Hemorrhagic strokes and hemorrhagic disease of the newborn
Few people know that stroke occurs not only in adults. Among the fund's wards are children, including those who are struggling with the consequences of perinatal stroke. We asked a pediatric hematologist from the National Medical Research Center for Pediatric Orthopedics. D. Rogacheva Fedorova Daria Viktorovna to tell about childhood strokes, why they happen and how to recognize the symptoms of a stroke in an infant.
Pediatric hematologist NMRC DGOI named after. D. Rogacheva Fedorova Daria Viktorovna
Strokes in newborns, as in older age groups, are the result of blockage of a blood vessel in the brain by a thrombus or rupture of such a vessel. Both of these causes cause damage to the brain substance surrounding the vessel. In medical terms, perinatal stroke is an acute cerebral circulatory disorder with chronic consequences that developed during the period from the 20th week of intrauterine development to the 28th day of the child’s life. In newborn children, hemorrhagic strokes (hemorrhages) occur approximately 3-4 times less often than ischemic strokes (that is, caused by thrombosis). Intracranial hemorrhage can be primary, or it can develop secondarily after an episode of thrombosis (the so-called hemorrhagic impregnation of ischemic foci). Perinatal stroke often causes chronic neurological deficits.
Clinical manifestations of stroke in a newborn child may include lack of response to external stimuli, episodes of convulsions, disturbances in muscle tone, weakness in the limbs, apnea (breathing problems), and breast refusal.
Evaluation of a child with suspected stroke includes examination by a neurologist and pediatrician, imaging of the brain (computed tomography or, preferably, magnetic resonance imaging, as well as ultrasound neurosonography to detect hemorrhages in the ventricles of the brain), as well as laboratory tests aimed at identifying the cause of the incident (in particular, blood clotting disorders). If the first clinical manifestation in a child is seizures, an examination aimed at excluding possible causes other than stroke (infections, electrolyte disturbances, inborn errors of metabolism), as well as EEG monitoring, is also necessary.
Premature babies (especially those born before the 28th week of gestation) are characterized by hemorrhages in the ventricles of the brain, associated primarily with the anatomical and physiological characteristics of a very premature baby. At the same time, in most cases (up to 75%) of hemorrhagic strokes in full-term newborns, the cause of the primary intracranial hemorrhage cannot be determined. Only a small part of them is a clear consequence of blood coagulation disorders (thrombocytopenia, hemophilia, hemorrhagic disease of the newborn, etc.) or cerebral vascular abnormalities (cavernous and arteriovenous malformations or aneurysms).
A high risk of intracranial hemorrhage (up to 25%) is associated with such a rare disease as neonatal alloimmune thrombocytopenia (NAIT). In this disease, the mother’s body produces antibodies to the fetal platelets. Passing through the placenta, antibodies destroy fetal platelets, causing deep thrombocytopenia in the baby before birth, while the mother's platelet count remains normal. Up to half of all intracranial hemorrhages during NAIT occur in utero. Intracranial hemorrhages occur much less frequently in newborns with hereditary coagulation disorders. In severe hemophilia, intracranial hemorrhage becomes the first manifestation of pathological bleeding in 2-3% of cases.
Another important and, most importantly, potentially preventable risk factor for intracranial hemorrhage in newborns is vitamin K deficiency.
Newborns are at risk for the development of vitamin K because their functionally immature liver cannot yet effectively utilize vitamin K. In addition, vitamin K does not pass well through the placenta, which leads to a lack of its reserves in the child’s body at the time of birth. A child in the first months of life receives little vitamin K from food (this is especially true for children who are exclusively breastfed, since breast milk contains less vitamin K compared to adapted milk formulas). In older children and adults, a significant proportion of vitamin K is formed by bacteria living in the intestines, however, the microflora of a newborn child is in its infancy and cannot yet compensate for the deficiency of vitamin K. Normally, the concentration of vitamin K in the blood reaches “adult” values by the age of 1 month .
Severe deficiency of vitamin K can lead to the development of the so-called hemorrhagic disease of newborns (a more modern name is vitamin K deficient bleeding (VKDB)). The risk of developing hemorrhagic disease of the newborn increases in babies whose mothers took certain antibiotics (for example, cephalosporins), anticonvulsants, and coumarin anticoagulants (for example, warfarin) during pregnancy.
Clinical manifestations of hemorrhagic disease of newborns include the appearance of bruises, bleeding from the mucous membranes and from the umbilical cord, regurgitation streaked with blood or blood in the stool, and intracranial hemorrhages.
There are three forms of hemorrhagic disease of newborns:
- Early (develops in the first 24 hours of a child’s life and is usually associated with the mother taking drugs that block the metabolism of vitamin K, for example, some anticonvulsants, the risk of intracranial hemorrhage is up to 25%,
- Classic (develops between 2 and 7 days of life and in most cases can be prevented by prophylactic administration of vitamin K at birth),
- Late (in fact, it no longer refers to the neonatal period and develops between 2 weeks and 6-8 months of life, risk factors are pathology of the gastrointestinal tract that impairs the absorption of fats, pure breastfeeding and refusal of prophylactic administration of vitamin K in the maternity hospital), according to According to some data, the risk of developing intracranial hemorrhage reaches 50%.
Vitamin K deficiency bleeding should be included in the differential diagnosis in all cases of increased bleeding and, especially, intracranial hemorrhage in children in the first six months of life, especially those who are exclusively breastfed and who have not received vitamin K prophylaxis in the maternity hospital.
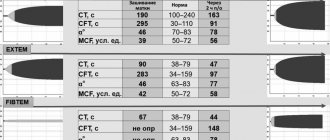
The diagnosis of vitamin K-dependent bleeding can be confirmed by studying the coagulogram (extension of prothrombin and activated partial thromboplastin time with normal fibrinogen concentration and normal platelet count). Treatment is immediate administration of vitamin K; if bleeding is severe, a transfusion of fresh frozen plasma may be required.
Hemorrhagic disease of the newborn is a well-known risk factor for intracranial hemorrhage and other severe bleeding. Therefore, in recent decades, prophylactic intramuscular administration of vitamin K to newborns on the first day of life has been a common practice. According to the recommendation of the Russian Society of Neonatologists, a vitamin K preparation (Vikasol) should be administered to all newborns in the first hours after birth once intramuscularly at a dose of 1 mg/kg (0.1 ml/kg). Similar recommendations (intramuscular administration of vitamin K to all newborns) exist in the USA, Canada, European Union countries, Israel, Australia, and Japan.
If the patient does not have congenital disorders of vitamin K metabolism, which are extremely rare, and severe pathology of the gastrointestinal tract, which impedes adequate absorption of fats and fat-soluble vitamins, after treatment, vitamin K-dependent bleeding does not recur at an older age and does not require regular monitoring coagulograms. A history of hemorrhagic disease of a newborn is in no way a contraindication to rehabilitation measures aimed at correcting the existing neurological deficit.
Intracranial hemorrhages caused by vitamin K deficiency can lead to profound disability and even death. The administration of vitamin K is not a vaccination; there are practically no absolute contraindications for its administration in the maternity hospital. Therefore, even if for some reason you refuse to vaccinate your baby in the maternity hospital, do not refuse to administer vitamin K. This simple manipulation can significantly reduce the risk of very serious complications.
Support the work of the foundation with a donation.
Help us fight stroke! Share
Clinical characteristics of hemorrhagic syndrome
| I. Hematoma type (disturbance of the internal coagulation pathway of coagulation hemostasis) | II. Petechial-spotted (microcirculatory) type (disturbance of the platelet link of hemostasis, external coagulation pathway of coagulation hemostasis) | III. Mixed (bruise-hematoma) type (combined disorder of both platelet and coagulation components of hemostasis) | IV.Vasculitic purpuric type (pathology of the microvascular bed) | V.Angiomatous type (local vascular pathology) |
Types of hemorrhagic syndrome
Violation of the internal coagulation pathway of coagulation hemostasis (hematoma type of bleeding)
Congenital and acquired afibrinogenemia
Deficiencies of different types of clotting factors cause different types of diseases called hemophilia, as well as other disorders that are not specific to a specific type.
More details
Disturbance of the platelet component of hemostasis, the external coagulation pathway of coagulation hemostasis (petechial-spotted type of bleeding)
Disturbance of the platelet component of hemostasis:
Disturbance of the plasma component of hemostasis
Thrombocytopenia
A condition characterized by a decrease in platelet count below 150•109/l, which is accompanied by increased bleeding and problems with stopping bleeding.
More details
Thrombocytopathy
A disease characterized by increased bleeding due to dysfunction of platelets (blood platelets that provide the initial stage of blood clotting) when their number is normal.
More details
Deficiency of factors II,V,VII,XI
Diseases associated with impaired coagulation; in these diseases, hemorrhages occur in the joints, muscles and internal organs, both spontaneously and as a result of injury or surgery.
More details
Combined violation of the platelet and coagulation components of hemostasis (mixed (bruise-hematoma) type of bleeding)
Etiology:
- Von Willebrand's disease (coagulopathy - impaired function of factor VIII, thrombocytopathy - impaired platelet aggregation)
- DIC syndrome (consumptive coagulopathy - decrease in all coagulation factors, hypofibrinogenemia, activation and depletion of fibrinolysis, thrombocytopenia, consumption thrombocytopathy)
Hemorrhagic syndrome:
- Petechial rash, ecchymosis, bleeding from the mucous membranes (nasal, gingival), postoperative, postpartum bleeding.
Disseminated intravascular coagulation
Impaired blood clotting due to massive release of thromboplastic substances from tissues.
More details
von Willebrand disease
A hereditary blood disease characterized by the occurrence of episodic spontaneous bleeding, which is similar to bleeding in hemophilia.
More details
Pathology of the microvascular bed (vasculitis-purple type of bleeding)
Petechial bleeding with exudative-inflammatory phenomena, foci of necrosis, hematuria, arthralgia, bleeding of mucous membranes.
Vasculitis:
- infectious, immune;
- systemic;
- hemorrhagic vasculitis (Schonlein-Henoch disease).
Hemorrhagic vasculitis
Systemic aseptic inflammation of the microvasculature with predominant damage to the skin, joints, gastrointestinal tract and renal glomeruli.
More details
Angiomatous bleeding
Angiomatous bleeding
One of the forms of hereditary vascular disease, characterized by a tendency to bleeding of the mucous membranes.
More details
Symptoms of hemorrhagic syndrome
The nature and localization of skin rashes during hemorrhagic syndrome determine the symptoms of this pathology.
The main symptom is prolonged bleeding that occurs as a result of injury or exhausting physical activity, severe overexertion, hypothermia or overheating, which can also occur spontaneously.
In every fifth case of the pathology, a rash of a different nature is observed, both small petechiae and large necrotic hematomas may appear, and angiectasias may occur.
Hemorrhagic syndrome can result from taking medications that affect the natural processes of platelets and reduce blood clotting. In addition, patients suffering from Werlhof's disease, hemophilia and prothrombin deficiency may also experience this pathology.