The Laboratory of the Blood Clinic performs a study of the activity of von Willebrand factor using a high-precision method using a modern aggregometer.
The analysis period is up to 30 days, not counting the day of collection.
List price is 3000 rubles.
Detailed description of the study
Von Willebrand factor (VWF) is a large protein that is a blood clotting factor and is involved in stopping bleeding. It ensures the formation of a clot of platelets at the site of vessel damage and protects factor VIII, an antihemophilic plasma protein, from destruction.
The hemostatic system is a combination of mechanisms that are responsible for stopping bleeding when a vessel is damaged. First, a primary clot is formed due to the action of platelets and the walls of the vessel itself. Next, plasma proteins participate in the formation of a dense blood clot, which finally eliminates the defect. Von Willebrand factor, unlike other clotting factors, is directly involved in the formation of a blood clot.
Von Willebrand factor is synthesized in the bone marrow. In addition, it is produced by cells lining the inner surface of blood vessels (endothelium). The protein is able to bind to factor VIII, and if a vessel is damaged, it delivers it to the site of vessel damage for effective blood clotting. Also, von Willebrand factor binds to a protein on the surface of platelets, which activates their gluing to each other (adhesion). Another of its functions is the attachment of platelets to collagen, which is released when the integrity of the vascular wall is violated. All of these processes ultimately lead to successful stopping of bleeding and restoration of the integrity of the blood vessel.
A defect in the gene that responds to the production of von Willebrand factor leads to the development of hereditary coagulopathy - von Willebrand disease. There are three types of the disease. The first type is the most common. At the same time, the amount of VWF in the blood is moderately reduced and functions are not impaired. The second type is when the functional activity of VWF is impaired, even with sufficient levels in the blood. The third type is severe, observed quite rarely, the amount of EF is sharply reduced.
Clinically, the disease manifests itself as prolonged bleeding of various locations: from the nose, gums, gastrointestinal tract, uterus. The disease is characterized by the appearance of bruises that do not correspond to the size of the injury. Bleeding is also observed after small cuts that do not stop for a long time; bleeding time increases after operations and dental procedures, such as tooth extraction.
In severe forms of von Willebrand disease (often type 3), symptoms similar to hemophilia may occur due to factor VIII deficiency. Muscle hematomas and hemarthrosis appear - hemorrhages into the joint cavity. The consequences of the disease are cerebral hemorrhages, bleeding from internal organs, decreased hemoglobin in the blood (anemia).
Determining the amount of von Willebrand factor in the blood is necessary to assess the state of the coagulation system and timely diagnosis of von Willebrand disease, which leads to bleeding.
Symptoms
The symptoms of von Willebrand disease are extremely diverse: from minor episodic bleeding to massive, debilitating bleeding, leading to severe blood loss.
Signs characteristic of von Willebrand disease:
- severe, prolonged or spontaneously renewing bleeding after minor surgical interventions, tooth extraction;
- subcutaneous hematomas that appear after minor traumatic impacts or spontaneously
- bleeding for more than 15 minutes after minor injuries or spontaneously recurrent bleeding 7 days or more after injury;
- hemorrhagic skin rash;
- severe anemia;
- intense, prolonged menstruation;
- spontaneous nosebleeds lasting more than 10 minutes or requiring medical intervention due to the intensity;
- blood in feces in the absence of gastrointestinal pathology that can provoke the development of gastrointestinal bleeding.
More often, increased bleeding is observed in childhood, decreasing as they grow older, and subsequently there is an alternation of exacerbations and remissions.
References
- Zozulya, N.I., Kumskova, M.A., Likhacheva, E.A. and others. Clinical guidelines for the diagnosis and treatment of von Willebrand disease. — Congress of Hematologists of Russia, 2021. — 30 p.
- Chernova E.V. von Willebrand factor. — Bulletin of the North-Western State Medical University named after. I.I. Mechnikova, 2018. - T. 10. - No. 4. - P. 73–80.
- Chubukov, Zh.A. Von Willerbrand factor and endothelial dysfunction under stress. - Problems of health and ecology, 2012. - pp. 40-44.
- Pathophysiology: textbook: in 2 volumes / ed. V.V. Novitsky, E.D. Goldberg, O.I. Urazova. — 4th ed., revised. and additional - GEOTAR-Media, 2009. - T. 2. - 640 p.
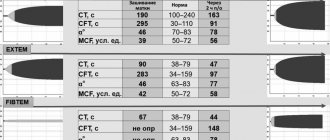
Diagnostics
Diagnosis of von Willebrand disease requires the indispensable participation of hematologists. It is impossible to make a diagnosis at the level of a clinic or children's consultation due to the lack of capabilities of the laboratories of these institutions to conduct specific diagnostic tests and enzyme-linked immunosorbent technologies. The doctor assumes the disease when interviewing relatives, examining the patient and taking into account information from the anamnesis.
Moreover, available tests vary in sensitivity and diagnostic value. Therefore, an algorithm for examining the suspected patient has been developed.
- First, a coagulogram is studied with all indicators of coagulation, including bleeding time. The test can be done at your clinic. If pathological abnormalities are detected, the patient is referred to the hematology center.
- To identify a specific type of disease and the qualitative side of the defect, a comparison of the impaired aggregation ability under the influence of ristocetin with the normal one is used - under the influence of collagen, thrombin, ADP, and adrenaline.
- The main method of detecting a decrease in the amount of factor VIII in the blood is to determine the activity of the patient’s platelets treated with formaldehyde in reaction with a solution of ristocetin.
- Using the collagen-binding technique, the impaired functional ability of factor VIII and the specific type of disease are identified.
In the diagnosis of concomitant lesions of the mucous membranes it is necessary:
- examination by an otolaryngologist;
- esophagogastroduodenoscopic examination;
- colonoscopy (examination of the intestines).
For treatment, it is important to identify vascular formations in the form of tortuosity, angiomas, extensions up to 2 mm, which contribute to bleeding.
What may indicate the presence of a negative process?
Many doctors point to the following von Willebrand symptoms:
- Bruising in the gum areas;
- The appearance of blue bruises for no apparent reason;
- Regular bleeding from the sinuses;
- Loss of large amounts of blood during menstruation;
- Severe hemorrhages in women during menopause;
- The problem is stopping the bleeding after surgery or due to injury;
- Presence of red cells in urine and feces;
- The same process takes place inside the joints and muscles, causing severe pain, swelling and difficulty moving.
Treatment of von Willebrand disease
Von Willebrand disease is treated by a hematologist. You should be prepared in advance for the fact that it will not be possible to achieve a full recovery, since gene abnormalities cause the pathology. However, it is quite possible to improve the quality of life of patients.
Treatment is based on replacement transfusion therapy, which allows normalizing the functioning of all stages of hemostasis. Patients are prescribed hemotherapy containing von Willebrand factor. This may be cryoprecipitate or antihemophilic plasma. This treatment makes it possible to increase the production of factor VIII in the patient’s body.
- If a person develops minor bleeding, you can try to stop it using a tourniquet and a hemostatic sponge. Treatment of the wound with thrombin also effectively prevents blood loss.
- To stop bleeding, the patient may be prescribed drugs such as: antifibrinolytics, hormonal oral contraceptives, Desmopressin.
- Fibrin gel can be applied to a wound surface that is bleeding.
- A plaster splint is applied to the limb with the affected joint (if hemarthrosis develops). It is imperative to give the joint an elevated position. When the hemorrhage is stopped, the patient is prescribed UHF. The affected joint should be limited in loads. If the patient’s condition is severe, he is prescribed a puncture with blood pumping.
Desmopressin is a drug prescribed to treat von Willebrand disease types 1 and 2. Taking this medication stimulates the body to produce factor VIII. The drug can be used both in the form of a nasal spray and in the form of injections. If therapy does not bring the desired success, then the patient is prescribed a transfusion of plasma concentrate of the missing factor.
Tranexamic acid and aminocaproic acid are antifibrinolytic drugs. They are administered intravenously or taken orally. These drugs are prescribed for recurrent uterine bleeding, nosebleeds and gastrointestinal bleeding.
If the disease has an uncomplicated course, then it is possible to use the drug Tranexam. In difficult cases, Tranexam is combined with Etamsylate or Dicinone.
Possible complications and consequences
The consequences of this disease of the blood system can be:
- Development of acute or chronic posthemorrhagic anemia.
- Arterial hypotension. Occurs against the background of severe blood loss.
- Heavy bleeding during childbirth.
- Subarachnoid hemorrhages (hemorrhagic stroke). May lead to speech, motor and visual disturbances. High probability of death.
- Hematuria.
- Arthrosis and limitation of joint movements. Observed against the background of hemarthrosis.
- Synovitis (inflammation of the synovial membrane).
Important information: Signs of drug (oil) embolism and what to do to prevent it
Prevention
To reduce the risk of developing von Willebrand disease, the following preventive recommendations must be followed:
- exclude possible marriage between sick people;
- stop using certain medications (NSAIDs, antiplatelet agents);
- prevent injuries and infectious diseases;
- carry out clinical observation;
- lead a healthy lifestyle, eliminating all bad habits;
- eat well.
Specific prevention has not been developed.
Causes and risk factors
The development of the disease is based on insufficient production of von Willebrand factor. It is synthesized by megakaryocytes and vascular endothelial cells. Risk factors for Diana von Willebrand disease are:
- Gene mutations. The gene responsible for the production of this substance is localized on chromosome 12.
- Burdened heredity. The disease is inherited in an autosomal dominant (types 1 and 2) and autosomal recessive (type 3) types.
- Frequent transfusion of blood components.
- Oncological pathology (malignant kidney tumors, Wilms tumor).
- Macroglobulinemia (gammopathy). Characterized by the formation of pathological immunoglobulins.
- Systemic connective tissue diseases (rheumatoid arthritis, rheumatism, systemic lupus erythematosus).
- Heart disease (narrowing of the aortic valve).
- Autoimmune disorders (formation of autoantibodies that damage blood vessels, platelets and von Willebrand factor).
Classification
The following forms of von Willebrand disease are distinguished:
- Classic (type 1). Is the most common. It is characterized by a normal spectrum of oligomers, the presence of moderate forms of multimers and a moderate deficiency of coagulation factor 8.
- Type 2 It is characterized by a qualitative violation of the production of von Willebrand factor. Its activity decreases, but the concentration is within normal limits. There is impaired affinity for receptor cells, decreased cofactor activity, poor binding to receptors, and impaired factor inactivation.
- Type 3 Characterized by a quantitative defect of factor 8. Its concentration in blood plasma is sharply reduced. There is a sharp decrease in activity.
- Platelet. Characterized by increased binding of coagulation factor to altered receptor structures. Concentration is within normal limits.
Important information: Signs of cardiogenic shock and how to provide first emergency (pre-hospital) aid (action algorithm)