Etiology of AF and cardiovascular risks
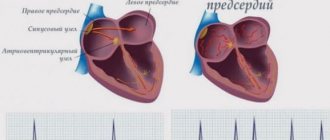
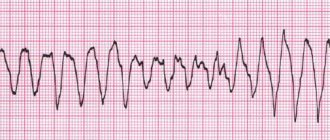
Atrial fibrillation is defined as a supraventricular tachyarrhythmia characterized by chaotic electrical activity of the atria at a high rate (350-700 per minute) and an irregular ventricular rhythm1. Previously, the term “atrial fibrillation” was widely used, which quite accurately conveys the essence of atrial fibrillation.
According to foreign studies, AF is the most common form of tachyarrhythmia in the world and occurs in 2% of the population2. There are valvular and non-valvular AF (NVAF). In the first case, AF is associated with damage to the heart valves and overload of the left atrium with pressure or volume, due to which fibrillation begins. The most common cause of valvular AF is rheumatic mitral valve stenosis or replacement1. All other cases of atrial fibrillation are defined as non-valvular.
NFP occurs against the background of a number of diseases and conditions, such as coronary heart disease, hypertension, primary myocardial diseases, diabetes mellitus, pheochromocytoma, as well as alcohol abuse, excess body weight and hypokalemia3. Due to the chaotic movement of blood in the fibrillating left atrium, the prerequisites are created for the formation of blood clots, which can spread through the left ventricle throughout the systemic circulation. Thromboembolic complications are the most dangerous complications of AF. These include:
- ischemic cardioembolic stroke;
- heart attacks of internal organs;
- thromboembolism of the vessels of the extremities.
In a cardioembolic stroke, an embolus (thrombus) located in the left atrium breaks off and enters the arterial system of the brain.
According to a number of epidemiological studies, NFP increases the risk of stroke by 2.6-4.5 times, depending on the clinical parameters of patients4. Moreover, for women, these risks, other things being equal, are higher than for men5.
A stroke that occurs during NAF is severe and more often leads to disability than a stroke in patients without AF6. The basis for the prevention of thromboembolism in NFP is oral anticoagulants. They reduce the activity of blood clotting and thus prevent the formation of emboli (blood clots). 10 years ago, the drug of choice was the vitamin K antagonist warfarin, but direct oral anticoagulants (DOACs) appeared, in particular apixaban, which have a number of advantages over warfarin, which allowed DOACs to become the standard for stroke prevention in NAF.
Right ventricle
Functional anatomy of the right ventricle
The volume of the right ventricle in newborns is 8.5-11 cm3, in children of the first year of life - 13-20 cm3, at 7-9 years old - 28-40 cm3, by the age of 18 it reaches 150-225 cm3. In newborns and children under 1 year of age, the length of the right ventricle is 4.3-6.2 cm, width 2.1-3.2 cm; in 7-12 year old children, the length of the ventricle increases to 5-7.2 cm, width - up to 2-3.5 cm. By the age of 18, the length of the right ventricle reaches 7.3-9.2 cm, width - 3-5 cm. The thickness of the free wall of the right ventricle in children under 1 year is 0.1-0.16 cm, by 6 years it increases to 0.2 cm, and by 12 years it reaches 0.32 cm. The cavity of the right ventricle has pronounced trabecularity, with the bases of the papillary muscles located in the thickness of the trabeculae.
One-dimensional echocardiography of the right ventricle
The inflow section of the right ventricle is studied in standard position I, and the outflow section in standard position IV. The transverse size of the right ventricle according to echometry does not correspond to the anatomical one, since the ultrasound beam crosses the ventricular cavity in the area corresponding to 1/3 of the maximum transverse diameter of the sphere. The thickness of the free wall of the right ventricle in one-dimensional and two-dimensional images is usually greater than the anatomical one due to the pronounced trabecularity of the cavity. Normal values for the cavity of the right ventricle and the thickness of its free wall are presented in tables 5, 8, 15.
Semiotics of the right ventricle
Right ventricular dilatation
- Idiopathic dilatation of the pulmonary artery.
- Congenital absence of the pulmonary valve.
- Partial absence of the pericardium.
- Atrial septal defect (primary, secondary).
- Abnormal drainage of the pulmonary veins (partial, total).
- Ebstein's anomaly (meaning an increase in the atrialized portion of the ventricle).
- Tricuspid valve insufficiency.
- Pulmonary valve insufficiency.
- Fistula of the right coronary artery into the right ventricle.
- Congenital absence of the pulmonary valve.
- Tumor of the right ventricle.
- Left ventricular hypoplasia syndrome.
- Transposition of the great vessels.
- Pulmonary hypertension (primary, secondary).
- Myocarditis.
- Congestive heart failure.
- Restrictive cardiomyopathy.
- Change in the position of the heart (rotation of the right ventricle anteriorly).
Reduction of the right ventricular cavity
- Atresia of the tricuspid valve.
- Pericardial tamponade.
- Pulmonary atresia with intact interventricular septum.
- Concentric hypertrophy of the right ventricle.
- Aneurysm of the interventricular septum.
- Compression of the right ventricle by a mediastinal mass.
- Change in the position of the heart (posterior rotation of the right ventricle).
Hypertrophy of the free wall of the right ventricle
(increase in wall thickness by more than 3 - 5 mm)
- Pulmonary artery stenosis (infundibular, valvular, supravalvular, stenosis of the left or right branch of the pulmonary artery).
- Pulmonary hypertension (primary, secondary).
- Restrictive cardiomyopathy.
- Tumor of the right ventricle.
- Tetralogy of Fallot.
- Transposition of the great vessels.
- In newborns born to mothers with diabetes.
- Hypertrophic cardiomyopathy with obstruction of the right ventricular outflow tract.
Additional echoes in the right ventricular cavity
- Abnormal muscle bundles.
- Tumors of the right ventricle (usually rhabdomyomas).
- Rupture of an aneurysm of the sinus of Valsalva into the cavity of the right ventricle.
- Aneurysm of the interventricular septum.
- Thrombus in the right ventricle.
Two-dimensional echocardiography of the right ventricle
The right ventricle is visualized in mutually perpendicular scanning axes: the inflow portion - in the projection of 4 chambers from the apex and in the transverse parasternal section; outflow - in the parasternal projection of the outflow tract of the right ventricle and the cross section at the level of the great vessels.
Volume overload of the right ventricle
- Dilatation of the right ventricle.
- Paradoxical movement of the interventricular septum (cm) (may not be detected in the presence of pulmonary hypertension).
- Increased excursion of the anterior leaflet of the tricuspid valve.
- Systolic flutter of the tricuspid valve.
- Decreased amplitude and speed of opening of the anterior leaflet of the mitral valve.
Right ventricular hypertrophy
- An increase in the thickness of the free wall of the right ventricle by more than 5 mm.
- Hypertrophy (right side) of the interventricular septum.
- Increased trabecularity of the right ventricular cavity.
Eliquis® (apixaban) for non-valvular atrial fibrillation
To date, the only drug with the INN apixaban registered in Russia is Eliquis®. This drug is a direct selective inhibitor of coagulation factor Xa, due to which it interrupts the coagulation cascade and prevents the formation of blood clots.
The superiority of apixaban over warfarin was demonstrated in the double-blind, randomized international clinical trial ARISTOTLE, the results of which were published in 20117. We analyzed data from 18,201 patients with atrial fibrillation and risk of stroke, divided into groups of patients taking INR-guided warfarin or apixaban.
The study results showed that apixaban, compared with warfarin, reduced the risk of stroke by 21%, the risk of major bleeding by 31%, and overall mortality by 11%.
Thus, to date, Eliquis® is the only direct oral anticoagulant that has shown superiority over warfarin in patients with NAF according to three main clinical indicators based on CT results.
In addition, the advantage of apixaban is its favorable safety profile. The drug has low renal excretion (renal excretion 27%), which allows its use in mild to moderate renal impairment8.
Also, Eliquis® at the full therapeutic dose (5 mg twice daily) is suitable for most patients with NFP and does not increase the risk of gastrointestinal bleeding7.
The treatment regimen for the drug on an outpatient basis looks very simple and is easy for the patient to remember: one 5 mg tablet twice a day, regardless of meals. (2.5 mg twice daily if two or more of the following are present: age 80 years or older, body weight 60 kg or less, or plasma creatinine concentration ≥1.5 mg/dL (133 µmol/L) ; or with creatinine clearance 15–29 ml/min).
Symptoms of hypertrophy
In the early stages, there are no pronounced symptoms, while when the process is advanced, a whole variety of signs can be observed, among which experts identify:
- headache;
- pain in the left side of the chest, which can radiate to the back, left arm or neck;
- heart rhythm disturbances;
- pressing pain in the chest;
- sleep disorders;
- cachexia;
- increased fatigue.
Also, people with a hypertrophied left atrium may experience periodic loss of consciousness, which is caused by a lack of oxygen. The same deficiency provokes shortness of breath. In the first stages of the disease, it can be observed in patients during sports or heavy physical activity, while in advanced cases it occurs in a state of complete rest.
Left atrial hypertrophy is dangerous because in the early stages it may not bother a person at all and may not cause him discomfort. The patient knows nothing about hypertrophy until it reaches significant proportions.
Ignoring these symptoms can lead to severe, irreversible consequences that can result in death. Therefore, if you detect any signs, you need to contact a specialist as quickly as possible, because only he can help as effectively as possible.
Right atrium
Functional anatomy of the right atrium
The right atrium is cylindrical; in newborns the volume of the cavity is 6.5-10 cm3, by the end of 1 year of life - 11-18 cm3, at 7-9 years old - 22-36 cm3, at 18-25 years old - 100-150 cm3.
The right atrium is studied in two-dimensional mode from the projection of 4 chambers from the apex or subxiphoidally. With subxiphoidal access, it is possible to visualize the confluence of the inferior vena cava, as well as its valve (endocardial fold 5-10 mm high) and the intervenous tubercle (at the border of the mouths of the superior and inferior vena cava). On the lateral wall of the right atrium, in some cases it is possible to visualize a muscular cushion (the border crest of the right atrial appendage). With dilatation of the appendage, the pectineus muscles can be visualized as trabecular formations, usually connected to the mouth of the vena cava.
The size of the right atrium depends on age: in newborns and children under one year old, the anteroposterior size ranges from 1.1 to 2.1 cm, in children 1-6 years old - 1.1-2.5 cm, in children 7-12 years old - 1 .3-2.5 cm, 13-17 years old - 1.4-2.5 cm. The width of the atrium in newborns and children under 1 year is from 1.2 to 1.9 cm, in children 1-6 years old - 1. 2-2.3 cm, for children 7-12 years old - 1.3-2.3 cm, for 13-17 year olds - 1.4-2.3 cm.
Two-dimensional echocardiography of the right atrium
The right atrium is visualized in several longitudinal and cross sections. From the subcostal approach, the place where the inferior vena cava flows into the chamber cavity (situs solitus) is determined. In the projection of 4 chambers from the apical or subcostal approach, the shape of the chamber, the presence of additional formations in it, and the relationship with the ventricular chamber are established.
Semiotics of the right atrium
Right atrium dilatation
- Idiopathic aneurysm of the right atrium.
- Abnormal drainage of the pulmonary veins.
- Atrial septal defect.
- Open atrioventricular canal.
- Ebstein's anomaly.
- Tricuspid valve stenosis.
- Tricuspid valve insufficiency.
- Tumor of the right atrium.
- Restrictive cardiomyopathy.
- Arrhythmogenic dysplasia of the right ventricle.
- Partial congenital absence of the pericardium.
- Pulmonary heart.
- Congestive heart failure.
- Constrictive pericarditis.
- Aneurysm of the sinus of Valsalva ruptures into the right atrium.
- Portal hypertension.
Reduction of the right atrium cavity
- Compression due to mediastinal tumors.
- Right ventricular hypoplasia syndrome.
- Large left-to-right shunt at the level of the ventricles (VSD) or great vessels (PDA).
Additional echoes in the right atrium cavity:
- Tumors of the right atrium (usually myxomas).
- Valve of the coronary sinus.
- Valve of the inferior vena cava (Eustachian valve).
- Valve of the oval hole.
- Pectineus muscles of the right atrial appendage.
- Thrombus in the right atrium.
- Tricuspid valve prolapse.
- Valve prolapse of the inferior vena cava.
- Aneurysm of the interatrial septum.
Interventricular septum
Functional anatomy of the interventricular septum
The interventricular septum separates the left ventricle from the right, has a complex spherical structure, and makes up 1/3 of the total mass of the ventricles. The radius of curvature of the septum is the same as that of the free wall of the left ventricle. On both the left and right ventricular sides, the septum has a triangular shape (Fig. 67). In functional and morphological terms, the septum is divided into 4 sections: inflow (inlet), outflow (outlet), trabecular and membranous portions. The first three sections form the muscular part of the septum. The membranous part of the septum forms the medial wall of the left ventricular outflow tract: on the side of the right ventricle, the anterior and septal leaflets of the tricuspid valve are attached to it. The inflow section forms the medial wall of the inlet tract of the left and right ventricles, respectively, the outflow section of the IVS forms the outflow tract of the left and right ventricles. Between the inflow and outflow sections is the trabecular part of the septum.
One-dimensional echocardiography of the interventricular septum
In a one-dimensional study, the interventricular septum is visualized as a strip of linear echo signals separating the cavity of the right ventricle from the left. During systole, the septum moves towards the posterior wall of the left ventricle and thickens. The nature of the movement and the thickness of the partition in one-dimensional mode are determined in the first standard position (Fig. 68).
Fig.67
Scheme of the functional and morphological sections of the interventricular septum from the right (a) and left (b) ventricles.
1 - inflow section (in let), 2 - outflow section (out let).
Along with this, the fraction of systolic thickening of the IVS is calculated: F IVS = { (Tc - Td) / T } * 100%
, where
Fig.68
Scheme of normal movement of the interventricular septum.
F IVS - fraction of systolic thickening (in %), Tc - IVS thickness in systole, Td - IVS thickness in diastole (cm, mm). Normally, F IVF ranges from 30 to 80%.
Semiotics of the interventricular septum:
Hypertrophy of the interventricular septum
Fig.69
Hypertrophy of the interventricular septum (diagram). An increase in diastole thickness of the septum by more than 5 mm in children under 1 year of age, more than 8 mm in children under 3 years of age, and more than 10 mm in children over 3 years of age. It can occur from the right and left ventricles or be isolated (Fig. 69).
Causes of right-sided IVS hypertrophy
- Pulmonary hypertension (primary, secondary).
- Open atrioventricular canal.
- Tetralogy of Fallot.
- Isolated pulmonary artery stenosis.
- Eisenmenger syndrome.
Causes of left-sided IVS hypertrophy
- Arterial hypertension.
- Hypertrophic cardiomyopathy (obstructive, non-obstructive).
- Athletic heart (hypertrophy of the interventricular septum in athletes).
- Aortic stenosis (subvalvular, valvular, supravalvular).
- Restrictive cardiomyopathy (cardiac amyloidosis, cardiac hemochromatosis, endocardial fibroelastosis).
Causes of isolated IVS hypertrophy
- Idiopathic hypertrophic subaortic stenosis.
- Initial stages of arterial hypertension.
- Intramural tumor of the IVS.
Pseudohypertrophy of the IVS:
- Incorrect orientation of the IVS (with anomalies in the position of the heart) or violation of the research technique (visualization of the septum at a large scanning angle).
- Parietal thrombus.
- Longitudinal trabeculae along the interventricular septum.
- Intracavitary tumor adjacent to the interventricular septum.
- Bacterial vegetation on the septum.
Hypokinesia of the interventricular septum
Fig.70
Hypokinesia of the interventricular septum (diagram). Normally, the systolic excursion of the IVS is 4-9 mm) (Fig. 70).
- Carditis, cardiomyopathies.
- Conditions associated with volume overload of the right ventricle (cor pulmonale, ASD).
- Congestive heart failure.
Hyperkinesia of the interventricular septum
Fig.71
Hyperkinesia of the interventricular septum (diagram). Increase in systolic excursion over 10 mm (Fig. 71).
- Mitral insufficiency of any etiology.
- Hyperkinetic cardiac syndrome (mitral valve prolapse, vegetative-vascular dystonia).
- Conditions associated with volume overload of the left ventricle (PDA, VSD).
- Small pericardial effusion.
Paradoxical movement of the interventricular septum
Fig.72
Variants of paradoxical movement of the interventricular septum.
The following types of paradoxical movement of the IVS are distinguished (Fig. 72):
Type A
- the septum moves in the opposite direction during systole (concordant with the posterior wall of the left ventricle) (Fig. 73);
Type B
- (otherwise referred to as variable motion) at the beginning of systole, the septum moves paradoxically, then has a flattened backward movement.
Fig.73
Paradoxical movement of the interventricular septum in atrial septal defect. Types A and B of paradoxical motion are usually combined with volume overload of the right ventricle. A close relationship between the degree of volumetric overload and the type of movement of the IVS has not been established, however, in practice, type A movement corresponds to a greater degree of overload.
Passive paradoxical movement of the IVS
— throughout the entire systole, the septum makes a slow forward movement, while its systolic thickening is practically absent
Abnormal movement with left bundle branch block
- this variant is manifested by rapid diastolic movement back at the beginning of systole, then the septum moves as in type A paradoxical movement.
The main conditions accompanied by paradoxical movement of the IVS:
- Volume overload of the right departments:
- Atrial septal defect (primary, secondary).
- Abnormal drainage of the pulmonary veins (partial, complete).
- Ebstein's anomaly.
- Pulmonary valve insufficiency.
- Open atrioventricular canal.
- Tricuspid valve insufficiency.
- Congenital absence of the pulmonary valve.
- Fistula of the right coronary artery into the right ventricle.
- Idiopathic dilatation of the pulmonary artery.
- Left ventricular hypoplasia syndrome.
- Anomalies of the cardiac conduction system:
- Wolff-Parkinson-White syndrome type B.
- Left bundle branch block.
- Ventricular arrhythmias.
- Pacemaker in the right ventricle.
- Pericardial pathology:
- Congenital partial absence of the pericardium.
- Constrictive pericarditis.
- Idiopathic aneurysm of the right atrium.
- Pleuropericardial adhesions.
- After heart surgery:
- After suturing or repair of VSD.
- After radical correction of tetralogy of Fallot.
- After mitral valve replacement.
- After aortic valve replacement.
- Other reasons:
- Corrected transposition of the great vessels.
- Arrhythmogenic right ventricular dysplasia syndrome.
- Tumors of the right ventricle.
- Dyskinetic segments with anomalies of coronary circulation.
- Hypertrophic cardiomyopathy with left ventricular outflow tract obstruction (LVOT).
- Dilated cardiomyopathy.
- Endocardial fibroelastosis.