Make an appointment by phone: +7 (343) 355-56-57
+7
- About the disease
- Cost of services
- Sign up
- About the disease
- Prices
- Sign up
Atrial fibrillation (AF)
is the most common rhythm disorder. It is registered everywhere and occurs in almost all age groups, but the frequency of its occurrence increases with each decade of life.
If you consult a doctor in a timely manner, correctly selected treatment and the patient follows all the doctor’s orders, the prognosis for this disease is quite favorable and the patient’s quality of life does not suffer significantly.
This applies to patients of all age groups, including the elderly.
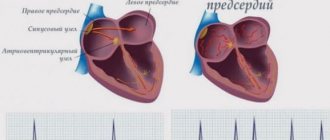
Normally, the human heart has a conducting system. It is similar to electrical wiring and its function is to conduct impulses from the sinus node located in the left atrium to the heart muscle, causing it to contract. With atrial fibrillation, the function of one “power source” (sinus node) is taken over by multiple arrhythmic foci in the atrium and the heart contracts chaotically. That is why this arrhythmia is also called delirium cordis (delirium of the heart).
These arrhythmic foci can be quite small and multiple, and then this form of AF is called atrial fibrillation
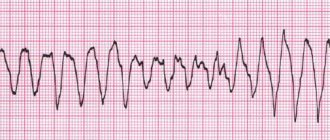
(from Latin fibrillatio - small contractions, trembling). With larger and more organized foci of arrhythmia, they speak of atrial flutter (reminiscent of the flutter of a bird or butterfly wing). Atrial fibrillation is always chaotic and absolutely arrhythmic contractions of the heart. Atrial flutter can be either regular or irregular in shape. In the first case, the rhythm is correct, but in the second, it is as chaotic as in atrial fibrillation. These forms of MA can be distinguished only by ECG. However, the methods of diagnosis and treatment, as well as prevention of these forms of the disease, are the same. Although with atrial flutter there is a greater effect from surgical treatment methods.
Like any disease, MA has its own course. It begins, as a rule, with a suddenly developing episode (paroxysm), which can end as suddenly as it began.
In this case, restoration of normal (sinus) rhythm can occur both spontaneously (on its own) and with the help of special medications - antiarrhythmic drugs.
The further course of this disease is completely unpredictable. After the first paroxysm, this ari often lasts for many years, and then it can appear at the most unexpected moment. Or, conversely, after the first episode, rhythm disturbances become more and more frequent. And, as a rule, with the increase in frequency and lengthening of paroxysms of MA, it gradually turns into a permanent form, that is, it settles in the patient’s heart forever.
In some cases, when paroxysms are repeated quite often and exhaust the patient, the transition of the arrhythmia to a permanent form brings him relief, because each episode of failure and recovery leads to complications.
In any case, you can live with this arrhythmia, you just need to master the basic principles of managing it. However, it should be understood that it is almost impossible to cure this disease once and for all, like many other diseases (bronchial asthma, diabetes mellitus, hypertension, coronary heart disease, etc.) - you can only coexist with MA, control its symptoms and prevent the development of complications.
A special cohort consists of patients with frequent relapses of AF. In this case, we are talking about either incorrect treatment (the patient does not take the medications, or takes them in an insufficient dose, and the problem can be solved with the help of an arrhythmologist). However, in some cases, an increase in paroxysmal AF is a natural course of the disease, indicating that the paroxysmal form of AF will soon become permanent. This process can be interrupted using surgical treatments.
Symptoms of atrial fibrillation
The most common symptoms of atrial fibrillation are:
- interruptions in the heart,
- heart sinking,
- frequent irregular heartbeat,
- chest pain,
- dizziness,
- fainting or momentary loss of consciousness,
- difficulty breathing, lack of air,
- dyspnea,
- increased fatigue,
- general weakness.
Often, atrial fibrillation is asymptomatic and is detected incidentally on an ECG or during Holter monitoring.
Types of atrial fibrillation (AF)
The term “atrial fibrillation” can refer to the following two types of supraventricular tachyarrhythmia.
Fibrillation (atrial fibrillation).
Normally, an electrical impulse arises in the sinus node (in the wall of the right atrium), spreads throughout the myocardium of the atria and ventricles, causing their successive contraction and ejection of blood. In AF, the electrical impulse travels chaotically, causing the atria to “flicker” as the myocardial fibers contract uncoordinatedly and very quickly. As a result of the chaotic transmission of excitation to the ventricles, they contract irregularly and, as a rule, not efficiently enough.
Atrial flutter.
In this case, contraction of myocardial fibers occurs at a slower pace (200–400 beats/min.). Unlike AF, with flutter the atria still contract. As a rule, due to the refractory period of the atrioventricular node, not every electrical impulse is transmitted to the ventricles, so they do not contract at such a rapid pace. However, as with fibrillation, with flutter the pumping function of the heart is disrupted, and the myocardium experiences additional stress.
Atrial fibrillation classification (ESCGuidlines):
- The paroxysmal form is a sudden onset of AF, lasting from several minutes to 7 days, recovering on its own (usually within 24-48 hours).
- The persistent form is atrial fibrillation lasting from 7 days to 1 month. It does not recover on its own, but there are indications and the possibility of cardioversion.
- Long-term persistent form - atrial fibrillation lasting more than 1 month, persisting or relapsing, despite attempts at cardioversion.
- The permanent form is atrial fibrillation in which cardioversion is contraindicated, was not performed, or was unsuccessful.
The prevalence of atrial fibrillation is 6% in elderly and senile people and about 2% among the entire population. In 6-10% of patients with coronary artery disease, the disease is complicated by atrial fibrillation, and in patients with mitral heart disease who require surgical treatment, atrial fibrillation develops in 60-80% of cases. Observations indicate a significant increase in the incidence of this arrhythmia.
In patients with atrial fibrillation, mortality is approximately 2 times higher than in patients with sinus rhythm. Dissociation of the atria and ventricles leads to a decrease in cardiac output by 20-30% due to the lack of atrial contribution to cardiac output, as well as inadequate filling of the left ventricle with blood. Thus, long-term atrial fibrillation leads to the development of dilated cardiomyopathy, which is accompanied by dilation of the cavities of the heart, severe systolic dysfunction of the left ventricle (decreased ejection fraction), the occurrence of mitral and tricuspid regurgitation (reverse reflux of blood), which leads to an increase in heart failure.
The presence of atrial fibrillation leads to blood stagnation and thrombus formation in the left atrial appendage with a high risk of blockage of the arteries of the brain, the main arteries of the upper and lower extremities (systemic circulation), and the vessels supplying internal organs. Every sixth stroke occurs in a patient with atrial fibrillation. The risk of such a complication in patients with atrial fibrillation is 5 to 7 times higher than in people without arrhythmia. In patients with heart defects of rheumatic etiology, complicated by atrial fibrillation, the risk of developing acute cerebrovascular accident (ACVA) is 17 times higher than in patients without atrial fibrillation.
Diagnostics
The main method for diagnosing atrial fibrillation is electrocardiography (ECG) and Holter monitoring - continuous long-term (for 1 - 7 days) ECG recording.
If the diagnosis of AF is confirmed and indications for endovascular catheter ablation of AF are determined, the patient undergoes an electrophysiological study (EPS) to identify zones of ectopic foci and construct a map of these zones.
Complications of the disease
In atrial fibrillation, the upper chambers of the heart are not fully filled with blood, causing reduced output and heart failure.
WPW syndrome with early excitation of the ventricles provokes the development of supraventricular arrhythmia, worsening the course of the disease and making it difficult to diagnose cardiac arrhythmias.
In addition to reducing the blood filling of the cavities of the heart, the chaotic contraction of the atria forms clots and thrombi, which, with the blood flow, enter the small and large vessels of the brain. Thromboembolism is dangerous due to complete closure of the arteriole and the development of ischemia, which requires resuscitation measures and initiation of treatment as soon as possible.
Treatment
Conservative treatment of atrial fibrillation (atrial fibrillation)
Atrial fibrillation is a risk factor for ischemic stroke, which develops as a result of the formation of blood clots in the cavity of the left atrium. The first-line treatment for atrial fibrillation is drugs that prevent blood clots. They are prescribed by a doctor, because... monitoring of the blood coagulation system is required. These drugs are indicated for almost all patients who suffer from atrial fibrillation, regardless of whether the arrhythmia is constantly present or occurs in attacks (paroxysmal form of arrhythmia). The risk of stroke is the same both in the presence of a chronic form of arrhythmia and in a paroxysmal form of arrhythmia.
In patients with paroxysmal atrial fibrillation, the issue of preventing the occurrence of arrhythmia attacks is addressed. If the attack occurs for the first time, antiarrhythmic drugs are not prescribed. Medications may be recommended to control heart rate and improve tolerance to repeated episodes of arrhythmias. Antiarrhythmic drugs are also not prescribed if the patient’s arrhythmia attacks are asymptomatic and do not reduce his quality of life. If rhythm disturbances recur and paroxysm tolerance deteriorates, the cardiologist-arrhythmologist, together with the patient, decides on the prescription of antiarrhythmic drugs or surgical treatment of arrhythmia (catheter ablation).
If a prolonged attack of atrial fibrillation develops, which does not go away on its own, it is necessary to contact a specialist cardiologist-arrhythmologist, who will choose the most suitable method for stopping the arrhythmia for the patient. A technique for medicinal restoration of normal heart rhythm has been developed, as well as a procedure for restoring rhythm using electrical cardioversion. To restore the rhythm, a certain medication preparation is necessary, the regimen of which will be determined by the doctor, based on the individual characteristics of the course of the disease. With the advent of the latest highly effective antiarrhythmic drugs, preference is given to drug restoration of rhythm.
When transforming the paroxysmal form of atrial fibrillation into a chronic form, the main task is to control the heart rate. In the presence of tachysystole (high heart rate), drugs are prescribed that reduce the heart rate, the primary of which are beta-blockers. An integral part of the treatment of atrial fibrillation is the treatment of the disease that provoked the rhythm disturbance - coronary heart disease, heart failure, arterial hypertension, disorders of the thyroid gland and others.
It is necessary to contact a cardiologist-arrhythmologist if:
- development of an attack of atrial fibrillation for the first time in life,
- development of another attack of arrhythmia that cannot be controlled by usual means,
- ineffectiveness of previously prescribed antiarrhythmic therapy.
Causes of development and risk factors
Cardiac pathology
- AMI (impaired conductivity and excitability of the myocardium).
- Arterial hypertension (LA and LV overload).
- Chronic heart failure (impaired myocardial structure, contractile function and conductivity).
- Cardiosclerosis (replacement of myocardial cells with connective tissue).
- Myocarditis (structural disorder due to inflammation of the myocardium).
- Rheumatic diseases with damage to the valves.
- SU dysfunction (tachy-brady syndrome).
Extracardiac pathology
- Diseases of the thyroid gland with manifestations of thyrotoxicosis.
- Drug or other intoxication.
- Overdose of digitalis preparations (cardiac glycosides) in the treatment of heart failure.
- Acute alcohol intoxication or chronic alcoholism.
- Uncontrolled treatment with diuretics.
- Overdose of sympathomimetics.
- Hypokalemia of any origin.
- Stress and psycho-emotional stress.
Age-related organic changes.
With age, the structure of the atrial myocardium undergoes changes. The development of small focal atrial cardiosclerosis can cause fibrillation in old age.
Doctor's advice
I think there is no need to talk about lifestyle modification, which can reduce the risk of obesity, diabetes and arterial hypertension. But many people forget that, having a family history of arrhythmia, it is necessary to promptly treat all diseases of the lungs and bronchi, choose a profession wisely, avoiding work with a high content of dust in the air (for example, the mining industry). This will reduce the risk of fibrillation associated with COPD.
Diagnostic methods
First you need to determine your individual risk of stroke:
Determination of stroke risk during primary* (if no previous stroke) prevention (J Am Coll Cardiol 2001;38:1266i-1xx).
| Source | High risk | Medium risk | Low risk |
| Atrial Fibrillation Investigators (1)** | Age 65 years and older History of hypertension Diabetes | Age younger than 65 years No high-risk features | |
| American College of Chest Physicians (2) | Age over 75 years History of hypertension LV dysfunction *** More than 1 moderate risk factor | Age 65 - 75 years Diabetes IHD Thyrotoxicosis | Age under 65 No risk factors |
| Stroke Prevention in Atrial Fibrillation (3) | Women over 75 years of age Systolic blood pressure more than 160 mm Hg. Art. LV dysfunction** | History of hypertension No high-risk features | No high-risk features No history of hypertension |
Obtaining required data
Studying the patient's medical history and complaints. It is necessary to find out the specific symptoms that manifest atrial fibrillation, determine its clinical form, the date of appearance of the first signs, the frequency and duration of paroxysms, determine the predisposing factors and provoking diseases, and the effectiveness of the treatment.
Carrying out ECG, EchoCG. These examinations make it possible to determine the type of heart rhythm disturbances, assess the size of the heart chambers and the condition of the valves, and changes in myocardial contractility.
Blood test. To determine the function of the thyroid gland (T3, T4) and pituitary gland (TSH), to identify a lack of electrolytes (potassium) and signs of acute rheumatism or myocarditis.
Getting More Data
Holter monitoring ECG. 24-hour ECG recording allows you to monitor and evaluate heart rate at different times of the day (including sleep) during the patient’s normal daily routine, and to record attacks of AF.
Record AF paroxysms online. This type of Holter monitoring allows you to record electrocardiogram signals transmitted by telephone directly at the time of an attack.
Bicycle ergometry, treadmill test and other stress tests. These methods are used in cases where adequate control of heart rate is not established (in chronic AF), to provoke arrhythmia caused by exercise, as well as to exclude cardiac ischemia before treatment with class 1C antiarrhythmics.
Transesophageal echocardiography. This test helps identify the presence of a thrombus in the left atrium before cardioversion.
Electrophysiological study. EPI is performed to explain the mechanism of tachycardia, identify and surgically treat predisposing arrhythmia (radiofrequency ablation).
Prevalence in society
Tachysystolic form of atrial fibrillation, which is the most common, occurs in 3% of adults aged 20 years and older. Moreover, older people suffer from the disease to a greater extent. This trend is explained by several factors:
- increasing life expectancy;
- early diagnosis of asymptomatic forms of pathology;
- the development of concomitant diseases that contribute to the appearance of atrial fibrillation.
According to the World Health Organization, in 2010 the pathology was detected in 33.5 million people on the planet.
It was found that the risk of getting sick in women is slightly lower than in men. But at the same time, the former are more often susceptible to strokes, have a greater number of concomitant diseases and a pronounced clinical picture of fibrillation.
Clinical case
Patient A., 25 years old, was brought to the emergency department with complaints of lack of air, inability to breathe deeply, palpitations, dizziness, and severe general weakness.
The patient was engaged in semi-professional powerlifting, and during the next approach he lost consciousness. In the family, the grandmother and mother were diagnosed with atrial fibrillation. Objectively: the skin is pale, shortness of breath at rest, blood pressure is 90/60 mm Hg, heart rate on auscultation is 400 beats/min, the first tone is also heard louder than normal, the rhythm is irregular, the pulse on the radial artery is 250 beats/min. Preliminary diagnosis: “Newly diagnosed atrial fibrillation.” To confirm the diagnosis, the following were used: clinical blood and urine tests, determination of TSH levels, ECG, Echo-CG. The patient underwent pharmacological cardioversion with Dofetilide, after which sinus rhythm was restored with a heart rate in the range of 60-64 beats/min. During the hospital stay, 24-hour ECG monitoring was carried out, and no paroxysms of fibrillation were observed. The patient was advised to limit physical activity.