Description of hypertension
Hypertension is a widespread pathology of the cardiovascular system, which is characterized by a persistent or transient increase in arterial (blood) pressure.
Today, medicine knows that hypertension is a systemic disease that affects many human organs.
At the onset of the disease, an increase in blood pressure (blood pressure) may not affect the patient’s condition. Depending on the severity of the process, hypertension can cause destruction in the structures of the heart muscle, brain, kidneys and eyes.
Degrees of hypertension and risk groups
There are three degrees of severity of hypertension:
- Hypertension of the 1st degree (mild form).
- Hypertension of the 2nd degree (hypertension of moderate severity).
- Hypertension of the 3rd degree (the most severe degree).
The severity of hypertension is always determined together with risk factors for the development of possible complications from the cardiovascular system.
Based on these factors, the cardiologist predicts hypertension.
There are four risk groups for hypertension:
- risk 1 (lowest)
- risk 2 (medium)
- risk 3 (high)
- risk 4 (very high).
Accurate determination of the type of hypertension is of great therapeutic importance. Lack of adequate treatment for hypertension can cause the development of a hypertensive crisis.
About medical examination
Clinical examination in the field of cardiology is one of the main measures to reduce mortality from cardiovascular diseases. There is a clearly defined concept of risk factors that must be controlled and treated for a long and fulfilling life. Therefore, clinical examination including cardiac examination is indicated for all men over 40 years of age and women over 50 years of age.
Symptoms of hypertension
Signs of the disease may manifest themselves differently depending on the stage at which hypertension occurs.
Symptoms that are most often observed with hypertension:
- headaches and dizziness of various types
- feeling of heaviness and pulsation in the back of the head
- cardiopalmus
- general weakness
- problems with coordination of movements (sometimes)
- intolerance to loud sounds
- photophobia
- nosebleeds
- nausea
- feeling of fear.
If symptoms appear, make an appointment with a cardiologist to diagnose and treat a possible disease.
How is diagnosis carried out?
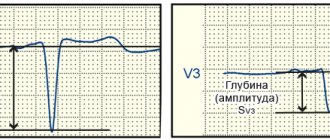
To make a diagnosis of stage 3 hypertension, risk 3, regular blood pressure measurements are required, as well as laboratory tests of the patient’s blood and urine. You cannot do without instrumental diagnostic techniques, such as ultrasound, Dopplerography, ECG.
And also read on our website: Causes, main symptoms and treatment of hypertension in men
All these measures allow the doctor to assess the condition of the target organs and determine the extent of their damage. Sometimes I need additional consultation with an ophthalmologist and endocrinologist.
Diagnosis and treatment of hypertension
Diagnosis of the disease
Diagnosis of hypertension at the A-Media clinic is carried out using the following methods:
- blood pressure measurement
- ECG
- 24-hour ECG monitoring with blood pressure (Holter monitoring)
- echocardiography (echocardiography or ultrasound of the heart)
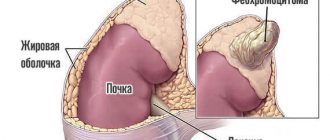
- Ultrasound of the abdominal cavity with kidneys
- Ultrasound Dopplerography of the BCA (ultrasound Dopplerography of brachiocephalic arteries and veins).
Treatments for hypertension
Treatment of hypertension in our clinic is planned by a qualified cardiologist only after an accurate diagnosis has been made.
First step: Our doctor will take measures to lower the patient's blood pressure.
Further therapy is planned individually based on the type of hypertension. Mild and moderate forms of the disease can be treated with medications. For severe hypertension, antihypertensive drugs are always prescribed. Lifestyle modification is a prerequisite.
What is it and what does it mean?
Stage 3 hypertension is a severe, no longer curable form of the disease.
It is not realistic to restore normal pressure levels, nor is it possible to restore the full functioning of target organs affected by constant arterial hypertension. The diagnosis is made if the patient's blood pressure regularly rises above 180 to 110 mm Hg. Art.
Stage 3 hypertension does not appear suddenly; it progresses over the years and affects more and more organs. All doctors can do is maintain a person’s vitality and stop the development of new complications. The patient needs not only to regularly use potent medications, but also to eliminate all possible provoking factors that affect the condition of the target organs.
A cardiovascular risk of 3 indicates that more than 20% of the blood vessels in the body are already affected.
Prevention of hypertension
To prevent hypertension and possible complications of this disease, the cardiologist at the A-Media clinic recommends taking the following measures:
- quit smoking
- minimize alcohol consumption
- control body weight
- be sure to get eight hours of sleep
- establish proper nutrition
- engage in physical activity daily.
Contact the A-Media clinic for the treatment of hypertension, and our experienced cardiologist will help you avoid severe complications of this disease and significantly improve your quality of life.
Getting a disability
Due to the fact that stage 3 hypertension is associated with severe dysfunction of vital organs and entails a limitation in the ability to self-care, patients are assigned group 1 disability.
It can only be obtained after a medical and social examination. It is carried out on the basis of a medical institution in which hypertensive patients are observed.
When a disability is assigned, they are shown pension payments and corresponding benefits.
People in the first group are completely disabled or can only work in specially created conditions.
Epidemiology
Cardiovascular (CV) diseases are a serious health problem worldwide due to their high prevalence and high mortality rate. In the world, about a third of all deaths occur from diseases of the circulatory system (85% of them due to heart attack or stroke), more than 75% occur in countries with low and medium levels of economic development. In Russia, the incidence of CVD is more than 19% in the structure of all diseases, mortality is 50%. Experts from the World Health Organization (WHO) predict a further increase in morbidity and mortality from CVD.
People of retirement age are more susceptible to vascular and heart diseases, but over the past decades these diseases have become significantly younger. Thus, coronary heart disease is often first diagnosed at the age of thirty, and from the age of forty it becomes the cause of premature death. Morbidity statistics show that in men the incidence and mortality from cardiovascular pathologies is 1.5 times higher than in women.
Today, in the section “Health School for Patients with Arterial Hypertension,” we will talk to you about groups at high cardiac risk and the main activities that lead to reducing the risk of developing cardiovascular diseases.
Large-scale scientific studies show that in certain categories of people the total cardiovascular risk may be high. This:
1. Persons with arterial hypertension.
2. People with excess body weight (obesity).
H. Persons with high levels of “bad” cholesterol.
4. Smokers.
5. Persons exposed to chronic stress and leading a sedentary lifestyle.
6. Persons with diabetes mellitus (including latent diabetes).
7. Persons with a family history of myocardial infarction, stroke, diabetes mellitus.
8. Age (starting from 30 years), the risk increases by 2% every year.
9. Male gender (up to 55 years old) in men the cardiovascular risk is higher, after 55 years old and in women it increases sharply.
10. Presence of angina or myocardial infarction in the past.
WHAT TO DO IF THE RISK IS HIGH OR VERY HIGH?
If the cardiovascular risk turns out to be high, then, first of all, it is necessary to find out the reason. The determining role is played not only by the number of risk factors, but also by their nature.
Are all risk factors equally dangerous? According to many years of research, the risk factors have the following order of importance: high levels of total cholesterol, low levels of “good” cholesterol, smoking, stress/depression, high blood sugar, hypertension, obesity, alcohol abuse, sedentary lifestyle and low consumption of vegetables and fruits. By addressing these risk factors (which is achievable), we can significantly reduce our overall cardiovascular risk. In real conditions, these risk factors occur in isolated form only in 10% of cases; more often they are combined. This circumstance requires an integrated approach when assessing the general or total cardiovascular risk. The risk scale can be used not only to determine risk, but also to assess the effectiveness of measures taken.
For clarity, let's return to the above example. A 50-year-old man had a high risk of death from cardiovascular diseases - 7%, which is due to high cholesterol levels (20% above normal), smoking (10-15 cigarettes per day), high blood pressure (150/100 mm Hg). Art.), as well as hereditary burden. Age, gender and heredity are factors that cannot be changed. However, a decrease in cholesterol levels by 20%, blood pressure to 140/90 mm Hg. Art. and stopping cigarette smoking will reduce the overall risk to two percent. What if we only lowered our blood pressure levels? The risk would then drop to 5%, which is also considered high.
Thus, despite the presence of two irreducible risk factors (middle age and poor heredity), by lowering blood cholesterol levels, blood pressure and stopping smoking, the total cardiovascular risk can be reduced by 3 times.
WHAT TO DO NEXT?
With the help of modern medications and compliance with non-drug measures, the rate of development of cardiovascular diseases can be reduced in a relatively short time (7-8 weeks). However, we can count on positive results only if we can maintain the achieved effect for a long time (years). To do this, it is necessary to visit a doctor regularly (once every 3 months) on an outpatient basis and undergo examinations.
WHAT BENEFITS DO WE GET BY FOLLOWING A CORRECT LIFESTYLE?
The term “lifestyle change” refers to a whole range of activities, including changing eating habits, dieting, regular exercise, quitting smoking, limiting alcohol and increasing stress tolerance.
Each of these measures leads to a reduction in the risk of developing cardiovascular disease. However, taken together, their power is much more significant, in some cases even comparable to the effectiveness of drugs. For example, following a diet (limiting animal fats, sugar and other easily digestible carbohydrates, table salt and alcohol) and daily 30-minute physical activity for 6 months leads to a decrease in body weight by 11%, cholesterol levels by 13% and blood pressure by 7 %. According to foreign studies, long-term implementation of these recommendations can reduce the risk of myocardial infarction by 42% and diabetes mellitus by 58%.
Basic principles of a healthy lifestyle: 1. It is recommended to have 3 main meals and 2 intermediate meals with the following distribution of food intake: breakfast - 25%, second breakfast - 100%, lunch - 35%, afternoon snack - 10%, dinner - 20%. Common types of poor eating habits include eating late in the evening, overeating (skipping the next meal contributes to overeating), eating too large portions and taking in excess calories from liquid foods, and eating foods high in salt and fat.
2. To reduce cholesterol levels, it is necessary to limit the consumption of foods containing saturated fats and include fiber in the diet. Reducing cholesterol levels is achieved by reducing the consumption of fatty cheeses, milk (fat content 2.5% and above), sour cream (fat content above 10%), butter, heavy margarines, mayonnaise, lard, duck meat, goose, chicken skin, eggs yolk, sausages, meat with visible fat, liver, brain and kidneys of animals. Fiber is a product containing fibers that enhance the elimination of neutral stearins and moderately reduce cholesterol levels. You need to consume at least 25 g of fiber per day, which is found in wholemeal bread, oats, and legumes (peas, beans, lentils). Limiting salt to 4 g per day helps lower blood pressure levels. For high blood pressure, it is recommended to consume potassium and magnesium, the sources of which are tomatoes, prunes, oranges, dried apricots, and legumes. In the diet, the main proportion of carbohydrates should be complex carbohydrates (vegetables and fruits), and easily digestible carbohydrates (refined sugar, biscuits, chocolates and drinks) should be limited.
3. For hypertension and high cholesterol levels, it is necessary to limit alcohol intake (no more than 50 g of vodka or 150 g of dry red wine per day).
4. The selection of physical activity should be individual, taking into account age, gender and concomitant diseases. Dynamic loads are recommended 3-4 times a week, at least 20-30 minutes a day.
These include walking, brisk walking, swimming, skiing and cycling. Typically, the intensity of physical activity is determined by heart rate, the normative values of which are different for each age. For example, up to 40 years of age, the permissible increase in heart rate is 110-140 beats per minute, at 40-49 years old - 105-130 beats per minute, at 50-59 years old - 100-125 beats per minute and over 60 years old - 95-115 beats. in a minute.
5. Often smokers reason like this: “As long as I’m healthy, why not smoke? And when there is already an illness, it’s too late to change something...” Indeed, does it make sense to give up cigarettes when a person is still healthy or, on the contrary, has been seen by a cardiologist for a long time? Yes, I have!
So, we have briefly listed the basic principles of a healthy lifestyle. As you noted, these measures are safe, cost-effective, and they naturally reduce the risk of cardiovascular complications. However, lifestyle changes alone cannot always reduce the total cardiovascular risk to a safe level. This especially applies to people with high and very high cardiovascular risk, in whom, as a rule, cholesterol is increased by 20% or higher and/or blood pressure exceeds normal by 15% or higher, etc. In this case, along with lifestyle changes, taking medications is necessary. The possibilities of modern cardiology are enormous. The arsenal of modern medicine has a sufficient number of drugs with proven effectiveness in reducing the risk of cardiovascular complications and high safety during long-term use. To reduce the overall cardiovascular risk, medications must be taken systematically and over a long period of time. The choice and prescription of drug therapy is carried out only by a doctor!
REMEMBER!
Timely identification and reduction of cardiac risk helps to prolong life and significantly improve its quality. The following are the normal values for the main risk factors:
* Arterial pressure
* Total cholesterol level
* Level of "bad" cholesterol
* Good cholesterol level >1 mmol/l (40 mg/dl)
* Fasting blood sugar
* Body mass index
* Waist circumference
Only maintaining the level of risk factors within these limits can guarantee the safety of the risk of developing cardiovascular complications.
IF THE DOCTOR PRESCRIBED YOU WITH ASPIRIN CARDIO
The presence of cardiovascular risk factors, such as arterial hypertension, diabetes mellitus, coronary heart disease, atherosclerotic vascular damage and others lead to a change in blood clotting ability towards increased thrombus formation. Increased thrombus formation is the main cause of severe disabling and life-threatening conditions, such as cerebral stroke and myocardial infarction.
Aspirin Cardio is a drug of acetylsalicylic acid, which was invented and produced by the German company Bayer. Its unique properties, effectiveness and safety have been confirmed in large international studies, unlike other acetylsalicylic acid preparations.
Taking Aspirin Cardio daily at a dose of 100 mg or every other day at a dose of 300 mg will help avoid severe cardiovascular complications.
Acetylsalicylic acid can cause irritation and damage to the gastric mucosa. To prevent these complications, a special enteric coating has been developed, which provides stomach protection during long-term use.
Classification of CVD
The most common, socially significant CVDs include:
- Hypertension is a persistent increase in blood pressure.
- Atherosclerosis is the blocking of the arterial lumen by cholesterol plaques. Damage to the coronary vessels leads to coronary heart disease, the arteries of the head and neck to ischemia (lack of blood supply) to the brain, and large arteries of the legs to ischemia of the limb.
- Coronary heart disease is a disorder of the blood supply to the myocardium caused by obstruction (narrowing of the lumen) of the coronary arteries. The acute form of the disease is myocardial infarction.
- Cardiac arrhythmias are disturbances in heart rhythm and conduction.
- Inflammatory heart diseases are lesions of an autoimmune or infectious nature that affect the pericardial sac, muscle layer or internal connective tissue lining of the heart - pericarditis, myocarditis, endocarditis, respectively. Rheumatic carditis is most often recorded.
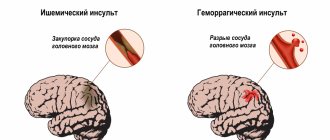
- Cerebrovascular pathologies are diseases of the blood vessels of the brain. An acute form of circulatory disturbance in the great vessels of the head and neck is ischemic stroke (cerebral infarction). If the integrity of the vascular wall is damaged or incompetent, a hemorrhagic stroke (bleeding in the brain) develops.
- Thromboangiitis obliterans is a progressive closure of the small arteries of the legs (first due to spasm, then associated thrombosis), accompanied by ischemia of the limb.
- Venous thrombosis and pulmonary embolism (PE) are complete or partial closure of the lumen of the veins or the main artery responsible for the blood supply to the lungs with a blood clot.
Significantly less common:
- congenital and acquired heart defects;
- heart tumors;
- systemic vasculitis;
- thromboembolism of the arteries of the systemic circulation (peripheral, mesenteric and others).