“Never sleep, you die too often in your sleep”
Mark Twain.
From WHO statistics: It has long been no secret that sleep is given to a person to restore strength after being awake. But we are talking about healthy sleep! Only he is able to “unload” the human brain. Increasingly, people go to bed, but the next morning they find themselves more unhealthy and stressed than at the end of a hard day at work. “It’s all about bad sleep,” most will say, not realizing that the concept of “bad sleep” has long been a terrible diagnosis that leads to death. And sleep disturbances hide dysfunctions of the whole body! So, we will talk about breathing disorders during sleep.
What are sleep breathing disorders?
The inability of the lungs to saturate the tissues with oxygen is most often a consequence of prolonged nighttime cessation of breathing during sleep, otherwise apnea - which translated from ancient Greek means calmness or lack of breathing. Experts divide apnea into obstructive and central.
Obstructive sleep apnea syndrome (OSA) occurs due to obstruction, that is, narrowing of the upper airways. The muscles relax, the tongue sinks into the airways and prevents the flow of oxygen into the lungs.
Doctors call OSA a “disguised killer”, because it really works “under the guise” of seemingly “banal” snoring, to which everyone has become accustomed and has long since let it float freely. But oddly enough, snoring is a bell, in some cases an alarm bell: “you have a serious problem and it requires an immediate solution!”
not as bad as the breathing disorder that snoring “masks”
In turn, pauses in breathing during sleep can last a minute and be repeated more than 20 times per night.
, and the total amount is more than an hour. Ultimately, this sleep disorder leads to hypoxia of the brain and other organs - the inability of oxygen to saturate the body. All this leads to a serious imbalance in the body.
Untreated obstructive sleep apnea results in death in three out of five cases.
.
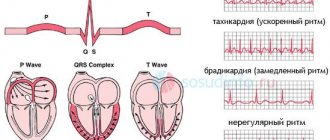
First, a person complains of high blood pressure, then of uncontrolled weight gain, in some cases diabetes mellitus, chronic fatigue, apathy, coupled with cardiac disorders, leads to heart attacks and strokes. Unfortunately, people die without knowing that the culprit is not hereditary cardiovascular pathology or excess weight, but an insidious disease - obstructive sleep apnea syndrome
.
Apnea is also neurological in nature
.
And it's called central sleep apnea syndrome.
Let's sum it up
If you experience a sudden lack of air during sleep once, there is no need to worry. However, when the disorder manifests itself regularly, there is no need to postpone a visit to the doctor.
This symptom most often indicates the development of serious diseases. The sooner the cause of respiratory failure can be determined, the greater the chance of preventing serious complications.
Monitor your health and pay attention to sudden changes in your health.
Author: Dasha Pashchenko
What happens in this case?
Since central sleep apnea
is a consequence of a disorder of the central nervous system and differs from obstructive apnea in that it is dependent on a neurological plan, and not a physiological one, this means that breathing disorder during sleep occurs from the brain.
Sleep and breathing disorders occur in the part of the brain that controls breathing. With central sleep apnea, the airways are completely free for air to enter. Central sleep apnea syndrome
It is much less common, but doctors who deal with sleep problems should certainly know the nature of your “bad sleep.”
For this purpose, several years ago, a unique diagnostic device was introduced into the circulation of somnologists - polysomnography
.
What is polysomnography?
This is diagnostic equipment designed to give a complete description of sleep
and all functions of the human body during sleep, determine the nature of the sleep disorder.
Sleep diagnostics today is the only chance to make an accurate diagnosis
and “not to miss” in the unequal struggle of doctors with breathing disorders during sleep.
Poly
- from lat.
a lot
,
dubiously
-
sleep
,
graphy
-
writing
. Diagnosis of sleep using polysomnography is the diagnosis of breathing disorders during sleep.
Polysomnography involves studying the basic functions of the body during sleep under normal human conditions. In a simulated bedroom, breathing function, heart function, brain function, blood oxygen saturation level, motor activity of the chest and abdomen, the nature of snoring and much more are monitored. Based on the results of polysomnography, the doctor gives the patient a diagnosis over the next day. After this, the patient is offered treatment. CPAP therapy
(CPAP therapy)
is recognized throughout the world as the gold standard for the treatment of apnea .
What is the treatment for sleep disordered breathing?
CPAP therapy appeared in 1981
.
This small device was created specifically for the treatment of sleep apnea by Australian professor of medicine Collin Sullivan. CPAP therapy is artificial ventilation of the lungs, which occurs through a small compressor. A tube with a mask is attached to the compressor. Coming out onto the tube and then onto the mask (which is attached to the patient's face), a constant stream of air flows directly into the respiratory tract
. CPAP machine therapy is used by doctors and patients to treat sleep apnea, snoring, respiratory failure, insomnia, depression and other sleep problems.
It is worth noting that CPAP therapy can only be prescribed by a doctor, after diagnosing sleep - polysomnography.
Treatment of apnea and snoring with CPAP therapy can last a year, in some cases a lifetime.
Patients get rid of bad sleep once and for all, they begin to lose weight, their blood pressure returns to normal, the problem of snoring “dissolves”, healthy sleep takes pride of place in a person’s bedroom! Having slept well once, as a rule, patients never part with their CPAP machine! Moreover, modern CPAP machines weigh no more than 2-3 kg and can be used not only at home and away, but also on business trips, on vacation, in the car and even on an airplane!
Sources
- Kongsong W., Rochanavibhata S. Reoperative genioplasty: a 10-year retrospective study. // Oral Maxillofac Surg - 2021 - Vol - NNULL - p.; PMID:33905017
- Schar MS., Omari TI., Woods CM., Ferris LF., Doeltgen SH., Lushington K., Kontos A., Athanasiadis T., Cock C., Chai Coetzer CL., Eckert DJ., Ooi EH. Altered swallowing biomechanics in people with moderate-severe obstructive sleep apnea. // J Clin Sleep Med - 2021 - Vol - NNULL - p.; PMID:33904392
- Matsuzaki S., Shimada A., Tanaka J., Kothari M., Castrillon E., Iida T., Svensson P. Effect of mandibular advancement device on plasticity in corticomotor control of tongue and jaw muscles. // J Clin Sleep Med - 2021 - Vol - NNULL - p.; PMID:33904391
- Strollo PJ., Soose RJ. Personalized care of obstructive sleep apnea with hypoglossal nerve stimulation. // Sleep - 2021 - Vol44 - NSupplement_1 - p.S1-S3; PMID:33903912
- Del Brutto OH., Mera RM., Castillo PR., Recalde BY., Costa AF. Previously diagnosed obstructive sleep apnea is not associated with increased risk of SARS-CoV-2 infection in community-dwelling older adults living in a highly endemic setting. // Clin Neurol Neurosurg - 2021 - Vol205 - NNULL - p.106639; PMID:33901750
- You A.H., Kang HY., Kim Y. The 95% effective target concentration of propofol for drug-induced sleep endoscopy in males with obstructive sleep apnea. // J Clin Anesth - 2021 - Vol72 - NNULL - p.110312; PMID:33901742
- Niroshana SMI., Zhu X., Nakamura K., Chen W. A fused-image-based approach to detect obstructive sleep apnea using a single-lead ECG and a 2D convolutional neural network. // PLoS One - 2021 - Vol16 - N4 - p.e0250618; PMID:33901251
- Alshhrani WM., Kohzuka Y., Okuno K., Hamoda MM., Fleetham JA., Almeida FR. Compliance and side effects of tongue stabilizing device in patients with obstructive sleep apnea. // Cranio - 2021 - Vol - NNULL - p.1-14; PMID:33899699
- Chen J., Lin S., Zeng Y. An Update on Obstructive Sleep Apnea for Atherosclerosis: Mechanism, Diagnosis, and Treatment. // Front Cardiovasc Med - 2021 - Vol8 - NNULL - p.647071; PMID:33898538
- Li W., Huang K., Wen F., Cui G., Guo H., He Z., Zhao S. Intermittent hypoxia-induced downregulation of microRNA-320b promotes lung cancer tumorigenesis by increasing CDT1 via USP37. // Mol Ther Nucleic Acids - 2021 - Vol24 - NNULL - p.528-541; PMID:33898105
Breathing disorders during sleep in patients with COPD
Patients with chronic obstructive pulmonary disease (COPD)
for physiological reasons, have rapid shallow breathing, which occurs during REM sleep.
As a result, alveolar ventilation decreases and the level of hypoxemia increases - all this leads to additional disorders. Doctors call this situation “crossover syndrome
.
Treatment of breathing disorders during sleep in patients with COPD consists of “unloading” breathing during sleep using the same CPAP therapy. Treatment of breathing disorders during sleep in such patients does not exclude treatment of the primary disease - COPD with oxygen therapy
.
As with the treatment of OSA, treatment for sleep disordered breathing in patients with COPD is prescribed by a doctor after diagnosing sleep and diagnosing sleep disordered breathing (polysomnography). Symptoms of sleep-disordered breathing that should prompt you to seek medical help:
- You snore.
- Difficulty breathing during sleep and immediately after waking up.
- Frequent awakenings during sleep.
- Increased urination at night.
- Nightmares.
- Headache in the morning.
- Fainting immediately after waking up.
- Sharp weight gain over the past 2 years.
- High blood pressure.
- Sleepiness during the day.
- Absent-mindedness.
- Irritability.
- Unmotivated depression.
- Shortness of breath while walking or doing exercise.
OSA does not have to present with all of the above symptoms. Just snoring or just obesity is enough! This is the insidiousness of OSA
. People mistakenly believe that poor sleep is associated with nightmares, excess weight with depression, shortness of breath with excess weight, snoring with a difficult day, headache with something else, and this chain closes on ignoring the symptoms. A person does not see a doctor because he cannot accept the idea that all this is a manifestation of a serious illness.
American doctors even compiled statistics on sleep-disordered breathing problems and came to the sad conclusion that every second person dies from the consequences of a sleep disorder
due to simple ignorance about their diagnosis, as well as a frivolous attitude towards the problem of snoring.
And remember, treatment for sleep disordered breathing begins with a sleep diagnosis! Making an accurate diagnosis and systemic treatment will not only relieve you of bad sleep and return you to a normal healthy life, but will also prolong your life for many years! After all, OSA and the problem of snoring in themselves are not as terrible as what they lead to - cardiovascular diseases and death.
Don’t forget, health is, first of all, healthy sleep!
Prevention of apnea BEFORE and AFTER treatment
Apnea is not a harmless breathing disorder, as the increase and intensification of symptoms over time causes serious complications. Therefore, prevention is needed both before and after treatment.
"BEFORE"
Before therapeutic measures, prevention makes it possible to identify the causes of the disease and suppress their further development:
- In the first place is timely examination of somatic diseases and their treatment. We are talking about the thyroid gland, brain, ENT organs, lungs and heart. Systematic monitoring of sugar levels, thyroid hormones, and blood pressure are mandatory parts of the preventive program.
- Control of body weight and its systematic reduction if the excess is more than 10% of the standard is of great importance.
- It is very important to give up habits that are always and everywhere considered harmful. These include alcohol and smoking, stress and a night work schedule.
- You cannot do without regular aerobic exercise - swimming and walking, competitive sports and cycling.
If breathing difficulties are caused by anatomical defects, then you should think about surgical correction of a deviated nasal septum or enlarged tonsils.
"AFTER"
When apnea is over, this does not mean that you can now “release the brakes.” Patients must follow simple rules aimed at consolidating the positive results achieved.
- Eat a low-calorie, vitamin-rich diet
- Limit your intake of carbohydrates and fats, especially hard fats
- Eat food no later than 3, or preferably 4, hours before going to bed
- You may benefit from sleeping on your side or stomach. Place your head and spine at the same level in bed
- Ensure normal humidity in the sleeping area
To prevent the disorder from returning or worsening, practice going for a massage. A good help is soothing baths before bed. This will allow you not only to get a good night's sleep, but also to forget about restless nights forever.