addition, the syndrome provokes serious complications during pregnancy.
It should be immediately noted that the production of antibodies to phospholipids itself cannot cause thrombosis. A certain event is necessary that will become a factor triggering the activation of the body’s immune forces. What could it be? For example, pregnancy, injury and stress.
Pathogenesis
The pathophysiological processes in the formation of antibodies to certain self-phospholipids have not yet been fully studied and are controversial. There are many theories trying to identify the mechanism/causes of coagulation disorders in APS - disruption of the mechanisms of cellular apoptosis , the production of antibodies against coagulation factors (proteins C and S, prothrombin, annexins), increased tropism of platelets to the vascular endothelium, etc. It also remains not fully understood the role of secondary risk factors in the development of APS (obesity, diabetes, hypertension, age, gender, etc.).
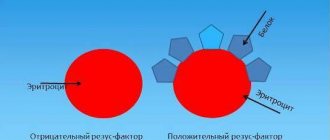
Antiphospholipid antibodies are represented by a large group of antibodies, but in practice, antibodies to cardiolipin (ACL)/lupus anticoagulant (LA) are of leading importance, which, when attached to platelets/endothelium of the vascular walls, enter into blood coagulation reactions, which leads to the development of thrombosis. There is also an assumption that antibodies have immune activity and can directly have a “toxic” effect on various tissues of the body.
It has been established that in order to trigger an autoimmune process, not only antibodies to phospholipids must be present in the body, but also cofactors, with which antibodies bind to form antigen-antibody complexes. Such cofactors include beta-2-glycoprotein-1, proteins C and S, prothrombin, etc., present in the serum of patients.
The process of producing antibodies to phospholipids is carried out due to endogenous/exogenous stimuli. The effect of exogenous stimuli (mainly infectious agents) is not an autoimmune process, is transient in nature and does not require treatment. And the production of antibodies when exposed to endogenous stimuli occurs with a violation of endothelial hemostasis . That is, the development of APS is based on various autoimmune reactions to phospholipid determinants, which causes coagulopathy of various localizations.
Phospholipids, being a universal component of mitochondria/cell membranes, are involved in the formation of the cytolemma of vascular endothelium, erythrocytes, platelets and nervous tissue cells. It is their wide representation in the human body that explains the extraordinary polymorphism/multisystem nature of the lesion, as well as the long-term persistent course and wide manifestations of APS symptoms.
Types of API
Antiphospholipid syndrome is divided into primary and secondary. The clinical manifestations of both forms are the same - thrombosis of various locations, miscarriage, obstetric complications (fetal growth restriction, preeclampsia, placental abruption). The only difference is the presence or absence of a background disease that could cause the appearance of APS.
- Primary antiphospholipid syndrome
Occurs in patients without concomitant autoimmune pathology, cancer, or infectious processes. In other words, there is no obvious reason for the production of antiphospholipid antibodies.
- Secondary antiphospholipid syndrome
“Lays on” the patient’s existing concomitant pathology:
- Secondary antiphospholipid syndrome against the background of autoimmune pathological conditions: rheumatoid arthritis, systemic lupus erythematosus, systemic scleroderma, ulcerative colitis, autoimmune thyroiditis, etc.
- Antiphospholipid syndrome occurring against the background of malignant pathology (carcinoma, thymoma, tumors of the lymphatic system).
- APS, which arose against the background of infectious and inflammatory processes, as well as infectious and immunological pathology (HIV, glomerulonephritis, bronchial asthma and others).
- APS that arose against the background of systemic pathologies, such as chronic renal or liver failure.
Criteria for antiphospholipid syndrome
To make a diagnosis of “Definite antiphospholipid syndrome”, at least one clinical and one laboratory criterion must be present simultaneously:
1. Clinical criteria:
- Thrombosis of any location. This may be venous thrombosis (affecting the veins of the lower or upper extremities, thrombosis of the venous sinuses of the brain); arterial thrombosis (in the vessels of the extremities, the arteries of the heart - myocardial infarction, the arteries of the brain - ischemic stroke, the vessels of the abdominal cavity - mesenteric thrombosis, thrombosis of the renal arteries, etc.), thrombosis of the retinal vessels, as well as thrombotic lesions of the microvascular bed - for example, subcutaneous diffuse thrombosis, which manifests itself as a reticular pattern on the skin (livedo reticularis).
- 3 or more consecutive losses of a morphologically normal fetus before 10 weeks of gestation. If a chromosomal pathology is detected in a dead fetus, such a case of pregnancy loss is not taken into account as a criterion for APS.
- At least one loss of a morphologically normal fetus during pregnancy more than 10 weeks (antenatal death, late miscarriage).
- Premature birth before 34 weeks of pregnancy due to placental abruption, severe preeclampsia, placental insufficiency.
2. Laboratory criteria:
- positive blood test for lupus anticoagulant,
- antibodies to cardiolipin IgG and/or IgM, determined by ELISA, in a titer of 40 U/ml and above (with the laboratory norm not exceeding 20 U/l),
- antibodies to beta-2-glycoprotein IgG and/or IgM, determined by ELISA, in a titer of 40 U/ml (with the laboratory norm not exceeding 20 U/ml)
Important
: The laboratory criterion is considered met if positive antibodies are detected at least twice with an interval of at least 12 weeks between tests, but not more than 5 years.
In addition, the diagnosis of APS is not considered confirmed if more than 5 years have passed between clinical manifestations (thrombosis or pregnancy loss) and a positive laboratory test.
Probable antiphospholipid syndrome
If the patient has antiphospholipid antibodies, but collectively the criteria for definite APS are not met, a diagnosis of “probable APS” can be formulated. This happens, for example, with one or two fetal losses for up to 10 weeks and the presence of antiphospholipid antibodies; in case of inconsistent fetal losses (miscarriage, then childbirth, then two more miscarriages), or if, for example, the pregnancy was complicated by preeclampsia or placental abruption, but the birth occurred later than 34 weeks, and so on.
Also, the diagnosis of “probable APS” can be established when laboratory criteria are not fully met: the antibody titer does not reach the required 40 U/ml, or positive antibody tests are performed at intervals of less than 12 weeks, and so on.
Treatment
Treatment of antiphospholipid syndrome consists of prescribing anticoagulant and antiplatelet therapy. APS is treated by a rheumatologist and a hematologist; in pregnant women, by an obstetrician-gynecologist together with a hematologist.
Bibliography:
- Federal clinical guidelines for the treatment of APS, 2013
- “Antiphospholipid syndrome” Makarenko E.V. Health and environmental issues, 2021
- “Antiphospholipid syndrome in obstetric practice” Goncharova A.A., Kravchenko E.N., Krivchik G.V., Votrina I.R., Chebakova V.Yu. Mother and child in Kuzbass, 2021
- “Antiphospholipid syndrome in surgical practice” Altukhov I.A., Lyubarsky M.S., Nimaev V.V. Medicine in Kuzbass, 2014
- “Antiphospholipid syndrome in the fibrinolysis system” Ostryakova E.V., Patrushev I.L., Reshetnyak T.M. Scientific and practical rheumatology, 2011
- “The role of b-2-glycoprotein I in the pathogenesis of antiphospholipid syndrome” Kobilyanskaya V.A. Kazan Medical Journal, 2008
Symptoms of antiphospholipid symptom
The doctor may be concerned about episodes in the patient’s past, such as:
- frozen pregnancies for a period of 10 weeks or more (even one such case is a reason for examination for the presence of APS);
- premature birth before 34 weeks, if severe forms of preeclampsia or fetoplacental insufficiency were detected during pregnancy;
- miscarriages (3 or more) in the early stages (up to 10 weeks), if the reasons for this could not be found;
- hypoxia (a condition caused by insufficient oxygen supply) and delayed fetal development;
- premature detachment of a normally located placenta.
Also at risk are women who have previously developed venous or arterial thrombosis during pregnancy, while taking oral contraceptives, or after giving birth.
Diet
There is no special diet. However, with increased cholesterol and the risk of cardiovascular diseases and blood clots, patients should limit animal fats, carbohydrates, and salt. When treated with Warfarin, the diet should not contain an increased amount of vitamin K , which contains leafy vegetables, green tea, white cabbage, cauliflower, Brussels sprouts, broccoli, wheat bran, pumpkin, avocado, dairy products, spinach, carrots, currants.
APS during pregnancy
To prevent the development of dangerous complications, the doctor prescribes treatment from the very beginning of pregnancy.
If there are appropriate indications, the specialist may prescribe anticoagulants (drugs that reduce blood viscosity) and antiplatelet agents (substances that prevent red blood cells and platelets from sticking together).
Additionally, it is recommended to take B vitamins (including folic acid) and magnesium.
If a pregnant woman suffers from APS, she develops progesterone deficiency, so from the very beginning of pregnancy the doctor prescribes progesterone drugs.
Pregnancy management should be carried out under the supervision of an experienced hemostasiologist. Careful monitoring of the condition of the expectant mother and baby is necessary, as well as adjustment of the dosage of drugs based on research results. In the absence of adequate treatment, the likelihood of a successful pregnancy outcome is very low. If therapy is started in a timely manner, the chances increase markedly.
Classification of the disease
The following forms of APS are distinguished, which differ in etiological factors and clinical course:
- Primary. The formation of the syndrome is not associated with background pathology that can provoke the growth of antibodies to phospholipids.
- Secondary. Develops against the background of some other autoimmune disease, complicating its course. The development can be transient and, with adequate therapy, reversible (for example, with oncology, long-term drug therapy, viral diseases, etc.)
- Catastrophic. Rapidly increasing coagulopathy, leading to generalization of thrombosis of the vascular structures of internal organs, multiple organ failure. Difficult to stop even in intensive care, fetal mortality reaches 95%.
- Seronegative. It is characterized by the presence of a typical clinical picture and the absence of laboratory criteria for the syndrome. Sometimes the symptoms are extremely mild.
APS can also be caused by other microangiopathic syndromes (lupus, hemolytic-uremic syndrome).
APS during pregnancy
Antiphospholipid syndrome during pregnancy requires regular monitoring of women on an outpatient or hospital basis. APS in most cases has tragic consequences not only for the fetus (sometimes a newborn), but also for the woman. The effect of APS on pregnancy is due to the activation of the following pathological mechanisms:
- the formation of blood clots in arteries and veins;
- development of severe inflammatory diseases;
- cell death;
- negative impact on the embryonic layer, which provides the developing fetus with nutrition from the mother throughout the gestation period.
Antiphospholipid antibodies disrupt the implantation process and the properties of embryonic cellular structures. In this regard, the depth of penetration of trophoblast (embryo cells) into the endometrium of the uterus is reduced, creating the prerequisites for the formation of a thrombus formation process.
Antibodies in APS syndrome can themselves cause low levels of the pregnancy hormone, which causes miscarriage or frozen pregnancy. Due to the launch of pathogenic mechanisms, complications such as intrauterine growth retardation and fetal death in a later gestational period, gestosis and preeclampsia, and fetal loss syndrome are observed.
Clinical manifestations and complications
APS syndrome can be suspected based on clinical and laboratory studies if it is impossible to conceive or spontaneous termination of pregnancy when it occurs. Women complain of pain in the pelvic organs of unknown origin, malaise, and pronounced venous-vascular pattern of the lower extremities.
Considering the various theories of the development of autoimmune pathology, the symptoms are also diverse. Despite this, antiphospholipid syndrome complicates the onset and course of pregnancy and threatens the life and health of the woman and the fetus. The following complications are identified:
- For pregnant. Preeclampsia - up to 22%, premature placental abruption in 10-15% of cases, thrombocytopenia, cardiovascular complications, arterial hypertension, catastrophic course of APS with a fatal outcome.
- For the fruit. Miscarriage in most cases of pregnancy, premature delivery, intrauterine death or profound developmental delay, fetal thrombosis in the fetus, frozen pregnancy.
- For newborns. Thrombosis in 85% of cases, asymptomatic increase in the level of antibodies to phospholipids. Most of these complications are associated with autism.
Women with APS syndrome are advised to carefully plan their pregnancy, lifelong maintenance drug therapy with dose adjustment during preparation and throughout gestation, and continue the course of treatment after childbirth.
Preparing for pregnancy
The main goal of preparatory measures is to create favorable conditions for embryo implantation, reducing the risks of miscarriage, intrauterine pathologies and fetal death. During preparation, blood clotting ability, the level of antiphospholipid antibodies and lupus anticoagulant are assessed. Be sure to eliminate infections if they exist.
Treatment regimen for antiphospholipid syndrome during pregnancy at the preparatory stage:
- low molecular weight heparin;
- hirudotherapy;
- antiplatelet agents;
- progesterone vaginally;
- Magne B6 injection or oral solution;
- Omega 3 fatty acids.
The dosage of heparin and antiplatelet agents is adjusted until blood test values stabilize.
Pregnancy management tactics
The use of heparin and aspirin-containing drugs is continued, the dosage is adjusted based on laboratory data. The course of treatment is supplemented with prophylactic doses of immunoglobulins. The patient needs to take vitamin D and calcium supplements to prevent the development of osteoporosis.
Aspirin is stopped at 36-37 weeks of pregnancy, low molecular weight heparin is continued until full term, but there are also individual treatment regimens. If a caesarean section is necessary, heparin should be stopped 24 hours before delivery. If a woman took heparin-containing drugs until childbirth, then epidural anesthesia is unacceptable.
After delivery
After birth, the treatment regimen prescribed during pregnancy is continued for 2-3 months. Taking medications is resumed 5-10 hours after birth if there is no bleeding. Women are prescribed a protective regimen, but it is recommended to get up earlier, move more, and wear compression stockings to prevent thrombosis.
With timely diagnosis and preventive therapy, the prognosis for life with APS in women, including during pregnancy, is favorable. Among the factors that worsen the prognosis are the course of antiphospholipid syndrome with systemic lupus erythematosus, persistent hypertension, and thrombocytopenia.
In our International Hemostasis Clinic, located in Moscow, you will find experienced specialists, some of the world's leading experts on this problem, who will help you understand the causes of your disease and prescribe competent treatment for the syndrome. Make an appointment using the online form on the website or by calling.
Antiphospholipid antibodies in the blood - normal or pathological?
Sometimes the level of antiphospholipid antibodies can be elevated in a healthy person. In 12% of people, these antibodies are present in the blood, but they do not develop the disease. The older the person, the higher the levels of pathological immunoglobulins may be. There is also a possibility of a false-positive Wasserman reaction, for which the patient should be prepared. The main thing is not to panic and undergo a comprehensive diagnosis.
Video: APS and other thrombophilias in obstetrics:
Author of the article:
Volkov Dmitry Sergeevich |
Ph.D. surgeon, phlebologist Education: Moscow State Medical and Dental University (1996). In 2003, he received a diploma from the educational and scientific medical center for the administration of the President of the Russian Federation. Our authors
Why us?
- Ultra-modern equipment. The qualifications of our specialists, expert equipment and modern techniques allow us to timely and accurately diagnose APS.
- Consultation of related specialists. The patient is examined by a council of doctors, this especially applies to pregnant women.
- Comfortable conditions. Our rheumatologists devote maximum time to each client. All services are provided in one building in the center of Moscow, which saves effort and time.
- Innovation. The use of high-tech treatment methods ensures the success of therapy.
Use the full potential of modern medicine to maintain your own health and give life to your child - contact a rheumatologist at the Yauza Clinical Hospital.
You can see prices for services
Diagnosis of antiphospholipid syndrome in pregnancy
If a woman has had 2 or more miscarriages, it is recommended to undergo testing for APS before planning a pregnancy. During pregnancy, diagnosis of APS syndrome includes:
- Assessment of symptoms – swelling, ulcers, high blood pressure;
- History of other diseases, genetic diseases in the family, whether other family members had APS, as well as heart attacks, strokes before the age of 40;
- Obstetric history - history of previous pregnancies, miscarriages, premature births;
- Complete blood count to evaluate red blood cells, platelets, white blood cells;
- Doppler - study of blood flow in vessels;
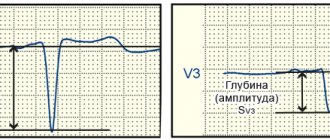
- Coagulogram is an assessment of blood clotting ability. Assessment of indicators that are responsible for stopping bleeding, the formation of blood clots, assessment of D-dimer - a product of the breakdown of blood clots;
- Enzyme immunoassay, indirect Coombs test, lupus anticoagulant test - determination of antibodies;
- Cardiotocography – assessment of the condition of the fetus, its motor activity, heart rate, hypoxia;
- Ultrasound fetometry and other studies when indicated.
Forecast
The course of this disease and the severity of thrombotic complications cannot be predicted. Unfavorable in terms of mortality are arterial thrombosis , recurrent thrombosis and thrombocytopenia . The prognosis still depends on how timely treatment is started, which the patient must strictly follow (sometimes for life). Mortality is associated with the development of stroke , heart attack , pulmonary hypertension , endocarditis , nephropathy , pulmonary embolism , and gangrene of the extremities .
If we consider catastrophic APS, the prognosis is unfavorable. Death occurs in half of patients and is caused by heart failure , myocardial infarction , respiratory distress syndrome and pulmonary failure . In the presence of antiphospholipid syndrome in patients with lupus erythematosus, the prognosis is also not favorable, since the survival rate of such patients is reduced.
What body systems are affected by APS, symptoms of disorders
Antiphospholipid syndrome is associated with a risk of developing various diseases. Moreover, any organs and systems can be affected, even the brain. If its vessels are damaged, a transient ischemic attack or heart attack may develop.
This is accompanied by symptoms such as:
- The appearance of seizures.
- Dementia that is constantly progressing.
- Mental disorders.
APS can also manifest itself with the following neurological symptoms:
- Severe headaches of the migraine type.
- Uncontrollable trembling of the limbs.
- Symptoms characteristic of transverse myelitis. They occur because in APS the spinal cord is affected.
The most serious complication of heart damage is a heart attack. It develops when blood clots form in the coronary arteries. If their small branches are involved, then the heart attack will be preceded by disturbances in heart contraction. APS can also lead to the development of heart defects and the formation of an intracardiac thrombus. Such indirect signs of antiphospholipid syndrome can make it difficult to diagnose the cause of the disease.
Symptoms of APS, depending on which organ is affected by thrombosis, will be as follows:
- An increase in blood pressure is observed with thrombosis of the renal arteries.
- When a pulmonary artery is blocked by a blood clot, pulmonary embolism develops, which leads to a sharp deterioration in a person’s well-being. Sometimes the death of a patient can occur instantly.
- Bleeding in the gastrointestinal tract.
- Splenic infarction.
- The appearance of subcutaneous hemorrhages, skin necrosis, ulcers on the legs - all these symptoms develop when the dermis is damaged.
The AFS clinic is diverse. It is impossible to describe the exact symptoms, since any organs and systems can be involved in the pathological process.
Prevention
Prevention includes:
- Control of the disease against which APS develops.
- Timely treatment of infectious complications.
- Impact on risk factors for thrombosis (high cholesterol, hypertension).
- Preparing women suffering from APS before pregnancy. This preparation includes the following treatment measures over 3 months: several sessions of plasmapheresis, taking antiplatelet agents (aspirin) for increased platelet function. If a woman receives warfarin, she is switched to low molecular weight heparins. In women, concomitant diseases are identified and treated, and foci of infection are sanitized. A woman should take vitamins with folic acid (0.8-1 mg per day), and if hyperhomocysteinemia is detected, the dose is increased to 5-6 mg. Taking vitamins B6, B1, B12 is also indicated. If the luteal phase is insufficient, progesterone .
- Women with recurrent miscarriage undergo HLA typing and karyotyping to identify various forms of thrombophilia.