Description of drugs in Lesson No. 15
Description of drugs in Pathological Anatomy in Lesson No. 15
(This is an indicative description, not a cathedral one, some drugs may be missing, as is the description of previous years)
- LESSON No. 1 5
coronary heart disease
ELECTROGRAM Acute ischemic myocardial dystrophy (demonstration).
Mitochondria are swollen, their cristae are destroyed. Glycogen granules are not detected.
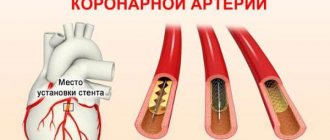
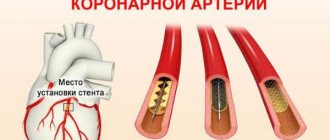
MICROPREPARATION No. 110 Atherosclerosis and thrombosis of the coronary artery of the heart.
The lumen of the coronary artery is narrowed due to an atherosclerotic plaque, in the center of which fatty protein masses, cholesterol crystals and lime deposits are visible (stage of atherocalcinosis). The plaque cover is represented by hyalinized connective tissue. The lumen is obstructed by thrombotic masses consisting of fibrin, leukocytes, and erythrocytes.
MICROPREPARATION No. 111 Myocardial infarction (necrotic stage). Demonstration, see earlier
MICROPREPARATION No. 111A Myocardial infarction. Organization stage.
A zone of necrosis surrounded by a demarcation shaft (granulation tissue with a large number of vessels). An area of necrosis with lysis of nuclei and clumpy disintegration of the cytoplasm of cardiomyocytes, surrounded by a zone of demarcation inflammation, in which full-blooded vessels, hemorrhages, and accumulations of leukocytes are identified.
MICROPREPARATION No. 215 Disappearance of glycogen from the ischemic zone of cardiomyocytes.
The absence of glycogen in the focus of necrosis is expressed by the pale color of the stained preparation. Cardiomyocyte nuclei are lysed. Thick red fibers are the remains of necrotic tissue. Around them is bluish tissue with many nuclei - granulation tissue in the form of a mesh (PMN, fibroblasts, vessels, connective fibers, BM fragments).
MICROPREPARATION No. 45 Large focal cardiosclerosis.
Heme-Eoz staining (demonstration). Staining with picrofuchsin according to Van Gieson: an irregularly shaped area of cardiosclerosis is red. The focus of sclerosis is irregular in shape, with pronounced hypertrophy of cardiomyocytes along the periphery. When stained for connective tissue (according to Van Gieson), the scar is stained red, cardiomyocytes - yellow.
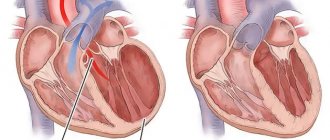
MACROPROOF Transmural myocardial infarction with cardiac rupture.
In the anterior wall of the left ventricle, a focus of necrosis is visible, irregular in shape, whitish-yellowish in color, flabby consistency, with a hemorrhagic rim. On the endocardial side – thrombotic masses attached to the endocardium, on the pericardial side – fibrous deposits. In the area of necrosis there is a slit-like hole whose walls are saturated with blood. In the pericardial cavity there is blood and thrombotic masses.
MACROPROOF
Subendocardial myocardial infarction with mural thrombus.
A focus of necrosis with a dark red rim is visible in the left ventricle. In the area of projection of necrosis on the endocardium, dense, dry, crumbling masses of gray-red color (thrombotic masses) are visible.
MACROPROOF Large focal cardiosclerosis.
- the heart is enlarged in size and weight
- in the area of the left ventricle, an irregularly shaped focus is determined, represented by dense whitish connective tissue.
MACRO PREPARATION
Chronic cardiac aneurysm
- the heart is enlarged in size
— the wall of the left ventricle in the apical region is thinned, whitish, represented by scar connective tissue, and bulges.
— the myocardium around the bulge is hypertrophied
- the aneurysm cavity is filled with crumbling, dense, dry gray-red masses (thrombotic masses) associated with the aneurysm wall
Myocardial infarction
Diabetes
Atherosclerosis
6615 16 February
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Myocardial infarction: causes, symptoms, diagnosis and treatment methods.
Definition
Myocardial infarction (MI) is the necrosis of an area of the heart muscle due to insufficient blood supply with the development of a characteristic clinical picture.
Causes of myocardial infarction
The heart is a hollow muscular organ shaped like a cone. The walls of the heart consist of three layers. The inner layer - the endocardium - lines the cavities of the heart from the inside, and its outgrowths form the heart valves. The middle layer, the myocardium, consists of cardiac muscle tissue. The outer layer is the pericardium. The human heart has four chambers: two atria and two ventricles. The right atrium receives blood from the tissues of the heart itself and all parts of the body (through the superior and inferior vena cava). Four pulmonary veins flow into the left atrium, carrying arterial blood from the lungs. The pulmonary trunk emerges from the right ventricle, through which venous blood enters the lungs. The aorta emerges from the left ventricle, carrying arterial blood to the vessels of the systemic circulation. Oxygen is delivered to the myocardium of the heart through the coronary arteries.
The heart is very sensitive to lack of blood supply (oxygen deficiency). In the case of blockage of a large coronary artery and in the absence of effective alternative blood circulation through other vessels, within 30 minutes the death of cardiomyocytes (muscle cells of the heart) begins in the affected area.
Poor circulation due to atherosclerotic lesions of the coronary arteries in 97-98% of cases is of primary importance in the occurrence of myocardial infarction.
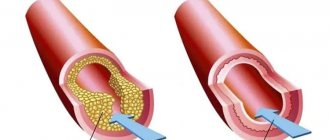
Atherosclerosis can affect either one coronary artery or all three. The degree and extent of narrowing of the artery can vary. When blood pressure increases, the sclerotic inner layer of the vessel (endothelium) is easily damaged, blood penetrates into the plaque, the blood clotting process is activated and a blood clot is formed, which can partially or completely block the vessel.
Where a blood clot can form:
- at the site of rupture of a vulnerable (unstable) atherosclerotic plaque;
- on a defect (erosion) of the endothelium of the coronary artery, not necessarily localized on the surface of the atherosclerotic plaque;
- at the site of hemodynamically insignificant narrowing of the coronary artery.
Coronary artery thrombosis occurs with complete or incomplete parietal occlusion. A thrombus located proximally (closer to the center) in the coronary artery tends to be transported with the blood flow more distally (closer to the vessel wall) and lead to the formation of small foci of necrosis and/or contribute to the expansion of the main area of necrosis.
Great importance in the development of myocardial infarction is attached to the development of spasm of the coronary arteries both with atherosclerosis and with unchanged vessels.
Developing myocardial necrosis can be of various sizes, and necrosis passing through all layers of the heart (transmural) can cause myocardial rupture.
The formation of foci of necrosis in the myocardium is accompanied by changes in the size, shape and thickness of the heart wall, and the remaining myocardium experiences increased stress and undergoes hypertrophy with an increase in volume and mass.
Concomitant conditions such as anemia, inflammation, infection, fever, metabolic or endocrine disorders (in particular, hyperthyroidism) can provoke or aggravate myocardial ischemia.
Risk factors for developing myocardial infarction include:
- hyperlipidemia (violation of the normal ratio of blood lipids);
- smoking,
- diabetes,
- arterial hypertension,
- abdominal obesity,
- psychosocial reasons (stress, depression, etc.),
- low physical activity,
- unbalanced diet and alcohol consumption.
Recurrent myocardial infarction occurs within 28 days of the initial myocardial infarction.
If myocardial infarction develops at a later date, they speak of recurrent myocardial infarction. Classification of myocardial infarction
I. Acute myocardial infarction.
- Acute transmural infarction of the anterior myocardial wall.
- Acute transmural infarction of the lower myocardial wall.
- Acute transmural myocardial infarction of other specified locations.
- Acute transmural myocardial infarction of unspecified localization.
- Acute myocardial infarction, unspecified.
II. Repeated myocardial infarction.
- Repeated infarction of the anterior myocardial wall.
- Repeated infarction of the lower myocardial wall.
- Repeated myocardial infarction of another specified location.
- Repeated myocardial infarction of unspecified localization.
III. Some current complications of acute myocardial infarction.
- Hemopericardium.
- Atrial septal defect.
- Ventricular septal defect.
- Rupture of the heart wall without hemopericardium.
- Rupture of the tendinous chord.
- Rupture of the papillary muscle.
- Thrombosis of the atrium, atrial appendage and ventricle of the heart.
- Other current complications of acute myocardial infarction.
IV. Other forms of acute coronary heart disease.
- Coronary thrombosis not leading to myocardial infarction.
- Dressler's syndrome is post-infarction sclerosis.
- Other forms of acute coronary heart disease.
- Acute coronary heart disease, unspecified.
V. Previous myocardial infarction.
Symptoms of myocardial infarction
During myocardial infarction, as a result of circulatory disorders, metabolic products accumulate in the affected area of the heart, which irritate the receptors of the myocardium and coronary vessels, which is manifested by acute pain. A painful attack leads to the release of adrenaline and norepinephrine from the adrenal cortex.
Pain in the typical course of myocardial infarction is its main symptom. It arises behind the sternum, sometimes it can radiate to the left arm, left shoulder, throat, lower jaw, and to the epigastric region.
In intensity and duration, such pain significantly exceeds a regular angina attack. The pain is not relieved by taking nitroglycerin. The duration of the pain syndrome can vary - from 1 hour to several days. Sometimes myocardial infarction is accompanied by severe weakness, dizziness, headache, vomiting, and loss of consciousness. The patient looks pale, lips turn blue, and sweating occurs.
On the first day of myocardial infarction, tachycardia (rapid heartbeat), rhythm disturbance, and temperature rise to 37-38℃ may be recorded.
In 30% of cases, myocardial infarction in the first hours of its development may manifest itself atypically.
The following clinical options are distinguished:
- asthmatic - occurs as an attack of bronchial asthma (there is shortness of breath, difficulty breathing, a feeling of lack of air);
- gastralgic - characterized by pain in the stomach spreading to the retrosternal space, there may be belching, hiccups, nausea, repeated vomiting, bloating;
- arrhythmic - life-threatening heart rhythm disturbances occur;
- cerebral – characterized by impaired cerebral circulation (nausea, dizziness, impaired consciousness with the development of fainting are observed);
- asymptomatic - myocardial infarction without a typical pain attack. Due to non-compliance with bed rest and lack of proper treatment, the course is unfavorable.
Diagnosis of myocardial infarction
There are clear criteria for diagnosing myocardial infarction:
- clinical picture of myocardial infarction;
- picture of myocardial infarction according to ECG data;
- the presence of new areas of the myocardium with reduced blood circulation or impaired myocardial contractility according to instrumental studies;
- detection of coronary artery thrombosis according to angiography.
To confirm the diagnosis, the following laboratory tests are performed:
- determination of the level of biochemical markers of cardiomyocyte damage in the blood;