Varicocele is a common urological disease in which a man experiences dilatation of the veins of the pampiniform plexus of the spermatic cord of the testicle. As a rule, the pathology occurs in men who have a predisposition to varicose veins. The weakness of the venous wall is genetically determined, so patients with varicocele very often have concomitant venous diseases - varicose veins and hemorrhoids.
Dilation of the veins of the testicle interferes with the normal outflow of blood, which can result in complete atrophy of the testicle over time. In many men with varicocele, due to impaired spermatogenesis, the spermogram has deviations, from minimal abnormalities to the complete absence of living, motile sperm suitable for fertilization. Therefore, treatment of varicocele is important in the prevention of male infertility.
Varicocele cannot be treated conservatively; the man requires surgery.
There are several options for the operation:
- Ivanissevich operation - through inguinal access;
- Marmara operation - through an infrainguinal incision;
- retroperitoneal access;
- laparoscopic clipping;
- transvenous embolization.
Marmara operation for varicocele
It is considered the most effective among the possible options. Compared to other types of surgical intervention, it has the lowest percentage of relapses and the minimum number of complications. This is a low-traumatic operation that is safe for neighboring tissues. Microsurgical intervention is performed through a small incision in the projection of the inguinal canal, mobilizes the spermatic cord and ligates the dilated veins. A cosmetic suture is applied, and after a few hours the patient can go home.
Contraindications
Contraindications may be the same factors as for all abdominal operations:
- poor blood clotting;
- the presence of other chronic diseases that prevent interventions with retroperitoneal access;
- poor general condition of the patient, interpreted as serious.
Note. Surgery may be delayed for boys if there is a grade 1 varicocele that is not painful.
In some cases, surgical treatment may be delayed or not performed at all, which is not associated with contraindications, and the postponement of surgical intervention is associated with reinsurance against possible complications or there is simply no urgent need for it. The table briefly names and explains the reasons for not performing the operation.
Reasons why surgical correction is not performed
| Cause | Short description | |
| Presence of contraindications | Blood pathologies or general poor condition preventing surgical treatment. |
|
| Little age | In the presence of the first degree of varicocele, a stable course of the disease without pain, surgery is postponed due to the significant risk of relapse in children. |
|
| Fertility is not relevant | There is no urgent need to perform the operation on adults or elderly men who already have children and do not want to have more, provided that the varicocele is of the first degree and there is no discomfort. |
|
If a decision is made not to undergo surgical treatment, the patient should be under constant observation. The patient receives detailed instructions on the use of drug therapy aimed at stabilizing the disease and maintaining spermatogenesis in proper condition.
In addition, there are a number of preventive restrictions, for example, a ban on lifting weights or avoiding significant physical activity (see Is it possible to play sports with varicocele).
Medicines are prescribed not for the treatment of varicocele, but to stabilize the disease during a delay
Methodology
Immediately before therapy, several preparatory measures should be taken:
- take blood tests (general, glucose and coagulability), urine;
- remove hair on the abdomen in the area of the future incision, if any.
Technique
Varicocele surgery according to Ivanisevich for adults is performed under local anesthesia; for children, general anesthesia is possible. The patient lies on his back, the surface of the skin is pre-disinfected and treated with an antiseptic.
The doctor performs a horizontal dissection of the left side (not exceeding 4-6 cm) of the peritoneal wall in the iliac region at the level of the anterior superior iliac spine parallel to the course of the inguinal canal. The incision itself is almost identical to the one made when removing the appendix, but not on the right, but on the left side.
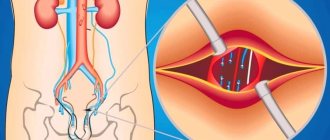
Now that the incision is made, the surgeon uses special hooks to push apart the layers of muscle tissue to access the testicular veins in the retroperitoneal space, as shown in the photo. As a rule, finding an inflamed vein is not difficult, but in the case of loose varicocele or when eliminating a relapse, finding varicose vessels can be difficult.
Photos of affected vessels
When the necessary veins are found, they are mobilized, taken on thread holders, ligated in the right places and crossed between two vein ligatures, and it is advisable to find all the additional branches extending from it and do the same actions with them.
After completing manipulations with varicose veins, they are placed in place, the incision is sutured tightly in layers, a sterile bandage is applied to the seams, which is not changed for the first two days. The duration of the entire operation usually does not exceed an hour and averages 40 minutes.
Complications
The likelihood of complications both during and after the operation is highest in comparison with other methods of varicocele removal used in modern medicine.
They arise for the following reasons:
- a technical error by the surgeon;
- technical difficulties.
Complications arise due to damage to adjacent tissues or blood vessels. There are cases when a doctor mistakenly cuts a completely healthy vessel, leaving veins affected by varicose veins untouched.
Let's name the most common complications:
- Damage to the iliac artery. Perhaps this can be called the most serious complication of all possible. This artery lies next to the testicular vein and is located at the same depth. If it is difficult to find an inflamed vein, the artery may be mistakenly verified as varicose and ligated. Accidental damage by tools is also possible;
- Injury to the lymphatic vessels is the cause of the manifestation of hydrocele already in the postoperative period;
- Damage or entrapment of a nerve. This is not a very dangerous complication, but its consequences are quite unpleasant. The consequences will be noticeable after the intervention and will manifest themselves in the form of pain in the groin area and numbness in some areas on the inner thigh.
Drug therapy
Treatment of varicocele involves the simultaneous use of medications (see Drug treatment of varicocele: review of medications), both before and after surgery. In the first case, these may be venotonics and drugs that stimulate spermatogenesis, and they continue to be taken during the recovery period.
For varicocele after Ivanisevich's operation, the following are prescribed:
- antibiotics to prevent the development of infections;
- painkillers;
- non-steroidal anti-inflammatory drugs;
- vitamins and immunomodulatory drugs;
- It is advisable to use tonic and strengthening dietary supplements.
Operation Ivanissevich
With this treatment option for varicocele, relapses are quite common, so Marmara surgery is preferable. Ivanissevich's operation is performed using an incision in the left iliac region about 5 centimeters long. The incision is quite deep and reaches the walls of the inguinal canal. The veins and spermatic cord pass through the inguinal canal. The doctor’s task is to ligate all dilated vessels.
If we compare the operations of Marmara and Ivanissevich, the first one is incomparably more effective and less traumatic, therefore it is preferable in modern realities. Often patients have to undergo repeat surgery to treat varicocele using the Marmara method after the Ivanissevich operation was unsuccessful.
Indications and contraindications for surgery
The only indication for this operation is varicocele - any degree of dilation of the veins along the spermatic cord of the testicles. But the need for intervention is determined by the attending physician based on the general clinical picture of the patient.
Surgeons argue about the time when surgery is necessary. Some experts recommend surgery at the earliest stages of the disease, because the longer it develops, the higher the risk of infertility. Others point out that infertility, in principle, accompanies the disease in most patients, regardless of its stage. In addition, surgery does not always improve sperm parameters. This means that there is no urgency in surgical intervention. But do not forget that each case is unique and only the attending physician can give an accurate recommendation.
The list of contraindications is small, but quite serious. Ivanissevich's operation is impossible if:
- the patient has severe pathology of one or more internal organs;
- there are acute infectious diseases;
- skin diseases, in particular in the area of surgery;
- have a urinary tract infection;
- there are blood pathologies.
Pathologies of internal organs are a contraindication until the patient’s condition becomes stable or a complete recovery occurs. As for skin lesions, the verdict is clear: before surgery, both the disease itself and its consequences must be eliminated.
Laparoscopic clipping for varicocele
Laparoscopic varicocelectomy has many advantages: cosmetic effect, short rehabilitation period and the ability to quickly return to normal life. But at the same time, there is a high risk of affecting the lymphatic pathways. To prevent this from happening, contrast is used.
The use of an endovideosurgical method for treating varicocele allows one to accurately assess the number of branches of the testicular vein and cut them off completely, leaving the artery intact.
Postoperative complications
As already mentioned, this technique has a high probability of developing relapses and complications. According to statistics, out of ten men who underwent surgery, at least three will encounter postoperative consequences of a different nature, and the likelihood of a relapse is estimated to be significantly higher (30-40%) than the manifestation of other postoperative complications.
Recurrence of varicocele
The occurrence of relapse is explained by the fact that the surgeon is not able to examine the entire vein because only a small section of it is accessible to him. At the same time, possible branches of the vessels, also affected by varicose veins and located outside the incision, remain invisible.
Under such circumstances, it is impossible to talk about a relapse, as such, in its pure understanding, but it would be more accurate to call it technical shortcomings or limited technical capabilities during surgery. There is another option when the veins remain unligated or, more precisely, only part of them is ligated, which occurs with the so-called loose varicocele.
The surgeon may not notice inflammation of the veins, since in a supine position some of them will be in a dormant state, especially if the lesion is not severe, and the doctor naturally does not have the opportunity to see them. Such vessels remain unligated.
After treatment, blood begins to circulate through them somewhat more intensely than before, and the re-development of varicocele occurs.
Complications
Complications do not refer to relapses, although often many do not share these concepts. When the integrity of nearby tissues is damaged, complications arise that are caused precisely by the surgical intervention and have nothing to do with the original disease.
When operating using the Ivanissevich method, complications are not frequent, but the following are still possible:
- hematomas and bleeding;
- dropsy of the testicle (hydrocele);
- disruption of the innervation of certain areas;
- secondary infection.
The mechanisms of occurrence of the first three complications have already been described above. The introduction of infection is explained by a violation of antisepsis both during surgery and when changing sterile dressings during dressings.
Schematic representation of a hydrocele
Gonadal vein embolization
We are talking about thrombosis of a damaged vein. A special catheter is inserted through a puncture of the vein in the thigh; it is gradually brought to the renal and then to the spermatic vein. Using contrast, the doctor determines which vessels need to be turned off. Using a catheter, a substance is injected that embolizes and “turns off” pathologically dilated veins.
Embolization requires virtually no downtime because the entire operation is performed through a small puncture. This is an effective and modern treatment method.
The choice of treatment method for varicocele depends on the patient’s wishes, his state of health, and the availability of medicine.
To receive treatment for varicocele at the highest level, contact the Urology Clinic named after R. M. Fronshtein of the First Moscow State Medical University named after I.M. Sechenov (State Urology Center). September 9, 2020
Akopyan Gagik Nersesovich - urologist, oncologist, doctor of medical sciences, doctor of the highest category, professor of the department of urology of the Federal State Autonomous Educational Institution of Higher Education First Moscow State Medical University named after. THEM. Sechenov
Clinic of Urology named after R. M. Fronshtein of the First Moscow State Medical University named after I.M. Sechenov invites you to an appointment with experienced urologists. To get an appointment with a qualified specialist, just fill out a short online application. Be sure to fill out all the fields, including a brief description of the symptoms (the “Information” column), specify whether you are interested in a secondary or primary appointment.
Pay attention to the “Attach file” button - it allows you to immediately send medical documents to the doctor in electronic form. This may include images, tests and other information that will be important to determine the diagnosis.
Still have questions? Call us by phone or! On a weekday, you can come for a consultation with a doctor within a few hours after filling out the online application. Do not delay visiting a specialist if you are concerned about your genitourinary health!
Preparation
When preparing for surgery for varicocele, the following studies are mandatory:
- blood and urine tests;
- ultrasound examination of the scrotum;
- spermogram;
- hormonal studies;
- coagulogram;
- infectious disease test;
- fluorography;
- ECG.
If the patient does not have chronic pathologies other than varicose veins, then an examination by a urologist, consultation with an anesthesiologist and a physician’s opinion are sufficient. If any diseases are detected, the patient is referred for additional consultation to an appropriate specialist.
Positive and negative aspects of this technique
For a long time, Ivanissevich’s operation remained practically no alternative for the removal of varicocele (not counting identical techniques, for example, Palomo), but in modern practice new, less traumatic methods of treatment have appeared using micro-access, magnifying imaging equipment, a computer and other innovations.
These operations are becoming increasingly popular, and classical abdominal interventions are gradually becoming a thing of the past. However, the simplicity and accessibility of surgery according to Ivanissevich keeps this method in the top of frequently used ones.
For the sake of objectivity, we will indicate the positive and negative aspects of such therapy, starting with the positive ones:
- The lowest price;
- A regular operating room is suitable for the intervention; there is no need for special equipment;
- The technique does not require special specialized training (unlike laparoscopy or sclerotherapy);
- Suitable for removing varicocele of any degree and regardless of the patient’s age.
However, the negative aspects significantly outweigh, which forces progressive clinics to abandon the use of this technique and switch to more effective methods for eliminating varicocele.
Among the main negative characteristics we highlight the following:
- Highly traumatic;
- Significant likelihood of developing postoperative complications or relapse (30-40%);
- Treatment requires hospitalization from 8 to 14 days, depending on the individual characteristics of the patient;
- Sutures are removed on the 8th day;
- Long rehabilitation period. Full recovery is possible no earlier than six months;
- Severe pain syndrome;
- The operation leaves a large scar (similar to an appendicitis scar).
The procedure is quite painful
Sclerotherapy for varicocele
This is a safe and minimally invasive method for treating varicocele. It involves the introduction of a sclerosant drug into the lumen of the testicular vein, which provokes sclerosis and fusion of the lumen of the vein. Because of this, the reverse venous blood flow to the testicle gradually stops. Surgery is usually performed under local anesthesia. First, the doctor makes a small skin incision measuring 0.5-1 cm in the area of the external inguinal ring. The patient must first strain, after which a thin catheter is placed into the dilated testicular vein. This catheter is carefully advanced a couple of centimeters up the inguinal ring.
Then the doctor proceeds with antegrade venography - first he injects a radiocontrast agent through a catheter into the vessel, after which he takes an X-ray. Then, under X-ray control, the urologist injects a sclerosant. When the substance enters the renal vein, the patient is again asked to strain, after which the catheter is removed and the vein is ligated and crossed. This operation can be performed on an outpatient basis. The procedure is considered effective and reliable, since the risk of relapse of the disease after it is 9%.
Microsurgical testicular revascularization
The purpose of this operation is microsurgical revascularization of the testicle, during which normal blood flow through the testicular vein is restored. This operation is performed under general anesthesia. The doctor first makes a small incision about 5-6 cm in size in the lower abdomen. Then the testicular vein is isolated along its entire length from the testicle to the point of its confluence with the renal vein. At the same time, a small section of the epigastric vein is isolated from the venous plexus. Then the testicular vein is completely removed, after which the epigastric vein is sutured in its place. This operation is considered the most effective, since after it is performed, blood circulation in the scrotum is restored immediately, and not after a whole week. Due to this, the risk of postoperative complications such as hydrocele is minimal.
Analogs
There are a number of open abdominal surgeries very similar to the Ivanissevich treatment method that should definitely be mentioned.
Let us briefly indicate the name of such operations and their differences:
- Palomo. At the level of the inguinal ring, not only the inflamed veins are ligated, but also the testicular artery. The blood flow will not be impaired provided that the testis still has other sources of nutrition, for example, an artery running parallel to the vas deferens;
- Bernardi, named after Ivanissevich’s student in 1946. The essence is that the ligation of the testicular vein is performed slightly lower - at the level of the internal inguinal ring, while the artery is preserved.
All of these techniques are similar: a 4-6 cm incision is required, access to the veins is through a retroperitoneal approach. With a magnifying microscope, the access can be classified as a micro-access, which will provide higher accuracy and less trauma.
A noticeable scar remains after the intervention
Diagnosis and treatment tactics for varicocele:
Diagnosis of varicocele in our clinic may include examination, palpation tests, ultrasound examination of the scrotal organs, Dopplerography of blood vessels, and spermogram. Such an examination allows you to diagnose varicocele with 100% certainty, determine the extent of the disease and spermatogenesis disorders, and decide on the treatment method. Today, the main method of treating varicose veins is surgery. Indications for surgery are pain that is not amenable to symptomatic treatment, testicular atrophy and infertility. In some cases (1-2 degrees of varicocele, absence of pain and testicular atrophy, which is rare), therapeutic treatment is carried out aimed at identifying and eliminating the causes of varicocele.