Reasons for development
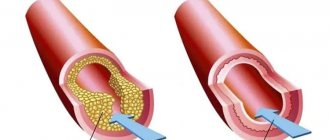
The key cause of the disease, which is called myocardial infarction, is considered to be the formation of a blood clot. Typically, a blood clot forms inside a coronary artery that is already narrowed due to atherosclerosis, a condition in which fatty deposits (or atherosclerotic plaques) accumulate along the inner walls of blood vessels.
Throughout life, fat, calcium, proteins and inflammatory cells accumulate in the arteries, forming atherosclerotic plaques. These deposits are hard on the outside but soft and crumbly on the inside. When the plaque hardens, the outer shell cracks. This is called plaque rupture. Platelets (plates in the blood that help it clot) become trapped in the area, and blood clots form around the plaque. If a blood clot blocks an artery, the heart muscle is starved of oxygen. The muscle cells soon die, causing permanent damage. This is the most common reason, but not the only one.
Slowing of blood flow in the coronary artery can occur when the heart beats very quickly or a person has low blood pressure. If oxygen demand exceeds supply, a heart attack can occur without a blood clot forming. People with atherosclerosis also often suffer from this type of heart attack. Source: Myocardial infarction. Zhmurov D.V., Parfenteva M.A., Semenova Yu.V. Colloquium-journal, 2021. p. 56-61.
In rare cases, coronary artery spasm can also cause a heart attack. During this coronary spasm, your arteries narrow or spasm, cutting off the blood supply to the heart muscle (ischemia). This can happen at rest or under stress, even if the person does not have serious coronary heart disease.
If vascular patency is not restored, there is a risk that recurrent myocardial infarction will develop over time. It will cause even more damage to the heart.
Risk factors
Most heart attacks result from atherosclerosis. The risk factors for heart attack and atherosclerosis are essentially the same:
- abnormally high levels of cholesterol in the blood (hypercholesterolemia);
- abnormally low levels of HDL (high-density lipoprotein), commonly called “good cholesterol”;
- high blood pressure (hypertension);
- diabetes;
- family history of coronary heart disease at an early age;
- smoking cigarettes, hookahs, vapes;
- obesity;
- lack of physical activity (too little exercise).
During middle age, the risk of heart attack is higher for men than for women. However, a woman's risk increases when she goes through menopause. This may be the result of a menopause-associated decrease in estrogen, a female sex hormone that may provide some protection against atherosclerosis.
Although most heart attacks are caused by atherosclerosis, there are rarer cases where heart attacks occur as a result of other diseases. These include congenital anomalies of the coronary arteries, hypercoagulability (an abnormally increased tendency to form blood clots), collagen vascular diseases such as rheumatoid arthritis or systemic lupus erythematosus (SLE or lupus), cocaine abuse, coronary artery spasm or embolus (small moving blood clot) , which enters the coronary artery and gets stuck there.
Myocardial infarction: symptoms
The nature of the symptoms that develop with each heart attack and the chances of survival are related to the location and extent of the coronary artery blockage.
The first signs of a heart attack include:
- discomfort, pressure, heaviness, tightness, squeezing, or pain in the chest, arm, or under the breastbone;
- discomfort in the back, jaw, throat, or arm;
- stomach fullness, indigestion, or a feeling of choking (may feel like heartburn);
- sweating, upset stomach, vomiting, or dizziness;
- severe weakness, restlessness, fatigue, or shortness of breath;
- fast or uneven heartbeat.
The clinical presentation may vary from person to person or from first to recurrent infarction. Source: Outcomes of Recurrent Myocardial Infarction. Shulaev A.V., Muradimova Z.R., Marapov D.I., Zakirov I.K., Mazitov M.R. Practical medicine, 2021. p. 142-144. Women are more likely to experience symptoms such as upset stomach, shortness of breath, and back or jaw pain. In some heart attacks, patients will not even notice any symptoms (a “silent” myocardial infarction). This is more common in people with diabetes.
“I feel good - pills in the toilet, and a cigarette in my teeth”
“It is important that patients understand that myocardial infarction is an ongoing process. The disease began long before the vascular accident and, unfortunately, continues after it,” explains Alexey Erlikh, Doctor of Medical Sciences, senior researcher at the Laboratory of Cardiology of the Federal Scientific Center for Physical and Chemical Medicine of the Federal Medical and Biological Agency. — Heart attack is a disease associated with two serious pathological processes: atherosclerosis and thrombosis, when atherosclerotic plaques grow in the vessels and blood clots form on these plaques. And after a heart attack, this process, unfortunately, continues.”
Experts say: there are two powerful effects on the body - non-drug and medicinal. And neither one nor the other can be neglected.
“Non-drug” recommendations are changes in lifestyle:
quit smoking and alcohol;
ensure uniform physical activity, gradually increasing it;
the “gold standard” for both healthy people and “heart attack patients” is 10,000 steps daily or 30 minutes of aerobic exercise;
eat right: complete proteins, limit animal fats and fast carbohydrates; more different vegetables, fruits, herbs, a minimum of sugar, salt, smoked, fried foods. We must try to reduce weight.
Diagnostics
Once a heart attack occurs, the patient needs prompt medical attention to open the blocked artery and reduce the damage. At the first sign of a heart attack, you need to call an ambulance. The best time to treat a heart attack is within 1-2 hours after symptoms appear. A longer wait means more damage to the heart and less chance of maximally complete recovery and rehabilitation after a myocardial infarction. Source: On the issue of overdiagnosis of myocardial infarction. Kim A.O., Kausova G.K. Bulletin of the Kazakh National Medical University, 2021. p. 28-29.
Emergency doctors will ask the person about all the symptoms and perform several tests:
- An ECG (electrocardiogram) can determine how much heart muscle has been damaged and exactly where (types of heart attack). It can also monitor heart rate and rhythm. If there are signs of damage according to the ECG, immediate hospitalization is indicated. The clinic urgently performs additional diagnostic methods.
- Blood tests . Different levels of cardiac enzymes in the blood may indicate damage to the heart muscle. These enzymes are usually found in heart cells. When these cells are damaged, their contents, including enzymes, leak into the bloodstream. By measuring the levels of these enzymes, the doctor can know the size of the heart attack and when it started. The tests can also measure troponin levels. Troponins are proteins inside heart cells that are released when the cells are damaged due to lack of blood supply to the heart.
- Echocardiography . This imaging test can be used during and after a heart attack to see how the heart is working and which areas are most damaged. An ECHO can also determine whether any parts of the heart (valves, septum, etc.) have been damaged due to ischemia.
- Cardiac catheterization . The patient may require cardiac catheterization in the early hours of a heart attack if medications do not relieve ischemia or symptoms. The catheter can provide an image of the blocked artery and help the doctor decide on treatment.
Features of making a prognosis for a heart attack
The peculiarity is that only after the acute period of the disease has passed, the doctor can give a positive prognosis. If the patient has some complications, then experts usually give a negative prognosis.
A heart attack itself is a very serious and in many cases fatal disease. There is a high probability of various complications occurring. In most cases, death occurs within the first 24 hours after the attack occurs. When more than half of the entire area of the myocardium is damaged, the heart can no longer function normally, resulting in the rapid development of cardiogenic shock and death. Even if the myocardium is damaged by 40 percent or less, the heart may not be able to cope with sudden loads, and severe complications appear, one of which is heart failure.
Myocardial infarction: treatment
Upon the arrival of doctors and after taking an ECG, treatment of a heart attack and emergency care depend on how stable the person’s condition is and his immediate risk of death. Doctors have a developed algorithm of actions.
- As soon as possible, the person is given aspirin and often other medications that help prevent unwanted blood clotting in the coronary arteries.
- The person will also be given oxygen to breathe, painkillers (usually narcotic analgesics) for chest pain, beta blockers to reduce the heart's need for oxygen, nitroglycerin to improve blood flow to the heart muscle cells, and statins to lower cholesterol. The patient may be given heparin in addition to aspirin for a stronger anticlotting effect. Emergency hospitalization to a clinic is also important.
- During the initial hospital assessment, the person will be considered for reperfusion therapy, according to clinical guidelines. The goal is to restore blood flow to the damaged heart muscle as quickly as possible to limit permanent damage. Reperfusion is best done mechanically. The patient is taken to the cardiac catheterization laboratory at the hospital. The catheter is passed through a large blood vessel (femoral) to the heart. A dye is injected to detect blockage in the coronary artery.
- The next step is percutaneous transluminal coronary angioplasty (PTCA). In PTCA, another catheter with a small deflated balloon is passed through the blockage and the balloon is inflated to clear the clot and plaque. Most balloon catheters also have a wire mesh, called a stent, on top of the balloon. After the balloon is inflated to clear the blocked artery, the stent is left in place to keep the artery open.
- In addition to aspirin, a second antiplatelet drug is prescribed. The most commonly used drugs are clopidogrel, prasugrel and ticagrelor.
- Reperfusion therapy can also be done with clot-dissolving drugs called thrombolytic agents, such as tissue plasminogen activator (tPA). This drug is used if it takes too long to transfer a patient to a hospital where angioplasty can be performed.
- While in the hospital, the patient begins to undergo the first stages of rehabilitation of patients. He receives daily medications that include aspirin, a beta blocker, an ACE inhibitor (angiotensin converting enzyme) to help the heart work more efficiently, primarily by lowering blood pressure, a statin and a second anti-clotting drug.
Complications of myocardial infarction
Each coronary artery sends blood to a different part of the heart muscle. The extent of muscle damage depends on the size of the area supplied by the blocked artery and the amount of time between the attack and treatment.
The heart muscle begins to repair itself soon after a heart attack. This takes about 8 weeks. As with skin wounds, a scar forms on the damaged area. But new scar tissue moves differently than healthy tissue. Thus, the heart cannot pump as much blood after a heart attack and heart failure is a complication. The extent to which this ability to pump blood is impaired depends on the size and location of the scar.
In addition, some coronary arteries supply blood to areas of the heart that regulate the heartbeat, so a heart attack sometimes causes potentially fatal abnormal heartbeats called cardiac arrhythmiasSource: Complications of Myocardial Infarction in the Elderly. Khalmukhamedov B.T. Eurasian Journal of Cardiology, 2021. p. 29-30.
Classification of the disease
There is no one specific classification at the moment. Therefore, experts use different concepts, it all depends on different factors. Here are the main classifications used by cardiologists:
- According to the size of the lesion. Here, large-focal and small-focal infarction are distinguished. The first is much more common - in about 80 percent of all people suffering from the disease.
- Depending on the depth of necrosis. For example, transmural or intramural myocardium. There are four varieties in total.
- According to the changes shown by the electrocardiogram. There are two types: heart disease, which is accompanied by the appearance of a Q wave, and an illness in which this wave is absent.
- According to topography. It all depends on which branch of the coronary artery is affected as a result of a heart attack.
- By the brevity of occurrence. There are only three types: primary, recurrent and repeated. A recurrent heart attack occurs less than 2 months after the appearance of the primary one, but a repeat one occurs after 8 or more weeks.
- By complication. Some ailments may be complicated by some concomitant diseases, while others may not.
- According to the presence and type of pain. In most cases, the first sign and symptom of a heart attack is severe chest pain. This is called the typical form. There are also atypical pain manifestations. For example, a person may complain of severe pain in the jaw, shoulder blade, or arm. The appearance of edema, arrhythmia and other unpleasant factors is also possible.
- According to the dynamics. Covers four periods (discussed above): from the acute to the post-infarction period, when scars form.
Prevention
- Check your blood pressure at home. High blood pressure can lead to a heart attack. Sit and rest for 5 minutes before taking your readings. Measure your blood pressure at least 2 times a day at the same time, for example, in the morning and evening.
- Quit smoking. Nicotine and other chemicals in cigarettes and cigars can cause damage to the lungs and heart. Electronic cigarettes or smokeless tobacco also contain nicotine and are no less dangerous.
- Eat a heart-healthy diet. A heart-healthy diet is one that is low in saturated, unhealthy fats and sodium (salt). It helps reduce the risk of heart disease and stroke. Limit the amount of fat you consume to 25-35% of your total daily calories. Your doctor may recommend an eating plan that lowers your cholesterol and blood pressure.
- Limit your sodium (salt) intake. Too much sodium can affect fluid balance. Do the exercises. Ask your doctor about the exercise plan that's best for you. Exercise strengthens the heart, lowers blood pressure and helps prevent heart attacks. The goal is 30 to 60 minutes of activity almost every day.
- Maintain a healthy weight. Ask your doctor how much you should weigh. He can help you create a safe weight loss plan if you are overweight.
- Manage stress. Stress can increase your risk of heart attack. Learn ways to control stress, such as relaxation, deep breathing and music. Talk to someone about what's upsetting youSource: Innovative Methods to Prevent Myocardial Infarction. Volodkin A.A. , Zaikov G.E. NBI-technologies, 2013. p. 103-106.
Sources:
- Myocardial infarction. Zhmurov D.V., Parfenteva M.A., Semenova Yu.V. Colloquium-journal, 2021. p. 56-61
- Outcomes of recurrent myocardial infarction. Shulaev A.V., Muradimova Z.R., Marapov D.I., Zakirov I.K., Mazitov M.R. Practical medicine, 2021. p. 142-144
- Complications of myocardial infarction in the elderly. Khalmukhamedov B.T. Eurasian Journal of Cardiology, 2021. p. 29-30
- On the issue of overdiagnosis of myocardial infarction. Kim A.O., Kausova G.K. Bulletin of the Kazakh National Medical University, 2018. p. 28-29
- Innovative methods for preventing myocardial infarction. Volodkin A.A. , Zaikov G.E. NBI-technologies, 2013. p. 103-106
Heart attack and stroke: signs, emergency care, prevention
Myocardial infarction is a disease in which, due to blockage of the coronary artery, the full blood supply to an area of the heart muscle (myocardium) suddenly and abruptly stops, which leads to a severe lack of oxygen (ischemia), nutrients and death of myocardial cells. This area can no longer take part in heart contractions, so the heart cannot provide blood flow to the body. All organs and tissues begin to experience oxygen starvation, which leads to disruption of their function. The main cause of heart attack is elevated levels of cholesterol and certain lipids in the blood.
Typical manifestations of myocardial infarction are a feeling of severe pressure or pain behind the sternum, or slightly to the left or right of it. The pain is most often squeezing, pressing, tearing (feeling of a stake in the chest), sometimes burning. Irradiation of pain to the left shoulder girdle, shoulder, arm, less often to the neck and lower jaw, sometimes to the right half of the shoulder girdle is typical. Occasionally, the pain is localized in the epigastric region. Unlike angina, pain during myocardial infarction lasts more than half an hour, usually several hours. Nitroglycerin taken brings only minor and short-term relief. Severe weakness and cold sweat are often noted. Often in the acute stage of myocardial infarction, patients experience nausea, vomiting, hiccups, and bloating, which are of a reflex nature. In some cases, myocardial infarction is practically asymptomatic.
During the period of pain, the patient's face has a suffering appearance, the skin is usually pale, sometimes with a cyanotic tint. Breathing is rapid. Blood pressure may rise when pain occurs, but soon drops to an unusually low level for the patient. The pulse is frequent, heart sounds are weakened. In most patients, various cardiac arrhythmias can be detected.
If you or someone else suddenly has the above characteristic signs of a heart attack, even with weak or moderate intensity, which last more than 5 minutes, do not hesitate, immediately call an ambulance team. Do not wait more than 10 minutes - in such a situation it is life-threatening.
The recovery period after a myocardial infarction lasts 4-6 weeks. It occurs differently in different patients. Most often, during this period, patients remain able to work, but they sometimes experience angina attacks. In rare cases, the course of the post-infarction period is interrupted by the onset of a second infarction.
The results of large-scale international studies, in particular the INTERHEART study, showed that the following factors have a decisive influence on the risk of developing myocardial infarction: dyslipidemia, smoking, hypertension, abdominal obesity, psychosocial factors (stress, social isolation, depression), diabetes mellitus, reduce the risk : eating enough vegetables and fruits, regular physical activity.
Emergency self-help and mutual assistance measures in case of a heart attack (myocardial infarction).
In our country, up to 80% of deaths occur outside of medical organizations - at home, at work, in the country, in public and other places. Most of them occur suddenly or by the mechanism of sudden death. However, with knowledge of simple first aid techniques on the part of people surrounding a person who finds himself in such a critical condition, as well as everyone’s knowledge of first self-help measures, can in most cases save the patient’s life.
Characteristic signs (symptoms) of a heart attack (myocardial infarction)
• sudden (paroxysmal) pressing, squeezing, burning, aching pain in the chest (behind the sternum) lasting more than 5 minutes;
• similar pains are often observed in the left shoulder (forearm), left shoulder blade, left half of the neck and lower jaw, both shoulders, both arms, the lower part of the sternum along with the upper abdomen;
• lack of air, shortness of breath, severe weakness, cold sweat, nausea often occur together and sometimes follow or precede discomfort/pain in the chest
• often these manifestations of the disease develop against the background of physical or psycho-emotional stress, but more often with some interval after them.
Algorithm of urgent actions:
• Call an emergency medical team.
• Sit (preferably in a chair with armrests) or lie in bed with the head of the bed raised, take 0.25 g of acetylsalicylic acid (aspirin) (chew the tablet, swallow) and 0.5 mg of nitroglycerin (put the tablet/capsule under the tongue, first bite the capsule , do not swallow); free your neck and provide fresh air (open the vents or windows).
• If after 5-7 min. After taking acetylsalicylic acid (aspirin) and nitroglycerin, pain persists, you need to take nitroglycerin a second time.
• If pain persists 10 minutes after taking the second dose of nitroglycerin, it is necessary to take nitroglycerin a third time.
• If after the first or subsequent doses of nitroglycerin there is severe weakness, sweating, shortness of breath, you need to lie down, raise your legs (on a bolster, etc.), drink 1 glass of water and then, as with a severe headache, do not take nitroglycerin.
• If the patient has previously taken cholesterol-lowering medications, give the patient his usual daily dose and take the drug with you to the hospital.
Attention! A patient with a heart attack is strictly forbidden to get up, walk, smoke or eat until the doctor’s special permission;
You should not take aspirin (acetylsalicylic acid) if you are intolerant to it (allergic reactions), as well as with obvious or worsening peptic ulcers of the stomach and duodenum;
Nitroglycerin should not be taken if there is severe weakness, sweating, or if there is severe headache, dizziness, or acute impairment of vision, speech, or coordination of movements.
Prevention of myocardial infarction.
As for the prevention of atherosclerosis, everyone who has become familiar with the factors contributing to its occurrence knows what to do. The one who sharply reduces the consumption of animal fats and develops a rational attitude to nutrition will do the right thing. You should eat low-fat cottage cheese and low-fat kefir. More fiber-rich vegetables should be included in the menu - raw and sauerkraut, beets, carrots (at least 500 g per day). Fiber helps remove excess cholesterol from the body. When the first cases of increased pressure are detected, for which you need to regularly, at least once every one to two months, measure blood pressure and, by contacting a doctor, take the necessary measures, it is quite possible to stop the development of hypertension (blood pressure should not be higher than 140/90 mm Hg. Art.). If elevated cholesterol levels are determined, then by resorting to dietary and drug treatment, the progression of atherosclerosis can be delayed (the maximum permissible level of cholesterol in the blood is 5 mmol/l). The most important preventive measure is to stop smoking. Harmful substances in cigarette smoke contribute to the development and progression of atherosclerosis, cause fluctuations in blood pressure, thicken the blood and provoke thrombosis. The danger is posed by so-called passive smoking, so it is important not only to quit smoking, but also not to be in areas where smoking is allowed and in the company of smokers. Smoking significantly reduces the effect of physical training, so the desire to achieve the maximum effect from exercise and lead an active lifestyle is another reason to stop smoking.
In order to timely identify initial disturbances in the activity of the cardiovascular system and, if necessary, prescribe optimal drug treatment that can prevent the development of myocardial infarction, experts strongly advise regular medical examinations or preventive medical examinations at the clinic at the place of residence.
Finally, it is important to remember that only a doctor prescribes treatment for a heart attack, and the patient and his relatives strictly follow the instructions. Self-medication of a heart attack, no matter how easy it may be, is unacceptable!
Stroke: causes, symptoms, prevention.
In the modern world, people suffer from such a disease as “stroke” more often than from “myocardial infarction”. Residents of large cities are most susceptible to this disease, where life is full of stress and anxiety, and there is also an unfavorable environmental situation. Stroke accounts for approximately 6 million deaths per year worldwide and is second only to coronary heart disease as a cause of death.
A stroke is a terrible blow, which often divides not only the life of the patient, but also the life of his family into two parts: “Before” and “After”. Everything can change overnight: an active, active person can become a helpless disabled person in need of constant outside help, caring for which places a heavy burden on his loved ones, creating considerable socio-economic difficulties for society. What kind of life are people forced to lead after suffering a severe stroke? This is a real genuine tragedy and tears invisible to the world, since for many of them even leaving the apartment is an insoluble problem, and it is not so rare that the disease is bedridden, making the patient completely dependent on others.
A stroke is an acute disorder of cerebral circulation, leading to damage to the brain substance and disruption of its functions. There are two types of this disease: ischemic stroke and hemorrhagic stroke. Ischemic stroke occurs when the lumen of a vessel is blocked by a thrombus or embolus. The cause of a hemorrhagic stroke is a rupture of the vessel wall and blood entering the brain.
Many risk factors for stroke are common to other cardiovascular diseases. They are divided into two large groups: internal - high blood pressure, age, family history (stroke, myocardial infarction, hypertension in close relatives), high blood cholesterol, obesity; external – emotional stress, sedentary lifestyle, bad habits, environmental features. In addition, stroke has risk factors unique to it: initial manifestations of insufficient blood supply to the brain, dyscirculatory encephalopathy, transient cerebrovascular accidents, and previous strokes.
The onset of a stroke can vary. Hemorrhagic stroke occurs suddenly. Subsequently, patients can even indicate at what hour and even minute they began to experience symptoms of the disease: severe headache, vomiting, dizziness, weakness, malaise. There may be a deterioration in a person’s orientation in the surrounding space, difficulty speaking, loss of consciousness, and the development of paralysis. With ischemic stroke, the onset may be slow. Often patients note increasing sensations of weakness in one half of the body, a gradual deterioration in speech, swallowing, facial distortion, and unsteady gait.
When the first such signs appear, the most correct thing is to immediately call an ambulance and hospitalize the patient in the neurological department. If a person’s stroke has developed acutely, with loss of consciousness and signs of paralysis, before the ambulance arrives, the patient must be turned on his side and a pillow placed under his head (if this happened at home); rolled up clothes or a bag (if this happened outside the home). To make breathing easier, unfasten your collar and, holding your head with your hands, constantly wipe away the foam with a handkerchief so that it does not get into your respiratory tract. To prevent the patient from biting his tongue, a comb or stick wrapped in a scarf can be inserted between the teeth. You cannot hold your arms and legs with force, trying to unclench your cramped fingers, much less lean on the patient with your whole body. This may make the seizure worse. The patient's arms and legs should only be held lightly so that he does not injure himself and others. And no ammonia! It may cause respiratory arrest. You cannot move a patient during an attack. If the patient’s pulse cannot be felt, the heart has stopped, and breathing has stopped, an indirect cardiac massage and mouth-to-mouth artificial respiration must be performed. Everything else is the task of the ambulance team.
Stroke prevention is based on the basic principles of a healthy lifestyle.
· Know and control your blood pressure - it should not be more than 140/90 mmHg.
· Do not start smoking or stop smoking as soon as possible.
· Add as little salt as possible to your food and avoid canned and processed foods that contain it in excess.
· Control your blood cholesterol levels – the maximum allowable level is 5 mmol/l.
· Follow the basic principles of a healthy diet - eat more vegetables and fruits (at least 500 g per day), avoid added sugar and saturated animal fat.
· Don't drink alcohol. The risk of stroke is highest in the first hours after drinking alcohol.
· Exercise regularly. Even moderate physical activity (walking outdoors for 30 minutes a day) reduces the risk of developing cardiovascular diseases, including stroke.
Preventative medical examinations and consultations that you can undergo:
— in a clinic at your place of residence, where you can undergo medical examination or in-depth preventive examination;
— at the Health Center (in Krasnodar at Tramvaynaya str., 5), where your blood pressure will be measured, your blood glucose and cholesterol levels will be determined, and your body mass index will be calculated. Knowing your risk for developing heart disease can help you develop a specific action plan to improve your heart health.