Reasons for the development of pathology
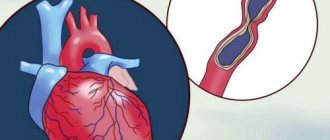
Symptoms of unstable angina develop against the background of a gradual narrowing of the lumen of the coronary arteries. This phenomenon causes necrosis of cardiomyocytes. Lipid deposits on the coronary vessels lead to the formation of atherosclerotic plaques. The patient suffers from decreased blood flow in the coronary arteries.
A significant amount of lipid deposits can cause blood clots. Damaged vessels become overly susceptible to substances released by platelets. This phenomenon provokes further narrowing of the arterial lumen.
Angina pectoris
Atherosclerosis
Diabetes
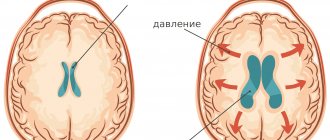
Stroke
21503 May 20
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Angina pectoris: causes, symptoms, diagnosis and treatment methods.
Definition
Angina is a clinical syndrome manifested by a feeling of tightness or squeezing pressing pain in the chest, which is most often localized behind the sternum and can radiate (“give”) to the left arm, neck, lower jaw, and to the epigastric region (epigastric region).
Pain occurs during physical activity or exposure to other factors that increase the heart's need for oxygen, and lasts from 1 to 15 minutes. It goes away with rest (when you stop exercising) or 1-3 minutes after taking nitroglycerin.
Translated from ancient Greek, angina means “narrow (weak, cramped) heart.”
Causes of angina
The development of angina is based on three mechanisms:
- atherosclerotic lesions of the coronary arteries;
- transient vascular thrombus formation;
- decreased coronary blood flow due to spasm or increased tone of the coronary arteries.
Angina pectoris makes itself felt during physical activity or stressful situations when there is a narrowing of the lumen of the coronary artery by 50-70%.
The severity of angina depends on the degree of coronary artery stenosis, its location and extent, the number and number of affected arteries. An atherosclerotic plaque can block a vessel completely or partially. With an increase in blood pressure, the inner layer of the coronary arteries (endothelium), damaged by the atherosclerotic process, can be easily damaged, blood penetrates into the plaque, the blood clotting process is activated and a blood clot is formed, which can partially or completely block the vessel.
The formation of a blood clot, especially against the background of a vessel spasm, can lead to its complete or partial blockage.
When myocardial tissue is damaged, pain mediators (serotonin, histamine, bradykinin, etc.) are released, which affect pain receptors.
There are modifiable (those that can be influenced) and non-modifiable factors that can provoke the development of angina. Modifiable diseases include dyslipoproteinemia (violation of the normal ratio of blood lipids), arterial hypertension, diabetes mellitus, smoking, low physical activity, obesity, and stress. Non-modifiable factors - male gender, age, family history of cardiovascular diseases (myocardial infarction or ischemic stroke in close relatives - up to 65 years (for women) and up to 55 years (for men)).
Classification of the disease
The most widespread classification of angina pectoris, developed
on the basis of WHO expert recommendations
:
- Stable angina pectoris (indicating functional class from I to IV).
- Class I – the patient tolerates physical activity well, angina attacks occur only during high-intensity exercise; Class II - slight limitation of usual physical activity, angina attacks occur when walking on level ground for a distance of more than 500 m, when climbing more than one floor; Class III – pronounced limitation of normal physical activity, attacks occur when walking at a normal pace on level ground for a distance of 100-150 m, or when climbing one floor; Class IV - angina occurs with little physical activity, walking on level ground at a distance of less than 100 m.
- Unstable angina:
- new-onset angina (less than 1 month from the onset of attacks);
- progressive angina (increasing attacks in frequency, duration, intensity with expanding localization and irradiation);
- early post-infarction (within 2 weeks after acute myocardial infarction) or post-operative angina.
- Spontaneous (vasospastic, variant, Prinzmetal) angina.
In practice, doctors also use the clinical classification of stable angina
:
- stable exertional angina (indicating the functional class);
- vasospastic angina;
- microvascular angina.
Symptoms of angina
Pain from angina can sometimes be perceived not as true pain, but as a feeling of discomfort, a feeling of heaviness, squeezing, tightness, distension, burning or lack of air.
Most often, the pain is localized behind the sternum or along the left edge of the sternum. It can radiate to the neck, lower jaw, teeth, interscapular space, and less often to the elbow or wrist joints, mastoid processes.
Pain with angina pectoris usually lasts from 1 to 15 minutes.
Pain occurs at the peak of physical or emotional stress. Stressful situations, due to increased activity of the sympathoadrenal system, lead to an increase in heart rate, increased blood pressure and myocardial contractility, which means the myocardial need for oxygen increases. After taking nitroglycerin or stopping the exercise, the pain stops, and the pain attack stops faster in a sitting or standing position.
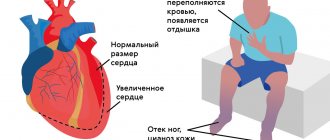
As angina progresses, a moment comes when attacks occur even with minimal exertion, and then even under conditions of physical rest.
Angina at rest joins angina pectoris and is combined with it. In such cases, attacks occur during times of increased oxygen consumption by the heart muscle, for example, during REM sleep, when the heart begins to beat faster.
In some patients, an attack of angina may occur in a horizontal position due to increased blood flow to the heart.
Vasospastic angina develops independently of physical and emotional stress, is caused by spasm of the coronary arteries, and usually occurs at a younger age than exertional angina due to atherosclerosis of the coronary arteries. In patients with vasospastic angina, many typical risk factors for atherosclerosis cannot be identified. The disease may be accompanied by threatening disturbances in heart rhythm, leading to the development of myocardial infarction and/or sudden death.
A feature of vasospastic angina is very severe attacks, usually localized in a typical location. They occur at night or early in the morning, and also when exposed to cold on exposed areas of the body.
Microvascular angina is characterized by attacks that occur some time after physical activity, during emotional stress and at rest; they are poorly controlled by nitroglycerin. The cause of microvascular angina is considered to be dysfunction of small coronary arteries (100-200 μm in diameter) in the prearteriolar segment of the coronary bed. In more than 70% of cases, microvascular angina coexists with classical angina in patients with atherosclerotic stenoses.
Diagnosis of angina pectoris
The diagnosis of angina is established on the basis of a combination of complaints (pain characteristic of angina) and information received from the patient about the course of the disease.
For all patients with suspected coronary heart disease, the following questions are asked:
- current or past smoking;
- the presence of cardiovascular diseases and/or deaths from cardiovascular diseases in the patient’s immediate relatives (father, mother, siblings);
- previous cases of seeking medical help and the presence of previously registered electrocardiograms, studies and conclusions;
- the presence of concomitant diseases in order to assess additional risks;
- currently taken medications.
To clarify the diagnosis and existing complications, data from laboratory and instrumental examination methods are used.
All patients with suspected angina are recommended to have a lipid profile tested to detect dyslipoproteinemia:
- triglycerides (Triglycerides);
Forms of pathology
The classification of unstable angina used by cardiologists takes into account the timing of the onset of primary symptoms of the disease.
| Form of angina | Description |
| First appeared | Pain syndrome develops against the background of many years of asymptomatic disease. Pain occurs during periods of physical activity of the patient. The frequency and intensity of attacks increase over time |
| Progressive | Over the course of a month, there is a sharp increase in the number of attacks. The pain syndrome develops at rest. The course of the disease is complicated by arrhythmia and functional disorder of the left ventricle |
| Spontaneous | It is characterized by single attacks that are not associated with the patient’s physical activity. The duration of the acute phase is at least 15 minutes. ECG reveals signs of ischemia, but cardiomyocyte necrosis does not develop |
| Variant | Unstable angina occurs when the patient is at rest. The attacks last more than 10 minutes. Cardialgia appears regularly, at the same time interval. Between attacks, the patient can perform any physical activity without consequences |
| Post-infarction | Develops several days after myocardial infarction. It is characterized by an extensive area of necrosis with an unfavorable course. Unstable angina of this form requires emergency care. |
Description of the disease
My patients at their initial appointment often ask the question: “What is unstable angina: a syndrome, a separate disease or a stage of exacerbation of chronic ischemic heart disease?”
The most accurate definition will be the following: this is acute myocardial ischemia, which does not lead to necrosis, that is, death, of heart cells. The sudden development of symptoms is similar to the clinical picture of a heart attack, therefore, in modern cardiology, unstable angina is included in the concept of acute coronary syndrome (ICD-10 code - I20.0). This diagnosis is “working”, emergency and must be clarified within the next few hours after the patient’s admission to the hospital. The final word here lies with laboratory tests: if the markers of myocardial necrosis are elevated, it is a heart attack; if not, it is unstable angina.
Etiology
The basis of unstable angina, like any other form of coronary artery disease, is atherosclerosis - the deposition of cholesterol in the vessel wall, leading to the formation of plaques. They can grow and penetrate inside it, which will ultimately lead to narrowing of the arteries and, as a result, hypoxia (oxygen starvation of cells). The clinic is especially clearly manifested when the heart rate increases, for example, when walking quickly or climbing stairs.
A vulnerable atherosclerotic plaque leads to unstable angina: the membrane covering its lipid core becomes thinner under the influence of various factors. This triggers a chain of reactions - inflammation, thrombus formation. A characteristic clinical symptom is pain, which is accompanied by low exercise tolerance and shortness of breath.
Signs of pathology
The main symptom of unstable angina is intense pressing pain behind the sternum. The attack can last 10-15 minutes. The pain radiates to the left arm, shoulder, shoulder blade, neck and jaw. Taking nitroglycerin by the patient does not completely relieve symptoms. Over time, the frequency and intensity of attacks increase.
Manifestations of unstable angina develop against the background of:
- physical activity;
- stressful conditions;
- changeable weather;
- excessive food consumption.
Patients may experience interruptions in heart rate that occur with minimal physical activity (moving around the apartment, performing daily household chores). Later, shortness of breath joins the listed symptoms, and the person faces a lack of air.
Doctor's advice
If, against the background of complete health, you begin to experience attacks of pressing, squeezing discomfort behind the sternum, shortness of breath when walking, decreased tolerance to physical activity (you go up to the fifth floor with stops), a burning sensation in the stomach that does not depend on food intake, I I strongly advise you to urgently consult a doctor or call an ambulance! New-onset angina can lead to a heart attack, so the danger of these symptoms should not be underestimated.
What is the algorithm for providing assistance before the medical team arrives?
Lay the patient down, provide rest, access to air, let him chew an acetylsalicylic acid tablet, if you have one, dissolve Nitroglycerin by placing it under the tongue.
What should an ambulance do upon arrival to a call (pre-hospital stage)?
- Anesthetize the patient with narcotic analgesics.
- Administer an anticoagulant (Heparin).
- Give a loading dose of a second antiplatelet agent (Clopidogrel, Ticagrelor, Prasugrel).
- Start an infusion of Nitroglycerin taking into account the blood pressure level.
- Administer beta blockers intravenously.
- If necessary (low gas concentration in the blood), start oxygen inhalation.
Diagnostic procedures
The absence of specific symptoms does not allow the cardiologist to confirm the diagnosis during a physical examination. The doctor carries out differential diagnosis to exclude heart attack and non-ischemic heart pathologies from the patient’s history. Clinical guidelines suggest the following tests to confirm unstable angina:
- electrocardiography;
- general and biochemical blood tests;
- echocardiography;
- coronary angiography.
Cardiologists detect changes in the condition of the coronary arteries and decreased left ventricular function. Based on these data, the diagnosis is confirmed.
What is the difference between unstable and stable?
Stable and unstable forms of angina can alternate in the same patient. Differential diagnosis (difference) between them lies in the nature and duration of pain, the provoking factor and the reaction to Nitroglycerin.
In patients with stable angina pectoris, anginal (“angina” is the Latin name of the disease) attacks occur when performing the same physical work and are relieved after taking Nitroglycerin or stopping the exercise. Patients get used to this: they know what actions can cause an attack, and take the medicine in advance.
With unstable angina, episodes of pain:
- occur more frequently;
- last longer;
- provoked by minimal load or develop during rest;
- do not always stop after taking Nitroglycerin.
These symptoms should cause alarm in the patient, as they indicate plaque instability and the threat of a heart attack.
Therapeutic measures
Conservative treatment involves prescribing several groups of drugs to the patient. Antianginal drugs relieve symptoms of angina pectoris. In acute attacks accompanied by intense pain, intravenous infusion of painkillers is performed.
Thrombolytics reduce the likelihood of blood clots. A similar goal is pursued when prescribing direct anticoagulants to a patient.
Lipid-lowering drugs remain an integral component in the drug treatment of unstable angina. They help normalize cholesterol levels in the patient’s blood. Constant use of such drugs reduces the likelihood of complications and recurrent attacks.
If conservative treatment is ineffective, the patient is prescribed surgery. The type of surgical intervention is determined by a cardiologist based on coronary angiography data. Imaging will allow us to understand the extent of damage to the coronary arteries. The most common methods of surgical treatment of angina remain coronary bypass surgery and coronary angioplasty.
Prognosis: is there a chance of recovery?
The answer to this question sounds disappointing: absolute recovery will not be achieved. But don't rush to panic. In the 21st century, almost all diseases have a chronic course: hypertension, diabetes, obstructive pulmonary disease, and so on. The causes of these pathologies are not bacteria, which doctors have successfully learned to fight, but lifestyle and environmental conditions.
The basis of coronary heart disease is atherosclerosis, which begins to develop with the birth of a person. Unstable angina is an acute manifestation of this process. By removing the symptoms by stenting, we do not destroy the root cause. To prevent new exacerbations, constant use of medications is necessary to prevent pathologies from progressing.
All patients want to minimize the use of pharmaceutical drugs, and some of them stop treatment after relief occurs. In their understanding, discharge from the hospital means freedom from medications, because there is no more pain. Unfortunately, such a decision often turns against them with serious consequences - a hospital bed and life-threatening complications.
In conclusion, I would like to add that cardiovascular diseases cannot always be defeated, but it is quite possible to prevent them. Weight control, smoking cessation, regular physical activity, normal cholesterol and glucose levels will help you in the fight for your health.
An important part of my work is preventive education of patients. Everyone does their own thing, and mine is to help people get rid of heart problems. Since this can only be done in the early stages of development of the pathology or at the stage of formation of a predisposition to it, I pay a lot of attention to issues of nutrition, lifestyle and screening. Only in this way - together - can we significantly improve the health of the nation.
Diagnosis and treatment of angina pectoris at the Paracelsus Medical Center
When should you see a doctor?
The characteristic posture of a patient with an attack of angina pectoris: he stops abruptly, leans forward, with his right fist pressed to his chest.
If such attacks occur, as well as pain and discomfort in the heart area, it is necessary to consult a general practitioner or cardiologist for a detailed examination and selection of drug therapy.
First of all, the patient is recommended to make lifestyle adjustments:
- quitting smoking, alcohol, drugs;
- normalization of nutrition (reducing the percentage of animal fats, sugar, flour products, increasing the proportion of plant foods, fish);
- optimal mode of physical activity;
- treatment of concomitant diseases.
Drug treatment
To eliminate attacks of pain, nitrates, calcium channel blockers, and anticoagulants are prescribed.
Attention!
Medicines should be taken only on the recommendation of a doctor. Dosages are selected individually, taking into account the characteristics of the patient.
Nitrates cannot be combined with drugs used to treat sexual dysfunction (Viagra, Tadafil, etc.).
Statistical data
Pathologies of the cardiovascular system remain the most common cause of death among Muscovites – 55% of cases in 2019. This figure is three times higher than the European average. The total number of Russian residents suffering from heart disease exceeds 16 million people. A quarter of them have congenital pathologies of the cardiovascular system. Prevention of attacks of myocardial ischemia remains one of the key tasks of cardiologists when monitoring patients at risk.
Treatment
Stopping an attack:
- calm, preferably sitting position of the patient;
- nitroglycerin under the tongue (1 tablet or 1 - 2 drops of a 1% solution on a piece of sugar, on a validol tablet), repeat taking the drug if there is no effect after 2 - 3 minutes;
- corvalol (valocardine) - 30 - 40 drops orally for sedative purposes;
- arterial hypertension during an attack does not require emergency medication, since a decrease in blood pressure occurs spontaneously in most patients;
- if nitroglycerin is poorly tolerated (bursting headache), then prescribe a mixture of 9 parts of 3% menthol alcohol and 1 part of a 1% nitroglycerin solution, 3 to 5 drops of sugar per dose.
The prognosis in the absence of complications is relatively favorable. The ability to work is preserved, but with a limitation of work that requires significant physical effort.
Diagnostics
Diagnosis of pathology includes:
- Examination of the patient. The specialist listens to heart sounds, studies anamnesis and symptoms.
- Blood test. A specialist can quickly identify existing inflammatory processes.
- Urine examination. The specialist excludes other pathologies.
- ECG. This study allows us to identify complications of coronary artery disease.
- Holter ECG monitoring. This study is being conducted to determine the frequency, conditions and duration of attacks.
- EchoCG. It is necessary to study the structure and size of the heart muscle, study the condition of the valves, and detect problems in the blood supply system. Additionally, a stress EchoECG is performed. It allows you to identify areas of myocardial hypoxia during physical activity.
- Coronary angiography. This study is carried out to study blood flow in the heart vessels.
- Scintigraphy. This study is aimed at studying the condition of the walls and cavities of the heart muscle.
Diagnostics must be performed comprehensively. Only in this case is it possible to examine all important structures and make an accurate diagnosis.