Obliterating atherosclerosis of the vessels of the lower extremities
Obliterating atherosclerosis of the vessels of the lower extremities is a chronic vascular disease that develops due to lipid metabolism disorders, leading to the formation of atherosclerotic plaques, thickening of the walls of the arteries of the legs and a decrease in the vascular lumen.
All these changes can lead to partial or complete cessation of blood flow. At first, this pathology practically does not manifest itself in anything, but as this disease progresses, atherosclerotic plaques increasingly narrow the lumen of the vessels and can completely block it, leading to ischemia and even necrosis of the tissues of the lower extremities. This development of the disease can result in the development of gangrene and loss of a leg.
What it is?
Obliterating atherosclerosis is one of the forms of atherosclerosis. With this disease, cholesterol plaques form on the walls of the arteries, they disrupt normal blood flow, causing vasoconstriction (stenosis) or its complete blockage, called occlusion or obliteration, therefore they speak of occlusive-stenotic damage to the arteries of the legs.
According to statistics, the prerogative of having pathology belongs to men over 40 years of age. Obliterating atherosclerosis of the lower extremities occurs in 10% of the total population of the Earth, and this number is constantly growing.
Healthy lifestyle, proper nutrition and diets
Diet is a fundamental principle in the prevention and treatment of dangerous vascular pathology.
The main principle of rational nutrition is to minimize the intake of cholesterol and animal fats with food.
If you have obliterating atherosclerosis or if there is a high risk of its development, it is strictly forbidden to use :
- fat meat;
- smoked meats;
- sausages;
- canned food;
- offal;
- high fat dairy products;
- fast food dishes;
- baked goods and sweets;
- margarine;
- butter;
- factory sauces.
Advice! Allowed foods include dietary meat (rabbit, veal, chicken), sea fish, cereals, vegetable soups, vegetables and fruits, shortbread cookies, low-fat dairy products, nuts and eggs (2-3 per week).
Causes
The main cause of atherosclerosis is smoking. The nicotine contained in tobacco causes the arteries to spasm, thereby preventing blood from moving through the vessels and increasing the risk of blood clots in them.
Additional factors that provoke atherosclerosis of the arteries of the lower extremities and lead to an earlier onset and severe course of the disease:
- increased cholesterol levels due to frequent consumption of foods rich in animal fats;
- high blood pressure;
- excess weight;
- hereditary predisposition;
- diabetes;
- lack of sufficient physical activity;
- frequent stress.
Frostbite or prolonged cooling of the legs suffered at a young age of frostbite can also be a risk factor.
Risk group
Persons over 40 years of age, especially representatives of the stronger sex, are at risk of becoming a victim of obliterating atherosclerosis. For women, this insidious disease usually strikes after menopause, when the gonads begin to fade. Before menopause, active hormonal levels protect the female body from cholesterol deposits.
Also at risk are people who lead an unhealthy and sedentary lifestyle, suffer from addictions, and are prone to overeating. Modern medicine identifies a family history of obliterating atherosclerosis as an additional risk factor.
Development mechanism
Most often, atherosclerosis of the vessels of the lower extremities manifests itself in old age and is caused by disorders of lipoprotein metabolism in the body. The development mechanism goes through the following stages.
- Cholesterol and triglycerides that enter the body (which are absorbed into the intestinal walls) are captured by special transport proteins - chylomicrons and transported into the bloodstream.
- The liver processes the resulting substances and synthesizes special fatty complexes - VLDL (very low density cholesterol).
- In the blood, VLDL molecules are affected by the enzyme lipoprotein lipase. In the first stage of the chemical reaction, VLDL is transformed into intermediate-density lipoproteins (or IDL), and then in the second stage of the reaction, IDL is transformed into LDL (low-density cholesterol). LDL is the so-called “bad” cholesterol and it is the one that is more atherogenic (i.e., capable of provoking atherosclerosis).
- Fatty fractions enter the liver for further processing. Here, high-density cholesterol (HDL) is formed from lipoproteins (LDL and LPPP), which has the opposite effect and is able to cleanse the walls of blood vessels from cholesterol deposits. This is the so-called “good” cholesterol. Part of the fatty alcohol is processed into digestive bile acids, which are necessary for normal food processing and are sent to the intestines.
- At this stage, the liver cells may fail (genetically or due to old age), as a result of which, instead of HDL at the output, low-density fat fractions remain unchanged and enter the bloodstream.
Mutated or otherwise altered lipoproteins are no less, and perhaps more atherogenic. For example, oxidized under the influence of H2O2 (hydrogen peroxide).
- Low-density fat fractions (LDL) settle on the walls of the arteries of the lower extremities. Prolonged presence of foreign substances in the lumen of blood vessels promotes inflammation. However, neither macrophages nor leukocytes can cope with cholesterol fractions. If the process is delayed, layers of fatty alcohol - plaques - form. These deposits are very dense and interfere with normal blood flow.
- Deposits of “bad” cholesterol are encapsulated, and when the capsule is ruptured or damaged, blood clots form. Blood clots have an additional occlusive effect and further clog the arteries.
- Gradually, the cholesterol fractions, together with blood clots, take on a rigid structure due to the deposition of calcium-containing salts. The walls of the arteries lose their normal extensibility and become fragile, resulting in possible ruptures. In addition to this, persistent ischemia and necrosis of nearby tissues is formed due to hypoxia and lack of nutrients.
Stages
During obliterating atherosclerosis of the lower extremities, the following stages are distinguished:
- Stage I (initial manifestations of stenosis) – a feeling of goosebumps, pale skin, a feeling of coldness and chilliness, excessive sweating, rapid fatigue when walking;
- Stage II A (intermittent claudication) – a feeling of fatigue and stiffness in the calf muscles, squeezing pain when trying to walk about 200 m;
- Stage II B – pain and feeling of stiffness prevent you from walking 200 m;
- Stage III – squeezing pain in the calf muscles becomes more intense and appears even at rest;
- Stage IV – signs of trophic disorders, long-term non-healing ulcers and signs of gangrene appear on the surface of the leg.
In advanced stages of atherosclerosis of the lower extremities, the development of gangrene often leads to complete or partial loss of a limb. The lack of adequate surgical care in such situations can lead to the death of the patient.
According to prevalence, obliterating atherosclerosis is divided into stages:
- Segmental obliteration - only one limb fragment falls out of the microcirculation area;
- Widespread occlusion (2nd degree) – block of the superficial femoral artery;
- Blockage of the popliteal and femoral artery with impaired patency of the bifurcation area;
- Complete blockade of microcirculation in the popliteal and femoral arteries – 4th degree. In case of pathology, blood supply is maintained through the system of deep femoral arteries;
- Damage to the deep femoral artery with damage to the femoral-popliteal region. Grade 5 is characterized by severe hypoxia of the lower extremities and necrosis, trophic ulcers and gangrene. The severe condition of a bedridden patient is difficult to correct, so treatment is only symptomatic.
Types of occlusive-stenotic lesions in atherosclerosis are represented by 3 types:
- Damage to the distal part of the tibial and popliteal arteries, in which the blood supply to the lower leg is preserved;
- Occlusion of blood vessels of the leg. Patency of the tibial and popliteal arteries is preserved;
- Occlusion of all vessels of the thigh and leg while maintaining patency of individual branches of the arteries.
How does atherosclerosis of the coronary vessels manifest?
The atherosclerotic process can begin at a young age and last for decades, only with a combination of predisposing factors and a narrowing of the lumen of the vessel by half or more, can it make itself felt with the following conditions:
- stable and unstable angina. Characterized by cardiac and chest pain, shortness of breath when moving, and in the advanced stage and at rest, the heart works intermittently;
- myocardial infarction. Gives unbearable chest pain, pronounced fear of death, a sharp drop in blood pressure, reaching shock. The severity of the consequences depends on the location and size of the dead zone. The damaged part of the heart will no longer be able to recover.
The destruction of the arteries supplying the heart can be asymptomatic for a long time and the person will not complain of any abnormalities, which is why it is so important to undergo annual examinations and tests.
Symptoms
Symptoms of OASNK in the initial stages are usually quite vague or absent altogether. Therefore, the disease is considered insidious and unpredictable. It is this damage to the arteries that tends to develop gradually, and the severity of clinical signs will directly depend on the stage of development of the disease.
The first signs of obliterating atherosclerosis of the lower extremities (second stage of the disease):
- feet begin to constantly freeze;
- legs often go numb;
- swelling of the legs occurs;
- if the disease affects one leg, then it is always colder than the healthy one;
- Pain in the legs appears after a long walk.
These manifestations appear in the second stage. At this stage of development of atherosclerosis, a person can walk 1000–1500 meters without pain.
People often do not attach importance to symptoms such as freezing, periodic numbness, pain when walking long distances. But in vain! After all, by starting treatment at the second stage of the pathology, you can 100% prevent complications.
Symptoms that appear at stage 3:
- nails grow slower than before;
- hair begins to fall out on the legs;
- pain can occur spontaneously both day and night;
- pain appears after walking short distances (250–900 m).
When a person has stage 4 of obliterating atherosclerosis of the legs, he cannot walk 50 meters without pain. For such patients, even going shopping, and sometimes just going out into the yard, becomes an impossible task, as going up and down the steps turns into torture. Often patients with stage 4 disease can only move around the house. And as complications develop, they stop getting up at all.
At this stage, treatment of the disease, obliterating atherosclerosis of the lower extremities, often becomes powerless; it can only briefly alleviate the symptoms and prevent further increases in complications, such as:
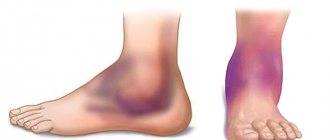
- darkening of the skin on the legs;
- ulcers;
- gangrene (this complication requires amputation of the limb).
Consequences and complications
Sometimes, after surgery, some complications and consequences may occur.
List of complications of obliterating atherosclerosis of the arteries::
intermittent claudication, the patient needs help with movement, even crutches;- hematomas at puncture sites, which are very noticeable and require covering under clothing;
- thrombosis or rupture of an artery (this complication is extremely rare);
- calcinosis is characterized by fragility of tissues and bones; it is also painful for a person to walk and, most often, he needs help.
If the disease relapses, it is recommended to carry out a second course of treatment, and, if necessary, carry out additional treatment procedures.
IMPORTANT! It should be remembered that the reappearance of symptoms may indicate progression of the disease.
Features of the flow
All symptoms of the disease develop gradually, but in rare cases, obliterating atherosclerosis of the vessels of the lower extremities manifests itself in the form of arterial thrombosis. Then, at the site of arterial stenosis, a blood clot appears, which instantly and tightly blocks the lumen of the artery. Such a pathology develops unexpectedly for the patient; he feels a sharp deterioration in health, the skin of the leg turns pale and becomes cold. In this case, a quick visit to a vascular surgeon (counting the time to irreversible events by the clock) allows the person to save his leg.
With a concomitant disease—diabetes mellitus—the course of obliterating atherosclerosis has its own characteristics. The history of such pathologies is not uncommon, and the disease develops so rapidly (from several hours to several days) that in a short time it leads to necrosis or gangrene in the lower extremities. Unfortunately, doctors often resort to leg amputation in such situations - this is the only thing that can save a person’s life.
Which doctor should I contact?
When the first signs of the disease appear, a visit to the doctor should take place as early as possible. During the initial visit, a diagnosis can be made by a local physician, who will also prescribe diagnostic measures and treatment tactics.
However, it is better to contact a specialized specialist who is more deeply familiar with the problem and will conduct proper diagnosis and treatment of atherosclerosis.
Who can I contact?:
- angiologist - a doctor who treats the arteries and lymphatic system;
- phlebologist – specializes in vein diseases;
- neurologist – studies and treats circulatory disorders;
- vascular surgeon is a doctor who practices surgical treatment methods.
Note! Related specialists are endocrinologist, cardiologist, neurologist. They will help patients suffering from diabetes, angina pectoris, arterial hypertension or nervous disorders, which are prerequisites for the occurrence of obliterating atherosclerosis.
Diagnosis of the disease
The diagnosis of “obliterating atherosclerosis of the vessels of the lower extremities” is made based on the following data:
- Characteristic complaints of the patient (pain syndrome, intermittent claudication).
- On examination, signs of atrophy of the soft tissues of the limb are noted.
- Rheovasography of the extremities shows a pronounced decrease in the index on the legs and feet.
- Reducing the level of pulsation in the arteries of the feet, legs, popliteal and femoral arteries. If the area of the aortic bifurcation is affected, there may be a lack of pulsation in both femoral arteries (Leriche syndrome).
- Thermometry, thermography – reducing tissue temperature and the level of infrared radiation.
- Ultrasound of the vessels of the legs (Dopplerography) indicates a violation of the blood supply to the peripheral parts.
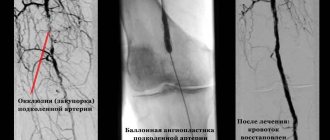
- Arteriography (a study that involves injecting a contrast agent into the arteries of the legs) shows the area of narrowing of the artery of the limb.
- Tests with functional load - decreased load tolerance, rapid fatigue and the appearance (or intensification) of ischemic pain.
How to prevent the development of gangrene?
Obliterating atherosclerosis is one of the most common causes of gangrene and amputation of the lower extremities. Severe complications can be avoided by strictly following the recommendations for the prevention of obliterating atherosclerosis.
Additionally, you should pay attention to:
- Shoes. Properly selected shoes prevent injury and rubbing of the feet;
- Temperature outside the window. Hypothermia and frostbite are the main enemies of the lower extremities;
- Amount of sugar consumed. “Sweet” blood provokes tissue destruction and slows down wound healing;
- Wounds, cracks and other skin damage. Timely treatment of wounds and burns is the key to healthy skin;
- Physical activity. Moderate exercise improves blood supply to tissues, but excessive activity can overwork the legs and worsen the condition.
Treatment of obliterating atherosclerosis
Conservative treatment of patients with obliterating atherosclerosis of the arteries of the lower extremities is carried out in the following cases:
- at the stage of chronic arterial circulatory failure in the extremities according to the classification of A. V. Pokrovsky - Fontane;
- with severe concomitant pathology: coronary disease, cerebral vascular damage, chronic diseases of the lungs, liver, kidneys, diabetes mellitus;
- multiple (multi-story) occlusions and stenoses of the main arteries;
- lesions of the distal vascular bed.
It assumes:
- sedative therapy (seduxen, elenium);
- desensitizing therapy (diphenhydramine, pipolfen);
- pain relief (analgesics, intra-arterial agents, blockades of 1% novocaine solutions, paravertebral blockades at the L2 - L3 level, epigastric blockades);
- exclusion of vascular risk factors (smoking, alcohol, excessive cooling, nervous stress, physical inactivity, diabetes mellitus);
- improving the rheological properties of blood, i.e. reducing its viscosity (plasma substitutes - dextrans, defibrinogenic enzymes - acrod, pentoxifylline, trental, vasonite, agapuria);
- elimination of vascular spasm (antispasmodics - no-shpa, halidor, xanthinol nicotinate; gangioblockers - hexonium, dicaine);
- normalization of the blood coagulation system (anticoagulants);
- inhibition of platelet adhesive-aggregation activity (acetylsalicylic acid, ticlide);
- restoration of oxidant-antioxidant balance - protection of cell membranes (antioxidants - vitamins A, E, C, probucol);
- activation of metabolic processes in tissues (vitamins, nicotinic acid, complamin, solcoseryl, bradykinin inhibitors - prodectin, parmidine);
- elimination of immune disorders (immunomodulation, immunosorption, ultraviolet radiation of blood);
- normalization of lipid metabolism. It includes diet therapy, the prescription of lipid-lowering drugs, the use of extracorporeal methods for correcting the composition and properties of circulating blood, partial jejunoileobypass surgery, and gene therapy.
Diet therapy for obliterating atherosclerosis is based on limiting the energy value of food intake to 2000 kcal per day with a decrease in the proportion of fat (up to 30% or less) and cholesterol (less than 300 mg). It is justified to prescribe antiatherogenic nutritional supplements to patients, such as polyunsaturated fatty acids, fish oil, eikonol (a nutritional supplement obtained from certain types of fish).
If there is no normalization of lipid metabolism parameters during diet therapy, without stopping it, drug treatment is carried out. Currently, five groups of lipid-lowering drugs are used for the treatment and prevention of atherosclerosis:
- enterosorbents - cholestyramine, which are sequestrants of bile acids;
- statins - lovastatin (Mevacor), simvastatin (Zocor), privastatin (Lipostat), fluvastatin (Leskol)
- fibrates - mofibrate, otofibrate;
The effectiveness of conservative therapy is assessed by factors affecting lipid metabolism, primarily by the level of total cholesterol and LDL cholesterol.
Normal triglyceride levels are 150 mg/dL. Extracorporeal methods for correcting the composition and properties of circulating blood: plasmapheresis; selective immunosorption, including on sorbents with monoclonal antibodies to LDL (especially effective in the treatment of patients with severe hetero- and homozygous hypercholesterolemia); hemosorption. These methods make it possible to obtain a persistent hypolipidemic effect, which consists in reducing the level of LDL in the blood and increasing the content of HDL, reducing the atherogenic coefficient. This slows down the progression of atherosclerotic arterial occlusion. However, if conservative correction of hyperlipidemia is unsuccessful, there is a tendency for the process to progress, especially in early atherosclerosis, significant clinical manifestations of atherosclerosis in patients with its generalized form, which is usually observed in people with familial hypercholesterolemia, when the cholesterol level exceeds 7.5 mmol/l, In cases of severe xanthomatosis, a partial jejunoileal shunt operation (Buchwald operation) can be performed.
The essence of this surgical intervention is to exclude the distal third of the small intestine from digestion and anastomose the proximal 2/3 of the small intestine with the dome of the cecum. The colon has the ability to synthesize and secrete several types of lipids and their apoproteins, influence hepatic synthesis and secretion of lipids through absorption and enterohepatic circulation of bile acids (BAs) and cholesterol. A decrease in the length of the functioning part of the small intestine leads to impaired absorption of FAs and acceleration of their excretion, an increase in the synthesis of fatty acids in the liver, increasing the oxidation of cholesterol, a decrease in the intestinal synthesis of cholesterol, chylomicrons, VLDL, a decrease in lipid absorption and subsequent inhibition of the synthesis of atherogenic lipoproteins in the liver. A side effect of Buchwald's operation is the frequent development of diarrhea, impaired absorption of vitamin B12 and folic acid.
Two main methods of gene therapy for obliterating atherosclerosis have been developed. The essence of the first of them is to introduce a gene encoding a normal protein - a receptor for LDL, with the help of a retrovirus, into a culture of hepatocyte cells of the patient, and then, through a catheter installed in the portal vein, to deliver a suspension of such cells to the patient's liver. After their engraftment, the donor's normal receptors begin to function. The disadvantage of the method is the need for the patient to take significant doses of statins and a gradual decrease in the function of the introduced genes.
The second (direct) method is performed on a patient without prior manipulation of target cells, while the gene is complexed with a carrier (vector) and directly introduced into the patient, but locally - into the cardiovascular system to avoid dissemination of the gene in the body. Direct administration is carried out using a viral infection, chemical or physical method,
In the complex of conservative treatment of patients with atherosclerosis, especially with stages III - IV of chronic arterial insufficiency of the extremities, it is advisable to include drugs with a complex mechanism of action; 1) tanakan - stimulates the production of relaxation factor by the vascular endothelium. The drug has a vasodilating effect on small arterioles, reduces capillary permeability, reduces platelet and red blood cell aggregation, protects cell membranes by suppressing lipid peroxidation reactions, improves the absorption of glucose and oxygen by tissues; 2) prostaglandins and their synthetic derivatives (vasoprostan). They influence all stages of the development of ischemic syndrome in the limb, have a vasodilating effect, suppress platelet aggregation, improve microcirculation, and normalize metabolic processes in ischemic tissues.
Patients with obliterating atherosclerosis of the vessels of the lower extremities are prescribed physiotherapeutic, balneological and sanatorium-resort treatment (magnetic therapy with pulsed and direct currents with effects on the lumbar sympathetic ganglia and lower extremities, interference currents on the lower extremities and lumbar spine, massage of the lower extremities, reflex-segmental massage of the spine , radon, hydrogen sulfide baths, acupuncture, hyperbarotherapy).
One of the most modern methods of physiotherapeutic treatment of patients with obliterating atherosclerosis of the vessels of the lower extremities is electrical stimulation of the spinal cord. It is performed if it is impossible to perform reconstructive operations on the arteries due to the prevalence of occlusive lesions with systolic pressure at the ankle level less than 50 mm Hg. Art. The essence of the method is the percutaneous introduction of a quadripolar electrode into the epidural space of the lumbar spine, extending its apex to the T12 level and positioning it in the midline. During the first week, electrical stimulation of the spinal cord is carried out with a pulse frequency of 70 - 120 Hz from an external source. If a positive clinical result is obtained, the generator is implanted into the subcutaneous tissue of the anterior abdominal wall and programmed for continuous or intermittent operation. Electrical stimulation is carried out for a long time (months).
For obliterating atherosclerosis of the vessels of the lower extremities, training walking is also used (kinesitherapy, muscle training, walking through a walking throuth). Kinesitherapy aims to increase the distance of pain-free walking. The essence of the method is as follows: if hypoxic pain appears in the calf muscles when the patient overcomes a certain distance, he temporarily slows down his step. A few minutes after this, the patient is again able to perform movements without pain. The mechanism of the beneficial effect of training walking in occlusive-stenotic lesions of the arteries of the extremities is explained by an improvement in the utilization of oxygen by myocytes, an increase in the activity of their mitochondrial enzymes and anaerobic energy production, the transformation of white muscle fibers into red ones, stimulation of collateral circulation, and an increase in the ischemic pain threshold.
For the surgical treatment of patients with obliterating atherosclerosis of the main arteries of the lower extremities, arterial reconstructive and palliative operations are used. Reconstructive methods for restoring arterial blood flow include: endarterectomy, bypass surgery, prosthetics, X-ray endovascular reconstruction (see “Treatment of Leriche syndrome”). An indispensable condition for their implementation is good patency of the distal vascular bed.
Endarterectomy (thrombendarterectomy), as a rule, is used in patients with short (segmental) single occlusions of the main arteries 7-10 cm long. The essence of the operation is to remove the atheromatically changed intima along with the blood clots located next to it. Endarterectomy can be open, semi-closed, closed, eversion, as well as using mechanical and physical methods.
In open endarterectomy, the isolated artery is dissected longitudinally above the location of the plaque. Then, under visual control, the altered intima is peeled off from the underlying layers of the wall to the level of transition to visually unaffected areas and is cut off. The edges of the intima adjacent to the manipulation zone are fixed to the artery wall with atraumatic sutures, which is a reliable way to prevent it from wrapping and blocking the lumen of the arteries. To prevent narrowing of the endarterectomized artery, an autovenous patch is sewn into the incision.
The semi-closed endarterectomy method involves: 1) exposure of the affected segment of the arteries along its entire length; 2) dissection of arteries (longitudinal, transverse) in the projection of the distal end of the occlusion; 3) circular separation in this place of the atheromatically changed intima from the muscular membrane; 4) transverse intersection of the selected segment and passing along it in the proximal direction a special instrument - a disobliterator, mainly a ring (ring stripper), exfoliating the altered ingima; 5) opening the lumen of the artery above the area of the proximal end of the occlusion and removing the detached cylinder of the affected intima through it; 6) suturing the artery wall, if necessary with an autovenous patch.
Endarterectomy with the closed method is carried out in the same way as the semi-open one, but without isolating the artery along its entire length.
When using the eversion endarterectomy method, the artery is transversely dissected below the location of the plaque. Next, the layer of its wall, consisting of the muscular layer and adventitia, peels off from the affected intima and contracts (turns out) in the proximal direction along the upper border of the plaque. At this level, the resulting cylinder of altered intima is cut off. The inverted muscularis propria and adventitia return to their original position. The patency of the vessel is restored by applying a circular suture. It is also possible to perform reverse eversion thromboendarterectomy.
Bypass operations for obliterating atherosclerosis are performed for extended and multi-storey occlusive-stenotic lesions of the main arteries of the lower extremities. A segment of the great saphenous vein isolated from its bed, reversed and anastomosed with the artery above and below the obstacle is most often used as bypasses. Less commonly used are the human umbilical cord vein, homoarterial grafts, synthetic prostheses made of polytetrafluoroethylene, and the great saphenous vein without isolating it from the bed. The essence of the latter method is that the vein is not isolated from the subcutaneous tissue and is not reversed, but is intersected above and below the site of occlusion. Before forming an arteriovenous anastomosis, the venous valves are destroyed using valvulotomes of various designs. The presence of tributary veins capable of acting as arteriovenous fistulas after arterial blood flow is started through it is established on the basis of data from angiography, Dopplerography, palpation, etc., followed by their ligation.
The success of the shunt operation is determined, in addition to the condition of the peripheral bed, and the diameter of the shunt used, which must exceed 4-5 mm.
In case of severe damage to the arteries of the leg, obstruction of the plantar arch, in addition to the usual femoral-popliteal (tibial) autovenous shunting, additionally c. After leaf anastomosis, an arteriovenous fistula is formed, which leads to the discharge of part of the blood directly into the vein, increases the speed of blood flow through the vein and thereby reduces the likelihood of thrombosis. During surgery, a side-to-side anastomosis is first performed with the receiving artery, then a fistula is created by anastomosing the distal end of the shunt with the adjacent popliteal or tibial vein. The diameter should be 2-4 mm, i.e. 40 - 60% of the shunt diameter.
Prosthetics of the main arteries of the lower extremities for atherosclerosis is used extremely rarely.
If it is not possible to restore blood flow through the main arteries, primarily due to occlusion of the distal vascular bed, plastic surgery of the deep femoral artery is performed. At the same time, quite frequent damage to both the deep femoral artery and the popliteal and leg arteries, poor development of collaterals between them lead to unsatisfactory results of the operation.
In case of occlusion of the distal vascular bed or poor condition of the deep femoral artery, palliative surgical interventions are performed aimed at enhancing collateral circulation in the limb. These include lumbar sympathectomy, revascularizing osteotrephination, methods of P. F. Bytka, G. A. Ilizarov, microsurgical transplantation of the greater omentum to ischemic tissue of the extremities.
Lumbar sympathectomy for obliterating atherosclerosis involves extra-, transperitoneal removal of the II - III lumbar sympathetic ganglia on the affected side (Diez operation). The main mechanism of action of the operation is to eliminate the influence of the sympathetic nervous system.
When using revascularizing osteotrephination for obliterating atherosclerosis, 6-9 burr holes with a diameter of 4-6 mm are made on the medial surface of the tibia at biologically active points (as in acupuncture) in the area of a well-developed subcutaneous network of collaterals without damaging the bone marrow. In the postoperative period, subthreshold irritation at biologically active points caused by trepanation stimulates the opening of reserve collaterals. At the same time, through burr holes, unconventional intervascular connections are formed between the arteries of muscle tissue and the bone marrow. In addition, the content of bone marrow mediators—myelopeptides, which have analgesic, trophic and angioprotective properties—increases in the general bloodstream (G. A. Ilizarov, F. N. Zusmanovich, 1983).
The essence of P.F. Bytok’s method is the introduction of autologous blood through certain points on the foot and lower leg into their soft tissues (Fig. 42). Treatment is carried out for 30 days. The tissues are infiltrated twice - on the lower leg on the 1st and 14th days, on the foot on the 7th and 21st days. One session consumes 60 - 80 ml of blood for the foot, 150 - 180 ml for the lower leg. The clinical effect of the operation becomes noticeable after 2-3 months. after completion of the course of treatment and is associated with the formation of well-vascularized connective tissue in the extravasation area.
G. A. Ilizarov’s method (longitudinal compactectomy according to G. A. Illizarov) involves the formation of a longitudinal bone flake 10-16 cm long from the anterior internal surface of the tibia. 2-3 distraction wires are passed through it and attached to the Ilizarov apparatus applied to the bone. From the 8th to 9th postoperative day, the bone flake is removed daily from the tibia by 0.5 mm. The procedure is performed for 31-36 days, until the gap between the tibia and its fragments is 15-20 mm. After this, fixation of the flake continues for 45–60 days, which depends on the degree of maturity of the connective tissue. According to G. A. Illizarov, when the flake is distracted, regional stimulation of the vascular network occurs under the influence of tensile stress. At the same time, the main vessels expand, the number and caliber of small vessels of muscles, fascia and bones increase; at the site of hematoma formation, well-supplied connective tissue develops; due to increased blood supply, regenerative processes in the limb are activated.
During microsurgical transplantation of the greater omentum onto ischemic tissues of the extremities, the greater omentum is placed subfascially on the thigh, moving to the popliteal region and lower leg. The feeding vessel of the graft, usually the right gastroepiploic artery, is implanted into the common femoral artery, and the vein into the femoral vein.
The disadvantage of these methods of surgical treatment of obliterating atherosclerosis, which occurs with occlusion of the entire distal vascular bed of the lower extremities, is the long period of time required for the development of collateral circulation - from 1 to 3 months. This limits the use of such operations in the treatment of patients with critical limb ischemia of stages III - IV, who need a rapid increase in blood circulation in the limb. In such cases, arterilization of the venous system of the foot is carried out: arterilization of the superficial venous network with preliminary destruction of its valves - arterilization into the sources of the great saphenous vein, and in case of occlusion of the superficial veins - into the deep venous system. Arterilization into the origins of the great saphenous vein on the foot involves performing a bypass (reversed autovein, vein in situ, prosthesis) between the patent segment of the popliteal artery or the distal segment of the superficial femoral artery and the origins of the great saphenous vein on the foot. The arterilization of the deep venous network is based on the inclusion of the posterior tibial vein into the bloodstream using a similar technique.
If it is impossible to perform reconstructive surgery in patients with thrombotic occlusions of the arteries of the lower extremities or abdominal aorta due to atherosclerosis, systemic or local thrombolysis with well-known thrombolytic drugs (streptokinase, decase) can be used.
The greatest effect from its use is achieved: 1) with a period of occlusion not exceeding 12 months. in patients with damage to the abdominal aorta and iliac arteries, 6 months. - with the appearance of the femoral and popliteal arteries, 1 month. - renal arteries; 2) with the extent of occlusion up to 13 cm, 3) with a satisfactory condition of the distal vascular bed (the arteries of the lower leg are patent).
Systemic lysis is carried out according to the traditional scheme, local involves the introduction of a thrombolytic in a lower dosage through a catheter directly into the body of the thrombus, antegrade or retrograde, which is accompanied by activation, in contrast to systemic lysis, only of plasminogen, which is part of the structure of the thrombus.
There are several methods of local thrombolysis: 1) continuous infusion with an initial administration of a large dose, and then a maintenance dose; 2) administration of a thrombolytic drug through a catheter with multiple holes along the entire length of the occluding thrombus (pulsatile spray technique); 3) administration of a thrombolytic in a large dose while pulling the catheter along the length of the thrombus. The maximum duration of thrombolytic therapy does not exceed 48 hours. Its effectiveness is monitored angiographically or using ultrasonography.
In the postoperative period, patients continue complex conservative treatment aimed at preventing purulent and thrombotic complications of the operation. Subsequently, they must annually undergo 1-2 courses of inpatient therapy for the disease, and while on outpatient treatment, constantly take antiplatelet agents, indirect anticoagulants and other pathogenetically based drugs.
Diagnosis of atherosclerosis of the lower extremities
When you first complain about an illness, the doctor conducts a standard visual examination during which:
- Measures pressure.
- Measures waist circumference to calculate the amount of visceral fat.
- Performs palpation and auscultation of the vessels of the legs to determine the presence of a pulse in the vein under the knees and on the thigh.
- Detects the presence of muscle hypertrophy, symptoms of a dried vein bed.
- Determines skin color and condition, hair fragility, areas with necrosis or baldness.
The patient is then prescribed laboratory tests to determine the level of glucose, total cholesterol, LDL, VLDL, HDL, triglycerides, homocysteine, c-reactive protein and apoliproteins.
Tests and samples
If OASNK is suspected, a differential diagnosis method is used. It consists of excluding diseases that are inappropriate for any factors or symptoms to establish a correct diagnosis. For this purpose, the diagnosis of obliterating atherosclerosis of the arteries of the lower extremities includes several tests.
Panchenko test
To undergo the Panchenko knee test, the patient is seated on a chair. The affected leg is placed on top of the healthy one. The doctor records the time and determines the appearance of muscle pain, numbness in the foot or pins and needles in the fingers.
Goldflam's test
Carry out from a supine position. The patient raises his legs and makes several flexion-extension movements of the ankle joint. If there is no pathology and the blood supply is not impaired, then joint mobility is maintained for a long time. If after 10-20 movements the legs get tired, then OASNK is diagnosed. At this time, the doctor also observes the color of the skin of the foot: if the blood circulation is severely impaired, the skin quickly turns pale.
Sitenko-Shamova test
It consists of the following: a tight tourniquet is applied to the upper thigh for 5 minutes, compressing the artery. When the tourniquet is loosened, the time is noted. A healthy limb restores normal blood circulation in 10-12 seconds. If pathology is present, recovery takes longer.
Calculation of the shoulder-ankle index
Carry out after measuring blood pressure on the arm and ankle. The normal ratio of indicators is greater than 1. Borderline data range from 0.91 to 0.99. A mild degree of atherosclerosis is diagnosed at values from 0.71 to 0.91, average - 0.4-0.7. An index below 0.4 represents a health hazard, indicating severe damage and poor blood circulation in the limb.
Instrumental diagnostic methods
Accurate diagnosis of obliterating atherosclerosis of the arteries of the lower extremities is possible using hardware methods that make it possible to establish not only the degree of damage, but also the location of the plaques.
Hardware diagnostics
Rheography is based on measuring the level of electrical resistance of muscle tissue when pulse fluctuations change. During the session, a graphic image of the vessels is displayed on the screen, by studying which the doctor makes a conclusion about the state of the blood flow. Another method of hardware diagnostics is X-ray angiographic examination of blood vessels. Before the session, a special contrast agent is injected into the artery through a catheter, and the essence of the procedure is X-ray imaging and subsequent data processing by software. The method allows you to determine the internal state of blood vessels, the speed of blood movement, the presence and density of cholesterol plaques.
Scanning methods
Doppler ultrasound is based on the property of ultrasound waves being reflected from blood cells. The sensor is able to measure the speed of blood flow, assess the wear and tear of vessel walls and the patency of arteries, the size and density of plaques. Color duplex scanning allows you to obtain a more accurate image of blood vessels, and is used in emergency cases to clarify details. It is usually prescribed before urgent operations and in advanced stages of the disease. Duplex scanning allows you to diagnose the cause of decreased vascular patency, visualize plaques and blood clots, determine the bends of the vessel and the thickness of its wall. Triplex scanning is similar to duplex scanning, but additionally shows the tissue through which the vessel passes. And the image of the vessel changes its color depending on the speed of blood flow.
Angioscopy
Allows you to see the condition of the arteries from the inside. It is carried out by inserting an endoscopic tube with a light-sensitive optical device inside the vessel. The diameter of the tube does not exceed 2 mm, and a video camera is installed at its end. Less commonly, patients are prescribed thermography, which studies the condition of tissues based on the level of infrared radiation. The presence and extent of damage is determined by the temperature difference.
All results of tests and instrumental studies, as well as the medical history, are recorded in the medical history. Obliterating atherosclerosis and its degree are diagnosed after studying all the data.
Prevention
Lost health due to atherosclerosis is the result of your attitude towards yourself at random, therefore, already having such a disease, you must at least now be more attentive to yourself and be sure to carry out prevention. In case of OASNK, it is necessary to choose spacious, comfortable shoes to avoid calluses, bruises, avoid any injuries to the legs, and when sitting, do not cross your legs over each other, because At the same time, the vessels are pinched and the blood supply to the affected leg is disrupted. It is necessary to take walks every day; it is very good for your legs. This also includes proper nutrition with the exception of animal fats, salt, smoked meats, fried, red meat, full-fat milk, and cream.
It is necessary to normalize weight and control blood pressure - the numbers should not exceed 140/85. Reducing blood lipids will protect you from myocardial infarction; eliminating physical inactivity from your daily routine and introducing moderate physical activity will also be useful. Quitting smoking is mandatory (this alone reduces the mortality rate from 54% to 18%). It is better to avoid alcohol in any dose.
It is necessary to promptly treat any chronic diseases, control blood sugar levels, avoid stress, regularly visit a doctor for examinations, and systematically conduct courses of conservative treatment. The prognosis is determined by the presence of other forms of atherosclerosis in the vicinity: cerebral, coronary - which, of course, do not improve health.