General information about angina
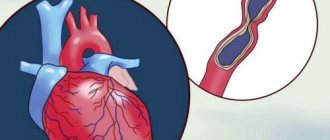
An attack of angina develops when there is insufficient oxygen supply to the heart muscle cells. This occurs when the coronary vessels narrow and the myocardial oxygen demand increases. The attack can be triggered by physical activity, emotional stress, or going out into the cold. The pain goes away within a few minutes at rest or after taking nitroglycerin.
Under conditions of oxygen starvation, cells cannot efficiently process glucose into energy. Metabolic byproducts accumulate and “acidify” the tissues, causing severe pain. If blood flow is not restored in time, the myocardium dies and a heart attack develops.
Angina pectoris (angina pectoris) - symptoms and treatment
After collecting complaints, anamnesis of life and illness, and examination, additional laboratory and instrumental examinations are prescribed.
Laboratory tests are mainly aimed at diagnosing dyslipidemia, which contributes to the formation of atherosclerotic plaques. For this purpose, a blood lipid spectrum analysis is prescribed, which includes total cholesterol and its fractions.
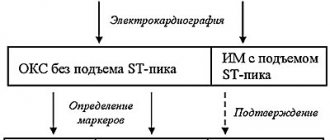
Instrumental methods primarily include electrocardiogram (ECG) . Many patients go to the cardiologist with the question “is everything normal with my heart” with only one ECG film. But, unfortunately, these indicators are of informative value only during an attack. In most cases, it is impossible to determine angina pectoris from one ECG film taken at rest, since it can only show rhythm disturbances, hypertrophy (enlargement) of various parts of the heart, conduction disturbances, or the presence of a previous myocardial infarction.
There is also an ultrasound examination of the heart , which shows its structure and can reveal possible abnormalities. Echocardiography is intended to determine the size of the heart and its chambers, the presence of valve defects (stenosis and insufficiency), neoplasms and previous infarction. But this study, like an ECG, is not informative enough if it was carried out outside an attack of angina, at rest.
Holter ECG monitoring (outpatient monitoring) is much more informative than the above studies. It is advisable to perform it in order to identify signs of myocardial ischemia during daily activities. To do this, the patient walks, eats and sleeps with the device attached to it for about a day, i.e., performs normal daily physical activity. When an attack occurs, the person being examined records the incident in a diary and then informs the doctor about when and under what conditions the symptoms arose. The sensitivity of this method in diagnosing coronary heart disease is 44-81%.
Since angina attacks practically do not occur at rest, there are examination methods using physical activity. By analogy with an electrocardiogram, a bicycle ergometry and treadmill test : an ECG is taken while the patient performs physical activity on a bicycle or treadmill. The sensitivity of this method is approximately 68%.
A more sensitive method is stress echocardiography - this is the same ultrasound examination of the heart, only performed after physical activity. As your heart rate increases during running, your myocardium consumes more oxygen and nutrients. When a vessel narrows, a sufficient amount does not enter the muscle, resulting in an attack of chest pain and disturbances in contraction. As a result, hypokinesia develops, which can be seen with ultrasound. This study has greater sensitivity (80-85%) and specificity (84-86%)
If it is impossible to perform an ECG and EchoCG during exercise, you can use transesophageal electrical pacing (TEES) or pharmacological tests . These methods are based on increasing the myocardial oxygen demand by increasing heart rate without significantly changing blood pressure.
There are also two less common research methods: stress myocardial perfusion scintigraphy and multislice cardiac computed tomography.
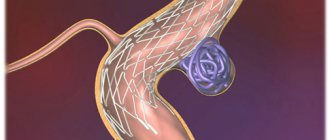
The main method for assessing the condition of the arteries, in which vessel narrowing can be visually recognized, is coronary angiography (CAG) - a radiopaque examination method that reliably determines the location and degree of narrowing of the arteries, as well as the type of blood supply, signs of thrombosis, ulceration, calcification and spasm of the coronary artery.
According to the timing of completion, this examination is divided into emergency (within 6 hours), urgent (within 6-12 hours) and planned.
Emergency coronary angiography is performed in case of unstable angina or myocardial infarction, when every minute is important.
Indications for planned coronary angiography include:
- objective signs of myocardial ischemia;
- transient ischemic changes detected during an ECG at rest or during 24-hour ECG monitoring;
- positive exercise test with bicycle ergometry, treadmill test, TES, stress echocardiography or myocardial scintigraphy;
- the occurrence of attacks of angina pectoris II-IV FC or angina pectoris at rest;
- condition of early post-infarction angina;
- life history of dangerous ventricular arrhythmias with a high risk of clinical death;
- planning surgery on the heart valve apparatus in people over 40 years of age;
- carrying out differential diagnosis with non-coronary myocardial diseases (including atypical pain syndrome);
- social indications in the presence of minimal and unclear signs of myocardial ischemia, provided that the patient’s profession is associated with a risk to the lives of other people (pilots, drivers), combat duty, etc.;
- undergone heart transplantation (the study is carried out every year, sometimes in combination with intravascular ultrasound).
There are currently no absolute contraindications for prescribing CAG.
An intermediate place is occupied by emergency coronary angiography. It is carried out in the event of a deterioration in the condition of a patient who is being treated in a hospital due to the progression of angina pectoris, when attacks of rest angina pectoris occur, there is no effect from maximum therapy, as well as in case of deterioration in condition after endovascular surgery or coronary artery bypass grafting.[1][10]
Classification of angina pectoris
Depending on the relationship between attacks and physical activity, angina pectoris is classified as exertional or resting. The latter can occur without the influence of provoking factors, so it is more difficult to control.
Angina pectoris can be divided into two types: stable and progressive. In the first case, the frequency and strength of attacks depends on the amount of physical activity; they are easily eliminated with the help of drug therapy. Progressive angina pectoris practically cannot be corrected with pharmaceutical drugs; the frequency of attacks increases over time.
The following functional classes of stable angina are distinguished:
- Pain appears only with intense or prolonged physical activity.
- The onset of an attack when walking more than 200 m or climbing more than one flight of stairs at a normal pace. With severe emotional stress.
- Pain when walking less than 200 meters or climbing one flight of stairs at a leisurely pace.
- Seizures occur with minor physical exertion or at rest.
There is Prinzmetal's angina or spontaneous (special, vasospastic) angina - caused by a sudden spasm of the coronary arteries. Attacks develop only at rest, at night or early in the morning.
What is angina?
In Russia, the classification given in the Clinical Guidelines of the Ministry of Health for Coronary Heart Disease of 2021 has been adopted. According to this classification, angina occurs:
- voltage, stable, indicating functional class (FC);
- vasospastic (other names - spontaneous, variant, Prinzmetal's angina);
- microvascular.
In the International Classification of Diseases, 10th revision (ICD-10), in addition to the above-mentioned options, there is also unstable angina, which can be either new or progressive. This type is usually mentioned in cases of progression of coronary insufficiency. The greater the degree of stenosis of the coronary arteries, the more severe the attacks will be
Risk factors for developing angina
The following factors lead to narrowing of the coronary vessels and insufficient blood supply to the myocardium:
- atherosclerosis - deposition of cholesterol plaques in the walls of blood vessels;
- hypotension ー low blood pressure;
- coronary artery thrombosis;
- age-related changes in blood vessels.
In the vast majority of cases, angina is caused by atherosclerotic lesions of the coronary arteries. It develops due to disturbances in the metabolism of cholesterol and other lipids: excess animal fats in the diet, lack of plant foods. Therefore, proper nutrition is the basis for successful prevention of angina pectoris.
Nicotine also constricts blood vessels, so smokers develop angina more often.
The risk group for the development of angina pectoris includes:
- people over 55 years of age;
- men;
- smokers;
- people who abuse alcohol and drugs;
- people with pathologies of the cardiovascular system (heart defects, heart failure);
- with pathologies of the respiratory system (bronchial asthma, chronic obstructive diseases);
- overweight.
All these factors increase the risk of developing atherosclerosis, cardiac ischemia and angina. Most of them can be eliminated through lifestyle changes.
How to distinguish the types of angina from each other
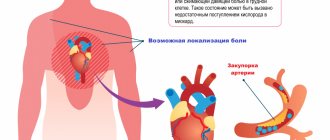
The main symptom of any type of this condition is pressing, squeezing pain in the left side of the chest, which can “radiate” to the left side of the face, neck, shoulder or shoulder blade.
Stable exertional angina
An attack of pain in the heart that occurs as a result of a decrease in arterial blood flow to the myocardium during exercise or stress. A decrease in blood supply to the heart muscle leads to a sharp decrease in the amount of oxygen supplied to the heart, which causes pain.
Signs of stable angina pectoris
- An attack is triggered by physical or emotional stress.
- Duration - from two to five minutes.
- The pain goes away after the action of the factor that caused it ceases or after taking nitrates.
Sometimes atypical manifestations are possible - shortness of breath (increased breathing rate), a feeling of suffocation, a burning sensation or heat in the chest.
The severity depends on the functional class (FC):
- 1st FC - attacks occur only with excessive stress;
- 2nd FC - attacks occur during normal exertion: fast walking, climbing stairs (more than two flights), after a heavy meal, stress;
- 3rd FC - attacks occur with minor exertion: walking at an average pace, climbing 1-2 flights of stairs;
- 4th FC - attacks occur at rest.
New or acute angina
After the first attack occurs, and up to three months after it, they speak of new-onset angina. During this period, the doctor draws conclusions about the severity of the pathology (determines the functional class) and the prognosis - the possibility of transition to unstable angina. In an acute attack, symptoms can range from mild to severe.
Unstable angina
Progressive exertional angina, or unstable angina, is said to occur when:
- the number of attacks increases;
- attacks appear at rest or after a heavy meal;
- the duration of attacks increases (up to 15-20 minutes or more);
- response to nitroglycerin decreases.
Progressive angina may precede myocardial infarction.
Vasospastic or variant angina
This type is spoken of when an attack occurs for no apparent reason - when it cannot be associated with the action of provoking factors. The cause of myocardial ischemia is a sudden spasm of the coronary arteries. More often, attacks of variant (vasospastic) angina occur in older women and occur at night or in the morning. Taking nitroglycerin is ineffective.
Microvascular angina
The clinical picture is no different from exertional angina. This diagnosis is made only after functional and instrumental research methods - echocardiography (ultrasound of the heart), coronary angiography or CT angiography. Based on the results of these studies, one can judge the condition of the coronary vessels. The main difference between microvascular angina and other types is the absence of damage to the coronary arteries.
Giving up bad habits, dosed physical activity and other prevention methods help prevent or delay the onset of any type of angina. Once diagnosed, angina requires treatment regardless of type
Diagnosis of angina pectoris
Angina pectoris has a fairly typical clinical picture, so it will not be difficult for a therapist and cardiologist with experience to recognize it. To find out the cause of the attacks and determine possible treatment tactics, specialists at the Paracelsus Medical Center recommend undergoing the following examination:
- general and biochemical blood test (cholesterol and other lipid levels);
- ECG at rest and during exercise;
- echocardiography (Echo-CG);
- coronary angiography ー examination of the heart vessels using a contrast agent;
- Holter monitoring - recording of electrical impulses of the heart for 24 hours (the patient adheres to his usual routine).
Forecast and prevention of angina pectoris
The basis for preventing angina pectoris is proper nutrition and exercise. The diet should consist of proteins, vegetable fats, and complex carbohydrates. The consumption of alcohol and trans fats (fast food) should be avoided. Give preference to white meat, fish and seafood.
Regular physical activity should be present in the life of every person, this could be swimming, team sports, fitness, running or just walking. Its intensity is determined by the person’s health status; if you have chronic diseases, you should consult your doctor about the types of physical activity acceptable to you.
If you follow all the doctor’s recommendations, angina pectoris can be controlled, but, unfortunately, most patients ignore lifestyle instructions, which can lead to a worsening of the condition.
Diagnosis and treatment of angina pectoris at the Paracelsus Medical Center
When should you see a doctor?
The characteristic posture of a patient with an attack of angina pectoris: he stops abruptly, leans forward, with his right fist pressed to his chest.
If such attacks occur, as well as pain and discomfort in the heart area, it is necessary to consult a general practitioner or cardiologist for a detailed examination and selection of drug therapy.
First of all, the patient is recommended to make lifestyle adjustments:
- quitting smoking, alcohol, drugs;
- normalization of nutrition (reducing the percentage of animal fats, sugar, flour products, increasing the proportion of plant foods, fish);
- optimal mode of physical activity;
- treatment of concomitant diseases.
Drug treatment
To eliminate attacks of pain, nitrates, calcium channel blockers, and anticoagulants are prescribed.
Attention!
Medicines should be taken only on the recommendation of a doctor. Dosages are selected individually, taking into account the characteristics of the patient.
Nitrates cannot be combined with drugs used to treat sexual dysfunction (Viagra, Tadafil, etc.).