Home » Department of Vascular Surgery » Diseases » Buerger's disease
Buerger's disease (or thromboangiitis obliterans) is a systemic inflammatory immunopathological disease of veins and arteries, especially small and medium-sized ones, with elements of an autoimmune nature.
The disease was first described in 1908 by L. Burger. Men at a young age get sick more often than women, and the pathological process is characterized by a certain localization and a set of clinical manifestations. Thus, Buerger's disease often starts with damage to the small arteries of the feet and hands. The main development factor is a pronounced inflammatory process, which causes arterial and venous blockage in the later stages of the disease, as well as compression of the entire neurovascular bundle by overgrown connective tissue. The disease progresses rapidly, with frequent exacerbations, which are usually provoked by cold or smoking.
This disease is widespread in Japan, Israel, India (the “Silk Road” countries), and in the countries of South Asia; it is much less common in Europe and the USA.
Causes of Buerger's disease
The exact cause has not been established, but the following development factors are identified:
- An infectious factor is a disease similar to viral, salmonella, streptococcal, rickettsial and chlamydial infections.
- Neuroendocrine factor - the development of spasm in the microcirculation system due to high levels of adrenaline in the blood, which is the result of increased adrenal function.
- Neurogenic factor - spastic dystrophy, thrombus formation and blockage of peripheral arteries due to organic changes in the nerve trunks.
- Autoimmune factor - the production of autoantibodies to collagen, elastin, endothelial cells, laminin with the formation of CIC (circulating immune complexes) and the development of antiphospholipid syndrome.
- Genetic factor – the disease is endemic.
- Tobacco smoking - nicotine has a toxic and hypoxic effect on endothelial cells, reducing the production of vasoactive peptides with the development of spasm, thrombosis and occlusion of peripheral arteries.
- Damaging factors - allergic reactions, trauma, frostbite, arsenic intoxication.
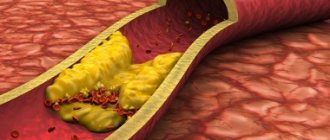
Morphologically, inflammation of the walls of small and medium-sized veins and arteries of the extremities occurs in the vessels, and blood clots can form. In the late stage, perivascular proliferation of connective tissue develops, blocking the lumen of blood vessels. The inflammatory process has a wave-like course, i.e. for months, years, leading to blockage of blood vessels.
Treatment
To help patients suffering from Buerger's disease, the department carries out the following therapeutic measures:
• Conservative treatment of inflammation. It consists of the combined administration of vasodilators, antithrombotic and analgesic drugs, as well as other symptomatic drugs in long courses. At the same time, smoking cessation is strongly recommended.
• Lumbar or thoracic sympathectomy is sometimes performed to relieve spasm.
• In the later stages of the disease, our surgeons perform vascular prosthetics. Operations are performed quite rarely due to the small size of the vessels affected by the disease.
• Too advanced cases risk amputation of the limb, which is performed by a thoracic surgeon. The department's specialists are making every effort to prevent such a situation. But for patients who do not adhere to the recommended prescriptions, the measure may be forced.
Symptoms of Buerger's disease
Buerger's disease is usually suspected when men between 20 and 40 years of age develop characteristic complaints associated with chronic ischemia (lack of blood flow) of the lower extremities, such as chilliness of the extremities, high sensitivity to low temperatures, weakness of the lower extremities, paresthesia, numbness, convulsions. Trophic skin disorders may appear in the form of ulcers on the feet and fingers, necrosis or gangrene.
The pathological process starts with superficial migrating nodular phlebitis (inflammation of the veins). The nodules have a certain localization, accompanied by skin erythema (redness), tension when touched. Cold sensitivity is often noted on the hands, i.e. When exposed to cold, the fingers first turn white, then blue, and finally red.
One of the characteristic and typical symptoms is periodic pain in the instep of the foot during physical activity, and disappears quickly with rest. Pain rarely occurs in the ankle area, which happens when the disease does not spread proximally and does not affect either the superficial femoral or popliteal arteries by blockage. When the hands are affected, the blockages are usually bilateral, symmetrical, leading to pain in the hands, as well as the appearance of very painful and difficult-to-heal ulcers on the fingers.
Symptoms of the disease
Three main signs of Buerger's disease:
• manifestations of vascular insufficiency of the extremities (pain, feeling of fullness, goosebumps, chilliness);
• migrating thrombophlebitis;
• lameness even in the initial stages.
Poor circulation begins at the fingertips and spreads upward. Sometimes foot ischemia develops. Over time, the patient's condition worsens. In half of the cases, Raynaud's disease develops, and the cerebral, visceral and coronary vessels are involved in the process.
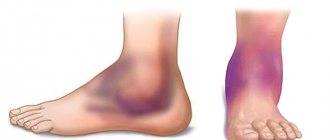
Complications of the disease can be a variety of trophic disorders: hyperhidrosis, anhidrosis, tissue atrophy and necrosis, ulcers and even gangrene.
Diagnosis of Buerger's disease in Israel
The absence of typical clinical and laboratory signs makes diagnosis difficult.
- When complaints of intermittent claudication appear in men 20-40 years old, smokers can think of Buerger's disease.
- Physical examination : intense redness of the feet is detected, there is no pulse in the feet, while it is preserved in the femoral and popliteal arteries, the frequency and filling of the pulse are reduced; thromboangiitis obliterans may be suspected in the patient.
- Doppler ultrasound
- Electrothermometry
- Rheovasography
- Capillaroscopy and graphy
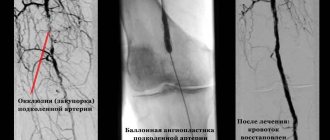
- Angiography : segmental vasoconstriction is noted, often symmetrical, which distinguishes this from the atherosclerotic process, characterized by asymmetry and diffuse damage along the vessel.
Medical Internet conferences
Relevance of the problem. Nowadays, there is an increasing increase in the incidence of systemic vasculitis, especially in people of working age. This is due both to diagnostic difficulties and to a significant increase in the impact of adverse (viral, chemical, toxic) environmental factors on the human body, causing the development of immune inflammation in the walls of blood vessels. Systemic vasculitis (SV) is a group of diseases based on generalized damage to the vascular wall of immune origin with the development of inflammation and necrosis, leading to impaired blood flow in organs and tissues. Systemic vasculitis is one of the most severe forms of human chronic inflammatory diseases.[1]
With various vasculitis, the severity of clinical manifestations, as well as the prognosis, will depend both on the nature of the immune-inflammatory process in the vascular wall, and on the type, caliber and location of the affected vessels, the course and severity of concomitant inflammatory changes in the tissues.[1] Among the most common vasculitis affecting small and medium-sized vessels, our attention was drawn to thromboangiitis obliterans, or in the English literature, “Winiwarter-Buerger disease.” The disease is more common in young men with a long history of smoking, while the progression of the pathological process with an increase in ischemic disorders in the extremities and changes in the vessels of internal organs lead to early disability of patients.[2] Today, there is no doubt about the relationship between immune inflammation and the development of thrombosis due to the fact that these processes are based on many similar pathogenetic mechanisms. Complications of a thrombotic nature remain one of the most severe and life-threatening conditions that occur in patients with systemic vasculitis. [3]
Objective: To demonstrate the diagnostic difficulties in managing a patient with Buerger's disease. Objectives: analysis of a clinical case of a patient suffering from thromboangiitis obliterans with assessment of clinical and laboratory-instrumental data with the establishment of leading syndromes, use of diagnostic criteria “disease development”, “treatment effect” when making a diagnosis.
Materials and methods: a retrospective analysis of the medical history and supervision of a patient with a final diagnosis of Buerger's disease involving the vessels of the upper and lower extremities was carried out.
Results: Patient N., 40 years old, was admitted to the cardiology department of the S.R. Clinical Hospital. Mirotvortseva SSMU on March 28, 2021 with complaints of mixed shortness of breath at rest and in a position with a low head, tachycardia, weakness accompanied by cold sweat, pain in the left leg, in the right half of the chest. From the anamnesis it is known that the symptoms manifested acutely: on March 26, for no apparent reason, constant pain appeared in the left lower leg, inspiratory shortness of breath with slight physical exertion, and severe weakness. However, the symptoms did not increase and he continued to lead his usual lifestyle (went to work). On March 28, he noted a sharp deterioration in his general condition: severe weakness appeared, severe shortness of breath, and he broke out in a cold sweat. He was taken to the cardiology department by ambulance with a preliminary diagnosis of pulmonary embolism (PE). From his life history it is known that over the past 6 years he suffered three times severe pneumonia, complicated by hemoptysis. I suffered from arterial hypertension for about 5 years.
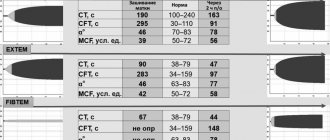
Upon admission, the condition was assessed as severe, the skin was pale, acrocyanosis, and pastiness of the left leg. Prefers a position with an elevated headboard. The respiratory rate is 22 per minute, shallow breathing, with an open mouth. Auscultation of the lungs reveals harsh breathing, weakened on the right in the lower parts, no wheezing. The borders of the heart are expanded to the left to the left midclavicular line. The heart sounds are weakened, the emphasis of the 2nd tone is on the pulmonary artery. Blood pressure 100 and 60 mmHg. Heart rate 100 per minute. Plesh's symptom is negative. The abdomen is slightly painful on palpation in the right hypochondrium. The liver cannot be detected by palpation. In other organs there are no features. Additional examination revealed: moderate leukocytosis (up to 16*109/l), increased level of C-reactive protein (CRP) to 28 mg/l, ALT, AST more than 2 upper limits of normal; the level of markers of myocardial necrosis (troponins, CPK-MB), coagulogram parameters are normal. An electrocardiographic study (ECG) revealed a deviation of the electrical axis of the heart to the right, right bundle branch block, QIII, SI. On March 29, a duplex scan of the veins of the lower extremities was performed, which revealed thrombosis of the popliteal and superficial femoral veins on the left with the apex of the thrombus localized in the superficial femoral vein at the level of the c/3 thigh; passable lumen of veins from 10% to 60%. Doppler echocardiography (DEchoCG) revealed signs of significant dilatation of the right ventricle (RV) and moderate dilatation of the right atrium (RA). In the cavity of the RA, two ribbon-like floating thrombi were identified, about 5.0 and 7.0 cm long, about 1.0 cm thick, which from the mouth of the vena cava reached the tricuspid valve (TV) leaflets. There were no echo signs of TC obstruction. Tricuspid regurgitation is significant (grade III). Paradoxical movement of the interventricular septum, caused by volume overload of the RV, and hyperkinesis of the posterior wall were determined. Myocardial thickness, chamber size and global contractility of the left ventricle were normal (ejection fraction about 63% according to the Teichgolz formula). Signs of cardiac decompensation in the systemic and pulmonary circulation were established (dilation of the inferior vena cava (IVC) up to 2.7 cm without signs of collapse, high-grade pulmonary hypertension - systolic pressure in the pulmonary artery (SPAP) 80 mmHg). An ultrasound examination of the abdominal cavity revealed signs of hepatomegaly and congestion in the IVC system. When X-raying the chest organs, there was an increase in the pulmonary pattern in the basal sections due to full-blooded vessels; in the area of the apexes of the lungs and the marginal border of the pulmonary fields, the pulmonary pattern was not traced. The mediastinal organs are unremarkable.
Based on the development of the disease (male gender, onset of the disease before 40 years of age, recurrent venous thrombosis complicated by embolism, increased levels of CRP), it was suggested that the patient has Buerger's disease, which has an atypical course (absence of clinical and instrumental signs of arterial damage).[ 4]
Treatment with anticoagulants, calcium channel blockers, β-blockers, glucocorticoids, antibacterial therapy, and gastroprotection was prescribed. Considering that the patient has a very high risk of developing pulmonary embolism (13 points on the GENEVA scale) and echocardiography data (blood clots in the RA cavity), a decision was made to conduct thrombolytic therapy with streptokinase. During treatment, the patient's condition improved significantly: chest pain, shortness of breath at rest were relieved, and exercise tolerance increased. On April 11, a repeat echocardiogram was performed, which showed positive dynamics in the form of lysis of one of the thrombi and a reduction in the size of the second (in the RA, one ribbon-like floating thrombus is visualized, about 5.0 cm long and about 0.6 cm thick, reaching the TC). Tricuspid regurgitation (I degree) and pulmonary hypertension (I degree, MPAP 36 mm Hg) decreased, signs of circulatory failure in the systemic circle stopped (IVC 1.8 cm, collapses on inspiration). On April 12, 2021, a repeat duplex scan of the veins of the lower extremities was performed, where an improvement was also noted in the form of a decrease in the length of the blood clot.
Conclusion. This clinical case clearly demonstrated the atypical course of Buerger's disease. As a rule, thromboangiitis obliterans is a chronic disease of small and medium-sized arteries and veins. The clinical picture of the disease is dominated by signs of damage to the veins of the lower extremities, which is quite rare.[5] Quick diagnosis, choice of rational patient management tactics and the use of high-tech medical care significantly improve the prognosis of the disease.
Treatment of Buerger's disease in Israel
Conservative therapy is prescribed for the spastic stage:
- Elimination of the cause (cooling, smoking)
- Dosed walking is recommended to develop vascular collaterals in the extremities
- Elimination of vascular spasm (antispasmodics, ganglion blockers, peripheral anticholinergics (andecalin, padutin, kallikrein depot), nicotinic acid preparations.
- Normalization of central nervous system functions (sedatives, anxiolytics)
- Physiotherapeutic methods (diadynamic currents, diathermy on the lumbar region)
- Improving rheology (movement through blood vessels) of blood
- Normalization of blood coagulation and anticoagulation systems: prescription of anticoagulants (heparin, clexane, fraxiparin) and antiplatelet agents (aspirin, clopidogrel) to reduce the risk of thrombosis and increase the “fluidity” of blood in the capillaries
- Corticosteroid drugs
- In patients with secondary infection, antibiotics are prescribed
- Plasmapheresis and hyperbaric oxygenation
Surgical treatment includes:
- Radical operations : endarterectomy (removal of the endothelium of a vessel with a length of arterial blockage up to 15 cm), bypass surgery (creation of a shunt to bypass the narrowed section of the artery), prosthetics (use of explants), stenting (installation of a stent frame in a vessel).
- Palliative operations : Leriche operation (circular removal of the outer membrane of the main arteries), periarterial sympathectomy, lumbar sympathectomy according to Diets, transplantation of the greater omentum to the lower leg, arterialization of the venous bed, use of autologous blood.
- In case of necrosis of the affected fingers, amputation ;
- In case of gangrene of the foot or its toes, low (economical) amputation is performed.
Please note that all form fields are required. Otherwise we will not receive your information. Alternatively use
Recommendations
A person suffering from Buerger's disease must immediately stop smoking - otherwise the disease will only progress. In addition, the patient should avoid skin damage due to exposure to high or low temperatures, chemicals, lesions associated with wearing uncomfortable shoes, minor operations (for example, callus removal), fungal infections.
All patients (except patients with ulcers and gangrene on the affected limbs) are recommended to walk briefly (20-30 minutes) several times a day.
Video from YouTube on the topic of the article:
Diagnosis and treatment
The primary diagnosis of thromboangitis obliterans at the MedicCity clinic is established by a doctor based on a survey of the patient, visual examination and palpation (feeling). The patient is then offered immunological tests.
After confirming the diagnosis (if it is not a late stage of thromboangitis obliterans), drug treatment is prescribed: vasodilators, anti-inflammatory and other drugs. The patient is also recommended to take regular walks.
A patient with thromoboangiitis obliterans is strongly recommended to quit smoking, since smoking significantly increases the risk of exacerbations of this disease and neutralizes the effectiveness of treatment.
If the patient has pain at rest, ulceration, or gangrene, he is indicated for inpatient treatment. A course of intensive drug therapy is prescribed, and the need for surgical intervention is decided. To minimize injury to the limbs, the patient is offered special bandages.
Be attentive to your health - trust the care of it to professionals! Our clinic employs only highly qualified specialists and well-proven techniques.
Reasons for the development of thromboangitis obliterans
The etiology of thromboangitis obliterans, that is, the reasons that provoke the development of this disease, is still not completely clear.
Among the identified factors causing the development of the disease are the following:
- infections;
- hereditary diseases of blood vessels;
- production of increased amounts of adrenaline by the adrenal glands;
- organic changes in nerve trunks;
- toxic poisoning;
- allergies;
- injuries;
- consequences of improper protein diets and cosmetic injections.
Types of disease
Thrombangitis obliterans is considered a type of obliterating endarteritis.
The most common type is distal thromboangitis obliterans, which obstructs blood flow in small-diameter arteries and leads to damage to the feet, legs, forearms and hands.
There are also a proximal type, in which obliteration of arteries of medium and large diameter occurs (iliac, aorta, femoral) and a mixed type, combining distal and proximal types of thromboangitis obliterans.