How to diagnose atrial fibrillation using an ECG
Fibrillation is characterized by a tachyarrhythmia-like heartbeat, rapid, irregular pulse and heart contractions.
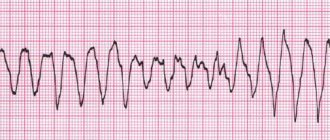
Most patients experience chest tremors and weakness. A distinctive symptom is an inconsistent pulse. But sometimes atrial fibrillation is asymptomatic, and therefore an electrocardiogram is considered the standard method for detecting heart rhythm disturbances. The main signs of atrial fibrillation on the ECG (photo 1):
- P waves are not recorded in all 12 leads, since the impulses pass chaotically through the atria;
- small random f waves are determined, most often recorded in leads V1, V2, II, III and aVF;
- ventricular QRS complexes become irregular, a change in the frequency and duration of the R-R intervals is observed, AV block is detected against the background of a low frequency of ventricular contraction - bradyform fibrillation;
- QRS complexes do not change, without deformation or widening.
Photo 1: Example of an ECG with atrial fibrillation.
Arrhythmia is manifested by rapid or slow contraction of the heart. Atrial fibrillation on the ECG is divided into two types:
- in the tachysystolic variant, electrocardiography reflects a heart contraction of more than 90 beats per minute (photo 2);
Photo 2: Tachysystolic form of AF.
- bradysystolic variant - contractions less than 60 beats per minute. (Fig. 3);
Photo 3: Bradysystolic form of AF.
With arrhythmia, contractions arise from different sections of muscle fibers, ectopic foci, as a result of which there is no single contraction of the atria. Against the background of hemodynamic failure, the right and left ventricles receive insufficient blood volume, cardiac output decreases, which determines the severity of the disease. Decoding the cardiogram helps to establish the exact heart rhythm disorder.
A characteristic sign of fibrillation on the ECG is f waves (large-wave and small-wave):
- in the first case, fibrillation is determined by large waves, atrial fibrillation reaches 300-500 per minute;
- in the second, the flicker waves become small, reaching 500-700 per minute.
Atrial flutter is a variant of slower contraction of the heart muscle, in the range of 200-300 beats per minute. Patients with persistent atrial fibrillation experience frequent flutter recurrences. Such an emergency requires urgent medical attention.
Analysis of cases of paroxysms shows that on average, in 10% of patients, an attack of atrial fibrillation turns into flutter, which is determined on the ECG in the form of the following description:
- the absence of P waves and the replacement of small f waves with large sawtooth waves F is the main characteristic, which is presented in photo 4;
- normal ventricular QRS complexes.
Photo 4:
Atrial flutter
regular contraction of the atria with a frequency of about 250-350 per minute.
The ventricular rate (VFR) is determined by atrioventricular conduction; the ventricular rhythm can be regular or irregular.
Atrial flutter is a form of atrial fibrillation; its clinical manifestations differ little from atrial fibrillation, but it is characterized by somewhat greater persistence of paroxysms and greater resistance to antiarrhythmic drugs.
Distinguish between the correct
(rhythmic) and
irregular
forms of this arrhythmia.
In interventional arrhythmology, the following classification is accepted: Typical
AFL,
Atypical
AFL,
Left atrial
AFL.
Types of atrial fibrillation and an example of a diagnosis
Clinically, atrial fibrillation manifests itself in several forms:
- paroxysmal, when an attack of fibrillation lasts no more than 48 hours in the case of successful treatment (cardioversion), or paroxysm is restored within 7 days;
- persistent - arrhythmia lasts more than a week, or fibrillation can be eliminated later than 48 hours with drug therapy and electrical stimulation;
- permanent form, when chronic fibrillation is not eliminated by cardioversion. Drug assistance in this case is ineffective.
Taking into account the heart rate data and signs of typical atrial fibrillation on the ECG, three variants of fibrillation are determined:
- normosystolic form - heart rate within 60-100 beats per minute;
- tachysystolic - heart rate more than 90 beats per minute;
- bradysystolic - heart rate less than 60 beats per minute.
The clinical diagnosis of the patient includes the characteristics of the arrhythmia and ECG data, which are deciphered: atrial fibrillation, persistent form, tachysystolic variant.
Classification of atrial flutter (according to M. Scheinman, 1999)
| Variant of atrial flutter | ECG signs | Heart rate | TP substrate |
| Typical TP : - counterclockwise (CCW) - clockwise (CW) | - II; III; F; +V1, +II; III; F; -V1 | 240-340 240-340 | Isthmus-dependence Isthmus-dependence |
| Atypical TP : - two-wave re-entry - lower loop re-entry - multiple cycles | - II; III; F; +V1, +II; III; F; -V1 Variable | 350-390 200-260 | Isthmus-dependence Isthmus-dependence Multiple re-entry |
| Left atrial atrial fibrillation | Variable | Silent zone of LA and PV Membranous part of IPP Estuary of CS |
Basic principles of treatment
Modern therapy for arrhythmia is based on methods of restoring the heart rhythm to sinus and preventing new attacks of paroxysms with the prevention of thrombus formation. The provisions of the medical care protocol include the following items:
- antiarrhythmic drugs are used as medicinal cardioversion to normalize heart rhythm;
- beta-blockers are prescribed to control heart rate and the quality of contraction of the heart muscle (contraindication - patients who have a pacemaker implanted);
- anticoagulants prevent the formation of blood clots in the heart cavity and reduce the risk of stroke;
- metabolic drugs act as a stabilizer and improve metabolic processes;
- Electrical cardioversion is a method of electrical impulse relief of an attack of atrial fibrillation. To do this, atrial fibrillation is recorded on an ECG and defibrillation is performed under the control of vital signs. The only criterion for prohibiting such a procedure is severe bradycardia and persistent fibrillation for more than two years.
Etiology and pathogenesis
The most common cause of atrial flutter is a change in the conduction system of the heart due to diseases:
- coronary heart disease (CHD). For example, in acute myocardial infarction (AMI), according to various data, TP occurs in 0.8 to 5.3% of cases - rheumatism
(especially in persons with mitral stenosis);
- arterial hypertension
;
- idiopathic cardiomyopathies
;
- chronic
or
acute cor pulmonale
;
— chronic nonspecific pulmonary diseases
and chronic obstructive pulmonary diseases;
- hyperthyroidism
;
- myocarditis
;
- pericarditis
;
- atrial septal defect
in adults -
ventricular pre-excitation syndrome
(WPW - syndrome) -
sinus node dysfunction
(SSND) - tachy-brady syndrome;
— idiopathic variants
— pathological desympatization of the atria.
Complications of the disease
In atrial fibrillation, the upper chambers of the heart are not fully filled with blood, causing reduced output and heart failure.
WPW syndrome with early excitation of the ventricles provokes the development of supraventricular arrhythmia, worsening the course of the disease and making it difficult to diagnose cardiac arrhythmias.
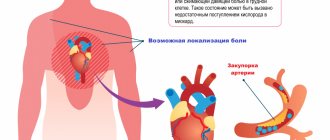
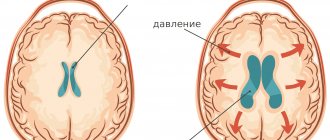
In addition to reducing the blood filling of the cavities of the heart, the chaotic contraction of the atria forms clots and thrombi, which, with the blood flow, enter the small and large vessels of the brain. Thromboembolism is dangerous due to complete closure of the arteriole and the development of ischemia, which requires resuscitation measures and initiation of treatment as soon as possible.
History of the development of ideas about atrial flutter
IN 1918
Mr.
T. Lewis
suggested the focal theory of atrial fibrillation, which assumed the formation of a high-frequency electrically active focus in the atria.
However, already in 1925
d. This author changes his ideas and speaks out in favor of intraatrial re-entry as a substrate of AFL.
The theoretical concept of TP has undergone changes in subsequent years from the original focal theory to the electrical excitation reentry theory:
— 1947
g. -
A. Rosenblueth
and
Garcia-Ramos,
in a surgical experiment, accidentally expanded the incision between the inferior and superior vena cava into the area of the free wall of the RA. The result was the manifestation of TP, the mapping of the cycle of which revealed the circulation of a re-entry wave along the perimeter of the cut being performed.
— 1949
g. -
D. Scherf
developed the focal theory of TP.
— 1954
Mr. -
E. Kimura
also put forward the focal theory.
— 1986
g. -
L. Frame
postulated re-entry as the initiating mechanism of TP.
L.Frame
performed the so-called Y-shaped incision, shown in Figure 5, and for the first time verified the topographic separation of the atrial incision from the area of re-entry wave circulation underlying AFL.
— 1982-1984
gg.
— M. Allessie,
based on the use of the acetylcholine model, speaks in favor of the re-entry mechanism underlying TP.
— 1981-1988
gg.
— P. Boyden
creates a model of tricuspid regurgitation and a model of pulmonary artery clipping. Evidence for the nature of re-entry TP.
— 1986
g. —
A. Waldo,
based on a sterile pericardial model, verifies re-entry as the leading mechanism of TP.
— 1991
g. -
J. Cox
, using the model of mitral regurgitation, advocates the re-entry theory underlying TP.
The evolution of clinical ideas about the nature of TP is similar:
— 1951
g. -
M. Prinzmetal,
based on the use of photographic technology, spoke in favor of the focal nature of TP.
— 1971
g. -
H.Wellens
, using the epicardial mapping method, confirms the position about the focal nature of AFL.
— 1986-1990
gg.
— F. Cosio
and
B. Olshansky
verify re-entry as the basis of TP.
Thus, the 90-year journey from the focal theory to the idea of re-entry has taken place.
Cardiac resynchronization therapy
Bipolar pacemaker in the treatment of heart failure
Look
indications, use in clinical practice
Ongoing research
The following methods are used to diagnose atrial flutter:
- ECG - allows you to record the type of rhythm disturbances
- Daily (Holter) ECG monitoring allows you to estimate the pulse rate at different times of the day, incl. during sleep, record paroxysms, if any
- EchoCG - ultrasound of the heart - allows you to assess the size of the heart chambers, myocardial contractility, the condition of the heart valves (they also affect arrhythmia)
- Blood tests can reveal a lack of electrolytes (potassium), dysfunction of the thyroid gland (increased levels of thyroid hormones), signs of acute rheumatism or myocarditis
- Sometimes there is a need to conduct an electrophysiological study (EPS) of the heart
to the top of the page
Pathogenetic significance of TP
The main factors of pathogenetic significance are high heart rate and associated symptoms in this category of patients.
Against the background of tachysystole, diastolic contractile dysfunction of the left ventricular (LV) myocardium develops, subsequently systolic contractile dysfunction and then a possible outcome in dilated cardiomyopathy and heart failure .
Pathogenetic cascade of atrial flutter Enlarge
to the top of the page