Varicocele is an enlargement of the spermatic cord veins in men. Because of it, blood stagnates in the scrotum and the formation of healthy sperm is disrupted. Thus, varicocele often causes infertility. In 40% of men complaining of infertility, varicocele is responsible for it.
Statistics
Due to the anatomical features of the veins in the testicular area, varicocele most often forms on the left side. 80-95% are allocated to these cases. Right-sided testicular varicose veins are not so common (up to 8%). On both sides, varicocele occurs in 2-12 cases out of a hundred. Male disease is “linked” to the age of the patients. A large percentage (19) of problems with testicular veins are noted by doctors in adolescents. If we consider the reproductive age of men, then the statistics of varicose veins reach 35%. These are sad numbers, because... Varicocele in sexually mature men can cause infertility. Treatment of the disease should begin at the earliest stages.
What does it look like
A photo of a varicocele clearly demonstrates a male problem - the scrotum on one side (usually the left) is slightly lower. The skin covering the testicle does not hide the contours of the veins. When self-palpating the venous vessels, a man can feel their expansion. The patient may not even be aware of other symptoms of the disease. Palpation of the scrotum and visual examination are necessary actions for all men who care about their health. This is especially true for males planning fatherhood. You need to be regularly examined by a urologist. Medical examinations and consultations with qualified specialists are offered by the Global Clinic Center, which has extensive experience in the treatment of varicocele.
How does varicocele affect infertility?
Enlarged veins interfere with proper blood flow in the groin area, which disrupts thermoregulation in the testicles. For sperm to mature, a temperature below body temperature is required. Stagnation of venous blood leads to overheating, and germ cells develop poorly.
Another factor in the influence of varicocele on conception is the entry of immune system cells into the testicle. They mark the sperm as foreign and begin to attack them. This leads not only to the destruction of germ cells, but also to the development of an autoimmune disease with inflammation and deterioration of well-being.
History of the disease
Varicocele is a disease with deep historical roots. The first mention of the problem dates back to the 16th century and is associated with the name of Paré, a famous surgeon of the Renaissance. He drew attention to the pathology of the venous vessels near the male testicle. Many medical historians speak of the involvement of Hippocrates and Celsius in establishing the facts about this problem. The topic of varicocele is very closely related to infertility. In the 19th and 20th centuries, scientists confirmed the possibility of curing male infertility in direct proportion to the elimination of testicular varicose veins.
Varicocele. Symptoms
The danger of the first stages of the disease is that it is asymptomatic. The problem is discovered by chance, during medical examinations or when patients address other male issues (for example, in connection with infertility). Symptoms of varicocele characteristic of other degrees of the disease:
- nagging pain and discomfort in the left side of the scrotum, testicle and groin area;
- drooping left (mostly) testicle, interfering with walking;
- decrease in the size of the testicle on the left;
- manifestation of the contours of venous vessels;
- appearance of pain.
Varicocele is characterized by symptoms manifested in a decrease in the number of sperm and a decrease in their motility, in this case it is worth talking about male infertility. When doctors try to find out the cause of male infertility and analyze various symptoms in a patient, they often discover a varicocele, using the most modern diagnostic methods.
Consequences after vaccination against coronavirus
Talking about the consequences of coronavirus that can affect a person’s life in the future, one cannot help but mention the complications after vaccination against COVID-19. The vaccination campaign is gaining momentum. Despite the fierce debate among supporters for and against the coronavirus vaccine, vaccination statistics show that about 30% of the world's population has already been vaccinated.
How the vaccine works, whether you should be afraid of the consequences after vaccination against coronavirus and whether there are ways to protect yourself from complications - we will tell you further.
Coronavirus vaccine - consequences of vaccination
The injected drug familiarizes the immune system with the virus. In response to foreign invasion, the body launches immune defense. Therefore, the very first consequence of the coronavirus vaccine is swelling and redness in the injection area. This is a local reaction, it is caused by the rush of cells to the site of vaccine administration, the task of which is to prevent the spread of the disease throughout the body.
Next, the drug with the virus enters the blood. The body’s natural response is to “heat” the body to destroy the enemy, produce antibodies to fight it, and “memorize” the pathogen in order to quickly destroy it when it hits it again, preventing the development of the disease. Thus, a vaccinated person develops lasting immunity to COVID-19.
When the temperature rises, muscle weakness appears, and headache is a normal reaction. How long and how severe such consequences will appear after vaccination against coronavirus depends on the individual organism. The same infection (any kind at that) is tolerated differently by different people, so the drug itself has nothing to do with it. Often, after the vaccine is administered, no external manifestations or reactions are observed.
Vaccination against COVID-19: complications and contraindications
But do not confuse the reaction to the introduction of the vaccine with complications after vaccination against Covid. A complication is an unexpectedly serious condition that occurs after administration of the drug. Such conditions include anaphylactic shock (a sharp drop in blood pressure, cessation of oxygen supply to organs and tissues), the occurrence of convulsions, encephalitis and other serious conditions.
Similar reactions develop in those who have contraindications, but for some reason have undergone the vaccination stage. You cannot vaccinate if you have:
- chronic kidney pathologies; diseases of the cardiovascular, endocrine, hematopoietic systems; autoimmune disorders; pronounced pathologies of the central nervous system; severe allergic reactions with previously administered vaccinations.
If such pathologies are present, there is a high risk of complications after vaccination against Covid. Persons under 18 years of age, people over 65, and pregnant women cannot be vaccinated. For those who have recently suffered a severe form of coronavirus, it is also better to hold off on the vaccine, since after the illness there is an increased level of antibodies in the body. As a result of vaccination, their number will increase even more, which can cause a violent immune reaction in the body - the cytokine storm that we talked about above.
Causes and risk factors for the disease
In the veins surrounding the spermatic cord, a malfunction of the valve occurs, which prevents blood from flowing back. Instead of rising upward, the blood stagnates, because... is transmitted in the opposite direction. Because of this, the venous vessels become dilated and weak. The causes and risk factors of varicocele are associated with the appearance of primary and secondary reflux. The abnormal structure of the veins associated with congenital pathology leads to the complete absence of valves for the reverse outflow of blood or their atypical operation. During puberty, blood pressure on the vessels increases, and varicose changes occur in the veins near the spermatic cord. The weak walls of blood vessels inherited from birth by boys cannot cope with the flow of blood during physiological changes. As a rule, varicocele is inherited, so this should be taken into account in case of male infertility and comprehensive treatment of testicular varicose veins should be carried out. Secondary reflux occurs when the blood outflow valves stop functioning normally due to problems in the renal or vena cava. Varicose veins most often occur on the left side, because it is on the left that the venous vessels meet the renal vein. Narrowing of the lumen in the latter structure can cause varicocele. Unfavorable factors for testicular varicose veins:
- haemorrhoids;
- phlebeurysm.
The following are considered as a trigger for the appearance of varicocele:
- Hard physical labor.
- Extreme loads in sports or weight lifting.
- Lack of normal sex life.
- Professions that require long periods of standing.
- Chronic constipation.
Causes of the disease
Varicocele is one of the most common diseases among men, affecting 15 to 20% of the population. The risk group includes young people from 14 to 25 years old who lead an active lifestyle (sports, heavy physical work).
In addition, an increase in venous pressure may be a factor that contributes to the development of the disease.
ICD-10 divides varicocele into three stages. During the first, varicose veins cannot be determined by palpation, and for diagnosis it is necessary to do a special test - the Valsalva maneuver. At the second stage, dilated veins can be felt, but they cannot be visually noticed. And finally, at the last stage, varicose veins are clearly visible to the naked eye, and testicular atrophy occurs.
At first, varicocele is asymptomatic, but after some time it enters the open phase and is accompanied by periodic nagging pain in the scrotum area.
Complications
The main thing that patients suffering from testicular varicose veins need to understand is the serious situation with the appearance of offspring. Infertility can become a sad complication of varicocele, so you should not delay going to the clinic for diagnosis and treatment. Doctors from the Global Clinic Center can provide qualified assistance. Statistics show that patients diagnosed with varicocele in 60 cases out of a hundred are faced with the problem of sperm dysfunction. 40% of men with testicular varicose veins become infertile.
Varicose veins of the prostate gland in patients with varicocele
Kapto A.A.
The venous plexus of the prostate gland (Plexus venosus prostaticus, Santorini labyrinth) was first described by Santorini Giovanni Domenico (1681-1737) in 1724 [1]. This plexus, forming the dorsal venous complex, collects blood from the prostate gland (PG), the bottom of the bladder and seminal vesicles and flows into the internal iliac vein.
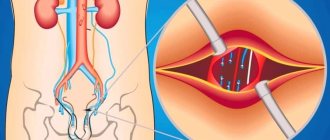
Pelvic venous congestion syndrome was first described by R. Gooch in 1831 in women [2]. Neurovascular bundles were described by PC Walsh and PJ Donker (1982) and are located on the dorsolateral surfaces of the pancreas between the rectum and pancreas [3]. It is believed that they do not belong to the venous plexus of the pancreas itself, although from our point of view this is not entirely correct and requires clarification (Fig. 1).
Rice. 1. Prostatic venous plexus and neurovascular bundles of the prostate gland
G.Z. Inaseridze identified two types of structure of the genitourinary venous plexus: reticular and concentrated (trunk) [4,5]. Later N.V. Kurennoy identified three types of structure of the genitourinary venous plexus: reticular; concentrated (main) and transitional [6]. O.S. Reiniger determined the prevalence of different types of structure of the genitourinary venous plexus during pelvic venography in 60 patients with benign prostatic hyperplasia: main - 53.3%, reticular - 33.3%, transitional - 13.3% of cases [7].
The syndrome of varicose veins of the pelvic organs occurs in various diseases: connective tissue dysplasia, portal hypertension, arteriovenous conflicts (Nutcracker syndrome, Posterior nutcracker syndrome, May-Thurner syndrome), tumor diseases (venous obstruction, arteriovenous fistulas) [8]. As is known, arteriovenous conflicts are the most common cause of varicocele.
The connection of varicocele with venous congestion of the pancreas was previously studied in the works of H. Sakamoto and Y. Ogawa, Y. Gat et al., A.I. Neumark et al., A.A. Capto [9-13]. Previously, we suggested that the anatomical vascular connection between the organs of the scrotum and the pelvic organs occurs in two ways: through the internal iliac vein, through the vein of the vas deferens (Fig. 2) [14].
Rice. 2. Anatomical connection of the organs of the scrotum and pelvis through the internal iliac vein (picture on the left) and through the vein of the vas deferens (picture on the right)
With retrograde phlebotesticulography with a 10-second delay, many researchers noted contrasting of the pericapsular area of the pancreas in patients with varicocele (Fig. 3) [15,16].
Rice. 3. Retrograde renal phlebotesticulography. Contrasting of the paraprostatic venous plexus on the side of the varicocele. On the left, discharge through the internal iliac vein predominates. In the middle and on the right, discharge through the vein of the vas deferens predominates
In continuation of the conducted research, in this work we made an attempt to determine quantitative criteria for varicose veins of the pelvic organs in men and propose a classification of varicose veins of the prostate gland.
MATERIALS AND METHODS OF RESEARCH
From September 2008 to September 2021, 206 patients with varicocele were examined and operated on. The examination of patients included a survey, physical examination, Ivanissevich test, semen analysis, ultrasound examination of the scrotal organs and transrectal ultrasound (TRUS) of the pancreas, color Doppler ultrasound of the pancreas at rest and during the Valsalva maneuver. Surgical treatment was carried out through a transscrotal approach along the Wesling line. Control examinations were carried out 3 and 6 months after surgery. Considering that the volume of the pancreas depends on the period of sexual abstinence, all ultrasound examinations were performed with the same period of abstinence - three days [17]. In cases of recurrent varicocele, magnetic resonance imaging of the inferior vena cava and pelvic vessels, retrograde venography of the renal and iliac vessels with phlebotonometry were performed.
RESEARCH RESULTS
The age of the patients ranged from 18 to 83 years and averaged 35.3 years. The diagnosis of varicocele was verified by physical examination, Ivanissevich test and scrotal Doppler ultrasound. Varicocele was left-sided in 131 (63.6%), right-sided in 3 (1.5%) and bilateral in 72 (34.9%) patients. When analyzing the ejaculate, pathospermia was found in 127 patients (61.7%), and an increased content of leukocytes (more than 1 million in 1 ml.) - in 148 patients (71.8%).
According to ultrasound of the scrotum, epididymal cysts were found in 112 (54.4%) patients. Combined pathology of the scrotal organs with varicocele was noted in 148 patients (71.8% of cases): bilateral varicocele, epididymal cyst, spermatocele, hydrocele, adhesions in the area of the epididymis and testicle, large hydatid of Morgagni, calculus of the inner lining of the testicle, lipoma spermatic cord. It was this circumstance that was the indication for the use of operative access along the Wesing line, in which it would be possible to simultaneously correct all identified problems from one incision.
According to TRUS of the pancreas, in all cases in patients with varicocele, visualization of the veins of the paraprostatic plexus on the side of the identified varicocele was noted. The classification presented in Table 1 was adopted as a working ultrasound classification of pancreatic varicose veins.
Table 1. Ultrasound classification of prostate varicose veins
| Stage | Definition of varicose veins | Maximum vein diameter, mm |
| 1 | Visible | 1- 4 |
| 2 | Significant | 5-10 |
| 3 | Expressed | > 10 |
The results of determining the stage of pancreatic varicose veins in 206 patients with varicocele are presented in Table 2.
Table 2. Prevalence of stages of prostate varicose veins in patients with varicocele
| Stage | Left-handed | Bilateral N=72 | Right-handed | Total N=206 | |
| N=131 | Left | On right | N=3 | ||
| 1 | 12 | 14 | 14 | — | 40 |
| 2 | 71 | 32 | 42 | 3 | 148 |
| 3 | 48 | 26 | 16 | — | 90 |
In all cases, the diameter of the veins of the prostatic venous plexus was positively correlated with the diameter of the veins of the right and left pampiniform plexus. In case of right-sided varicocele, according to TRUS data, dilatation of the veins of the paraprostatic venous plexus on the right was noted (Fig. 4).
Rice. 4. TRUS of the pancreas in patient M., 47 years old, with stage 2 right-sided varicocele. The volume of the pancreas is 35.0 cm3. The maximum diameter of the veins on the right is 3.5; 3.6 and 2.2 mm. Stage 1 varicose veins of the pancreas or visible varicose veins. Reticular type of venous plexus. BPH, chronic prostatitis. From the anamnesis, October 23, 2008, Ivanissevich surgery on the left
In most cases, patients had left-sided varicocele. At the same time, according to TRUS data, dilation of the veins of the paraprostatic venous plexus on the left was noted (Fig. 5).
Rice. 5. TRUS of the pancreas in patient L., 69 years old with left-sided varicocele stage 2. The volume of the pancreas is 16.5 cm3. The maximum diameter of the veins on the left is 6.0 mm. Stage 2 varicose veins of the pancreas or significant varicose veins. Main type of venous plexus. Chronic calculous prostatitis
With bilateral varicocele, dilation of the veins of the paraprostatic venous plexus on both sides was noted (Fig. 6).
Rice. 6. TRUS of the pancreas in patient K., 33 years old, with stage 3 bilateral varicocele. The volume of the pancreas is 22.3 cm3. The maximum diameter of the veins on the left is 10.9 and 18.3 mm, on the right 12.5 mm. Stage 3 varicose veins of the pancreas or pronounced varicose veins. Main type of venous plexus. Chronic calculous prostatitis
With a maximum vein diameter of 1 to 4 mm (visible varicose veins), the blood flow velocity in them was 1-3 cm/sec, and with the Valsalva maneuver - 5 cm/sec. With a maximum vein diameter of 5 to 10 mm (significant varicose veins), the blood flow velocity in them was 3-5 cm/sec, and with the Valsalva maneuver - 5-15 cm/sec. When the maximum diameter of the veins was more than 10 mm (pronounced varicose veins), the blood flow velocity in them was more than 5 cm/sec, and with the Valsalva maneuver more than 15 cm/sec (Fig. 7).
Rice. 7. Color Doppler TRUS of the pancreas in patient K. 42 years old with stage 3 bilateral varicocele. The diameter of the vein on the left is 14.3 mm, the blood flow speed is 5.9 cm/s (on the left). The blood flow velocity during the Valsalva maneuver is 17.4 cm/s (right). Severe varicose veins of the pancreas (stage 3)
In 93 patients (45.1% of cases), there were pronounced local changes in the pancreas in the form of foci of hypoechogenicity, fibrosis and calcification on the side of the varicocele. In 22 patients (10.7% of cases), TRUS revealed pancreatic cysts. We did not note any connection between the severity, localization of varicocele, severity of varicose veins of the pancreas and the size and localization of pancreatic cysts.
6 months after surgery, without any additional treatment, the following changes occurred in patients: 1) the diameter of the veins of the paraprostatic venous plexus on the side of the varicocelectomy decreased by 1.5 - 2.5 times in 175 patients (85.0%) (Fig. 8,9), 2) pathospermia remained in 88 patients (spermatogenesis was restored in 30.7% of cases), 3) pyospermia remained in 52 patients (disappeared in 64.9% of cases).
Rice. 8. TRUS of the pancreas in patient K., 30 years old with bilateral varicocele on 02/01/2016 (left) and 4 months (06/01/2016) after simultaneous bilateral varicocelectomy, plastic surgery of the testicular membranes according to Winkelmann from the midscrotal access along the Wesling line (from 02/09. 2016) (right)
Rice. 9. TRUS of the pancreas in patient Z., 40 years old with bilateral varicocele on 12/09/2015 (left) and 6 months (06/10/2016) after simultaneous bilateral varicocelectomy, excision of epididymal cysts of both testicles, plastic surgery of the membranes of the right and left testicle according to Winkelmann from the scrotum access via the Wesling line (from 12/22/2015) (right)
In the postoperative period, the development of recurrent left-sided and right-sided varicocele after left-sided varicocelectomy was noted in 5 patients (2.4%). A magnetic resonance imaging study of the inferior vena cava and pelvic vessels revealed MayThurner syndrome in all 5 patients (Fig. 10).
Rice. 10. Magnetic resonance imaging of the inferior vena cava and pelvic vessels in patients with recurrent varicocele. May-Thurner syndrome
All these patients underwent retrograde venography and phlebotonometry of the renal and iliac vessels. Phlebotonometry confirmed hypertension in the left internal iliac vein (pressure on average 31 mm Hg) and in the right internal iliac vein (pressure on average 27 mm Hg), which was 6-8 times higher than the average statistical norm. Phlebography revealed pronounced varicose veins of the paravesical and paraprostatic venous plexus due to May-Thurner syndrome (Fig. 11). All these patients underwent sclerotherapy of decompensated testicular veins.
Rice. 11. Retrograde venography of the left common iliac vein and selective venography of the left internal iliac vein in a patient with varicocele and May-Thurner syndrome. Severe varicose veins of the paravesical and paraprostatic venous plexus on the left
DISCUSSION
The criteria for varicose veins of the pelvic organs are currently determined based on the results of the following research methods: 1) ultrasound, 2) phlebography, 3) computed tomography (CT) or magnetic resonance imaging (MRI). These criteria have two features: they differ significantly from each other in assessing the diameter of dilated veins; describe varicose veins of the pelvis in women. Below we present a summary table 3, which presents the point of view of different authors on the criteria for pelvic varicose veins in women.
Table 3. Criteria for varicose veins of the pelvic organs in women
| Author | Research method | Vein diameter | Blood flow speed |
| Beard RW et al. (1984)[18]; Ignacio EA et al. (2008) [19] | Ultrasound | > 4 mm | < 3 cm/s |
| Inal M. et al. (2014) [20]; | Ultrasound | > 5-6 mm | ~ 3 cm/s |
| Ganeshan A. et al. (2007) [21]; | Ultrasound | > 6 mm | 3 cm/s |
| Leal Monedero J. et al. (2006) [22]; Barros FS et al. (2010) [23] | Ultrasound | > 7 mm | — |
| Black CM et al. (2009) [24]; Kim HS et al. (2006) [25]; Park SJ et al. (2004) [26]; Beard RW et al. (1984) [27] | Phlebography | > 5 mm | — |
| Kennedy A., Hemingway A. 1990 [28] | Phlebography | > 10 mm | — |
| Coakley FV et al. (1999) [29] | CT, MRI | Peri-uterine > 4 mm, ovarian > 8 mm | — |
Criteria for varicose veins of the pelvic organs in men A.Yu. Tsukanov and R.V. Lyashev considered dilation of the veins of the paraprostatic plexus to be more than 5 mm and/or the presence of blood flow reflux during the Valsalva maneuver during duplex angioscanning using a rectal sensor [30]. The criteria we proposed for varicose veins of the pelvic organs in men and the classification of this disease were based on measuring the maximum diameter of the veins of the paraprostatic plexus. We believe that venous dilatation is secondary to pathological blood flow and its duration, so measuring the maximum diameter of the veins can fairly accurately reflect the true state of the paraprostatic plexus veins. Considering that TRUS of the pancreas is a routine research method (in contrast to phlebography and phlebotonometry, CT, MRI), and based on the fact that the classification of varicose veins of the pancreas should have practical significance, we decided to base it on the results of ultrasound examination.
CONCLUSION
We have proposed an ultrasound classification of pancreatic varicose veins, which includes three stages: 1 - “visible varicose veins” with a maximum vein diameter of 1-4 mm, 2 - “significant varicose veins” with a maximum vein diameter of 5-10 mm and 3 - “pronounced varicose veins" with a maximum vein diameter > 10 mm. Our data indicate that the detection of dilated veins of the paraprostatic plexus according to TRUS may indicate the presence of varicocele and associated venous congestion of the pancreas. In all cases, pancreatic varicose veins were detected on the side of the varicocele and were ipsilateral in case of unilateral varicocele and bilateral in case of bilateral varicocele. 6 months after the operation, without any additional treatment, the diameter of the veins of the paraprostatic venous plexus decreased by 1.5-2.5 times in 85.0% and pyospermia disappeared in 65.0% of cases. This allows us to identify varicocele as one of the causes of pelvic disorders and prostatopathies associated with venous congestion. In case of recurrent varicocele, it is advisable to conduct a magnetic resonance examination of the inferior vena cava and pelvic vessels, phlebography and phlebotonometry of the renal and iliac vessels to confirm or exclude May-Thurner syndrome.
LITERATURE
1. Santorini GD Observationes anatomicae. Venice: Giovanni Battista Recurti, 1724; X: 193-194.
2. Gooch R. In: An Account of Some of the Most Important Diseases Peculiar to Women. Murray J, editor. London: Murray 1831: 1829 p.
3. Walsh PC, Donker PJ. Impotence following radical prostatectomy: Insight into etiology and prevention. J Urol 1982;128(3):492-497.
4. Inasaridze G.Z. Experimental data on ligation of the main veins of the bladder and clinical observations of similar changes in patients with pathology in the genitourinary venous plexus. Theses of the Ukrainian Congress of Urologists, Kyiv, 1939. P.78-79, 212-230.
5. Inasaridze G.Z. Extreme types of variability of the genitourinary venous plexus and their clinical significance: dissertation. Dr. med. Sci. M. 1940.
6. Kurennoy N.V. Details of the macroscopic structure of the urogenital venous plexus and their possible significance. Sat. "Issues of Urology". Kyiv, 1964. pp. 28-53.
7. Reiniger O.S. The role of the anatomical structure of the genitourinary plexus in the pathogenesis of bleeding after adenomectomy. Abstracts of reports of the IV Plenum of the All-Russian Scientific Society of Urologists. - M, - 1973, - P. 67-68.
8. Kapto A.A., Zhukov O.B. Varicose veins of the pelvis in men (literature review). Andrology and genital surgery. 2016; 17(2):10-19.
9. Sakamoto H, Ogawa Y. Is varicocele associated with underlying venous abnormalities? Varicocele and the prostatic venous plexus. J Urol 2008; 180(4):1427-1431. doi: 10.1016/j.juro.2008.06.048.
10. Gat Y, Gornish M. Reversal of Benign Prostate Hyperplasia by Super-selective Intraprostatic Androgen Deprivation Therapy. Euro Urol Rev 2009; 4(1):10-14.
11. Gat Y, Joshua S, Gornish MG. Prostate cancer: a newly discovered route for testosterone to reach the prostate: Treatment by super-selective intraprostatic androgen deprivation. Andrologia 2009; 41(5):305-315. doi: 10.1111/j.1439-0272.2009.00972.x.
12. Neymark A.I., Popov I.S., Gazamatov A.V. Features of microcirculation of the prostate gland and gonads in young men suffering from isolated varicocele and varicocele in combination with pelvic congestion. Experimental and Clinical Urology 2013; (2): 56-60.
13. Kapto A.A. The phenomenon of prostate varicose veins in patients with varicocele. Collection of abstracts of the 11th Congress of the Professional Association of Andrologists of Russia. May 25-28, 2021, Sochi, Dagomys. P.15-16.
14. Kapto A.A. Clinical aspects of vascular anatomy in patients with varicocele (lecture). Experimental and Clinical Urology 2006; (2):70-79.
15. Gat Y, Gornish M, Heiblum M, Joshua S. Reversal of benign prostate hyperplasia by selective occlusion of impaired venous drainage in the male reproductive system: novel mechanism, new treatment. Andrologia. 2008;40(5):273-81.
16. Osipov N.G., Teplinskaya N.P., Sabalenko Yu.A., Alekseychuk G.I. Changes in the architectonics of the veins draining the pampiniform plexus and spermatogenesis in patients with newly diagnosed and recurrent varicocele. Andrology and genital surgery 2014; (2):30-36.
17. Kapto AA.Value assessment of prostate tone in the complex treatment of patients with chronic prostatitis. Int Jmmunorehabilitation 2002; 4(2):316-317.
18. Beard RW, Highman JH, Pearce S, Reginald PW. Diagnosis of pelvic varicosities in women with chronic pelvic pain. Lancet 1984; 2:946-949.
19. Ignacio EA, Dua R, Sarin S, Harper AS, Yim D, Mathur V, et al. Pelvic congestion syndrome: diagnosis and treatment. Semin Intervent Radiol 2008; 25(4):361-8. doi:10.1055/s-0028-1102998.
20. Inal M, Karadeniz Bilgili MY, Sahin S. Nutcracker accompanying pelvic congestion syndrome; color doppler sonography and multislice CT findings: A case report. Iran JRadiol 2014;11(2):e11075 doi: 10.5812/iranjradiol.11075.
21. Ganeshan A, Upponi S, Hon LQ, Uthappa MC, Warakaulle DR, Uberoi R. Chronic pelvic pain due to pelvic congestion syndrome: the role of diagnostic and interventional radiology. Cardiovasc Inervent Radiol 2007; 30(6):1105-1111.
22. Leal Monedero J, Ezpeleta SZ, Castro FC, Senosiain LDC. Recidiva varicosa de etiologia pelvica. In: Thomaz JB, Belczack CEQ. Tratado de flebologia e lin-fologia. Rio de Janeiro: Livraria Rubio; 2006. P. 301-322.
23. Barros FS, Perez JMG, Zandonade E, Salles-Cunha SX, Monedero JL, Hilel ABS, et al. Evaluation of pelvic varicose veins using color Doppler ultrasound: comparison of results obtained with ultrasound of the lower limbs, transvaginal ultrasound, and phlebography. J Vasc Bras 2010; 9(2):15-20.
24. Black CM, Thorpe K, Nielsen R. Diagnosis and Endovascular Management of PVI. Pelvic venous insufficiency remains an underdiagnosed but treatable cause of chronic pelvic pain. Endovascular today. 2009. P. 67-71. Available from: https://evtoday.com/2009/07/EVT0709_08.php
25. Kim HS, Malhotra AD, Rowe PC, Lee JM, Venbrux AC. Embolotherapy for pelvic congestion syndrome: long-term results. J Vasc Intervent Radiol 2006;17(2, Pt 1):289-297. DOI:10.1097/01.RVI.00001948 70.11980.F8
26. Park SJ, Lim JW, Ko YT, Lee DH, Yoon Y, Oh JH, et al. Diagnosis of pelvic congestion syndrome using transabdominal and transvaginal sonography. AJR Am J Roentgenol 2004;182(3):683-688. DOI:10.2214/ajr.182.3.1820683
27. Beard RW, Highman JH, Pearce S, Reginald PW. Diagnosis of pelvic varicosities in women with chronic pelvic pain. Lancet 1984; 2(8409):946-949.
28. Kennedy A, Hemingway A. Radiology of ovarian varices. Br J Hosp Med 1990;44(1):38-43.
29. Coakley FV, Varghese SL, Hricak H. CT and MRI of pelvic varices in women. J Comput Assist Tomogr 1999; 23(3):429-434.
30. Tsukanov A.Yu., Lyashev R.V. Violation of venous blood flow as a cause of chronic abacterial prostatitis (chronic pelvic pain syndrome). Urology 2014; (4):37-42.
Topics and tags
BPH
Nocturia
Magazine
Journal "Experimental and Clinical Urology" Issue No. 1, 2017
Comments
To post comments you must log in or register
Diagnostics
To effectively treat the disease, you need to use all diagnostic methods. To detect varicocele, experienced specialists only need to visually examine the patient and palpate the plexus of testicular venous vessels in the form of a cluster. The man is examined in a standing position, in a calm state. To clarify the results of palpation, the patient is asked to tense the abdominal muscles (Valsalva maneuver) to improve the filling of testicular vessels with blood. In this case, the study of the enlarged area will be more complete. This will help in diagnosing grade 2-3 varicocele; if the problem is not expressed, you will need the help of modern equipment. Ultrasound and doplegraphic examination of the scrotum is necessary to clarify the diagnosis. The patient must be examined in two positions - standing and sitting. To rule out infertility, a man needs to have a spermogram. One semen examination is not enough; examination in the interval from 4 to 12 weeks will make the diagnosis more accurate. This diagnosis is very informative; it can be used to determine the type of varicocele, obtain data on the size of the testicle, the location of diseased veins, and thickening of the spermatic cord.
Classification
The degrees of the disease are classified based on the dilation of the veins of the spermatic cord and testicle. The development of varicocele is divided into 4 degrees. They speak of zero degree if the symptoms of the disease cannot be determined visually or by manual palpation. Only instrumental examination (most often when diagnosing other problems) reveals varicocele. Grade 1 is diagnosed when the dilation of the veins cannot be palpated with the patient lying down, only standing. In patients with the 2nd degree of the disease, the doctor feels with his hands an increase in the venous vessels of the spermatic cord and testicle in men who are sitting and standing. To determine the third degree of varicocele, a visual examination of the patient is sufficient. If we consider testicular varicose veins from the point of view of the location of the pathology, then we distinguish left-, right- and bilateral varicoceles. Subclinical and clinical types of the disease are classified depending on physical examination methods.
Physiology
Why do guys have visible veins on their arms? The latter may appear due to the physiological characteristics of the body. Most often, such manifestations are characteristic of “wiry” men. With age, the skin loses its elasticity. In the absence of an abundance of fat deposits, veins may also protrude in older men. If there is no pain or other discomfort, there is no reason to worry.
Veins in a guy’s arms can appear due to hereditary structural features of the body. Often protruding blood veins are observed in those with thin skin and thin people. They are especially noticeable on the dorsum of the hand.
The veins on a guy’s arms stand out clearly under the skin when the atmospheric pressure increases, as well as in hot weather. As a result of an increase in ambient temperature, blood begins to circulate faster and blood vessels dilate. On the contrary, in cold weather, previously prominent veins are practically invisible.
Treatment
The problem of varicose veins in the vessels of the spermatic cord and testicle cannot be eliminated. Improper operation of the blood outflow valves can be corrected through surgery. Surgical treatment of varicocele is the main method. The effectiveness of medication use is insignificant. Only the first stages of the disease can be treated conservatively. Consultation with a doctor and a joint decision on surgery for varicocele are mandatory. Surgical intervention is not always necessary for the patient. If the disease does not bother the man too much, or the patient is of advanced age, then doctors advise not to undergo surgery. A variety of surgical methods helps doctors find the only correct method. The essence of the operation for varicocele is to ligate the venous pathological vessels and normalize the outflow of blood. To save the results obtained during the operation, you should:
- limit physical and sexual stress;
- come to your doctor for examination.
Preventing the formation of protruding veins on the arms
If a man or woman wants to visually eliminate veins that stand out under the skin, the situation can be corrected by applying the following preventive solutions:
- To begin with, it is worth reducing the level of physical activity on the upper extremities by eliminating exercise equipment and lifting all kinds of weights from your daily routine.
- The veins on a guy's arms can become less noticeable if he regularly warms up his body. The volume of veins will decrease over time as a result of improved blood circulation processes. In particular, holding the arms in a raised position helps to increase the venous outflow of blood.
- To make protruding veins less noticeable, it is enough to work on changing your daily diet, enriching it with fresh fruits and vegetables. Products in this category contain a whole host of useful enzymes that thin the blood, normalize blood pressure, and increase vascular tone.
- Water treatments can make prominent veins almost invisible. By regularly taking a contrast shower, you can see positive changes in a short time. Exposure of the body to water of different temperatures activates the work of the heart muscle and also has a relaxing effect on body tissues.