The structure of the heart contains tendon threads called chords. Normally, they are attached to the valve flaps through which blood flows, and prevent them from sagging under the influence of gravity. However, sometimes an additional chord may be detected during diagnosis. This is a structural feature of the heart, which does not always indicate an anomaly. But in some cases it can be dangerous to the health and even life of the patient.
What is a chord
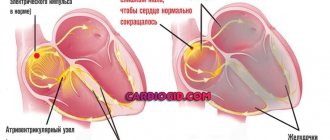
The human heart consists of 4 chambers through which blood regularly passes - 2 ventricles and 2 atria. Blood flow moves through valves, which open in chords. When tensioned, the valve opens the flaps, and when loosened, it closes. Thanks to this, the blood flows only in a given direction and does not move backward.
The valves tension special longitudinal strands - chords. But along with the main ones, additional chords are often identified. They are also attached to certain parts of the heart, but do not take any part in pumping blood. Therefore they are also called false chords.
Patent foramen ovale
This is the opening located between the two upper chambers of the heart (the left and right atria). It functions as a “door” during the development of the child in the womb. Through it, blood is discharged from the fetus from right to left. This is how blood flow exchanges between the small and large circles of blood circulation. An open foramen ovale in a child before birth plays a big role, “helping” the undeveloped lungs cope with blood flow. It is this that ensures the passage of blood to the left atrium and aorta.
When a child is born and his lungs, expanding, begin to work at full strength, the oval window “automatically” closes. A small depression remains in its place. However, there are cases when the oval window does not close after the baby is born. It is important to keep in mind that this anomaly does not belong to heart defects, and it can be detected by echocardiography. Usually, the bubble contrast technique is used for this, and if the baby’s oval window is not closed, air bubbles will move from right to left during examination.
Why do false chords of the heart appear?
False chords are quite easy to detect already in a child’s heart. Moreover, pediatricians do this while listening to the chest (by the presence of heart murmurs). Typically, additional chordae form during fetal development. The main reasons for their appearance are:
- Heredity - for example, parents or grandparents also had this diagnosis.
- The mother’s unhealthy lifestyle, especially during pregnancy (smoking, drinking alcohol, uncontrolled use of medications, toxic substances), and the presence of chronic or infectious diseases.
- Genetic factor - mutation of genes or chromosomes.
- Unbalanced diet - excess animal fat.
- Heavy workload during pregnancy.
- Unfavorable environmental conditions.
- Constant, severe stress.
- Deterioration of immunity for various reasons.
Combating complications
Despite the fact that trabeculae in the cavity of the left ventricle do not pose a threat to the child’s health, with the wrong lifestyle they can go from a benign form (painless) to a malignant one (requiring regular use of medications). Therefore, when a disease is detected, doctors immediately determine prohibitions for the patient. These include:
- Extreme sports, sports career, active gymnastics, excessively active dancing, scuba diving.
- Unauthorized taking of medications. Each drug (even those not related to heart disease), its dosage, must be approved by a specialist. Many pharmacological drugs affect intravascular pressure and increase heart rate, which is unacceptable for this type of pathology.
- Intense physical and emotional stress.
In addition, the doctor issues a certificate prohibiting the child from participating in school physical education competitions and exempting him from certain types of exercises. He develops such a complex of activities so that the child’s additional trabecula of the left ventricle is trained and does not bother him in the future. This shows:
- Easy short run.
- Walking on a tightrope.
- Drill exercises.
- Jumping.
- Gymnastic procedures on a skipping rope, wall bars, bench, with a ball.
In addition to all this, a child with an additional chord will benefit from attending massage courses, eating right, going to slow dances, resting more often and not getting into stressful situations.
The best way to give birth to a healthy baby is to avoid factors that can negatively affect the development of the fetus (for the entire period of pregnancy). If the expectant mother has this disease, it is recommended to take it much more seriously. This way you can reduce the risk of an additional chord. If a child has already been born with such a pathology, you need to carefully monitor the baby’s well-being and listen to every medical recommendation so that the child grows and develops on par with his peers.
Accessory chord: symptoms
A person can comfortably live their entire life with additional chordae, unaware of their existence. Most often they do not cause any sensation. But sometimes patients may notice the following symptoms:
- fast fatiguability;
- periodic manifestation of fatigue;
- pain in the heart area;
- headache;
- rapid heartbeat (the heart “jumps out”), especially during excitement or conflict.
The described symptoms do not necessarily indicate the presence of a chord, since they may be associated with other causes. Therefore, to accurately determine the cause, it is necessary to undergo professional diagnostics.
Diagnostics
First of all, you need to contact a therapist or children's doctor (pediatrician), who will listen to your heart rhythm using a stethoscope. It is very easy to hear a heart murmur, so the therapist can easily make a preliminary diagnosis after the first examination.
Next, the patient may be referred for additional diagnostics:
- ECG at rest and after exercise;
- blood pressure measurement;
- Holter monitoring.
Thanks to the examinations carried out, it is possible to accurately determine the presence of a chord, the degree of its danger to health, as well as other diseases (if any).
Clinical significance of minor cardiac anomalies in children
In recent years, much attention has been paid to connective tissue dysplasia (CTD) in children. DTD is understood as a congenital anomaly of the connective tissue structure of various organs and systems, which is based on a decrease in the content of certain types of collagen and/or a violation of their ratio, leading to a decrease in the strength of connective tissue [12, 13, 24, 26].
Endogenous (chromosomal and genetic defects) and exogenous (unfavorable environmental conditions, inadequate nutrition, stress) factors take part in the development of DST [12, 30, 43]. The peculiarity of connective tissue morphogenesis is that it participates in the formation of the heart frame at almost all stages of ontogenesis; therefore, the influence of any damaging factor can lead to the development of cardiac dystrophy [15].
In 1990, in the classification of diseases of the cardiovascular system of the New York Association of Cardiologists, as well as in Omsk, at a symposium dedicated to the problem of connective tissue dysplasia, the syndrome of cardiac dysplasia, accompanying both differentiated and undifferentiated dysplasia, was first identified. In case of DST syndrome of the heart, its connective tissue framework is involved in the pathological process - heart valves (atrioventricular, semilunar, Eustachian valve), subvalvular apparatus, heart septa and great vessels.
In clinical practice, when it comes to the morphological basis of changes in the cardiovascular system without hemodynamic disturbances, Yu. M. Belozerov (1993) and S. F. Gnusaev (1995) instead of the term “DST of the heart” proposed another one - “minor developmental anomalies heart" (MARS) [3, 8]. According to the definition of these authors, MARS are considered anatomical changes in the architecture of the heart and great vessels that do not lead to gross impairment of the functions of the cardiovascular system [9].
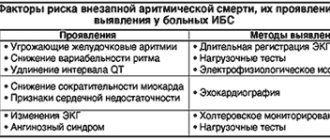
Classification of MARS according to S. F. Gnusaev, 2001 (as amended)
- Localization and form:
atria and interatrial septum: prolapsed valve of the inferior vena cava, enlarged Eustachian valve more than 1 cm, patent foramen ovale, small aneurysm of the interatrial septum, prolapsed pectineus muscles in the right atrium;tricuspid valve: displacement of the septal leaflet into the cavity of the right ventricle within 10 mm, dilatation of the right atrioventricular orifice, prolapse of the tricuspid valve;
pulmonary artery: dilatation of the pulmonary artery trunk, prolapse of the leaflets;
aorta: borderline narrow and wide aortic root, dilatation of the sinus of Valsalva, bicuspid aortic valve, asymmetry and prolapse of the aortic valve leaflets;
left ventricle: trabeculae (transverse, longitudinal, diagonal), small aneurysm of the interventricular septum;
mitral valve: mitral valve prolapse, ectopic attachment of chords, impaired distribution of chords of the anterior and (or) posterior leaflet, “fluttering” chords, additional and abnormally located papillary muscles.
- Complications and associated changes: infectious carditis, calcification, myxomatosis, fibrosis of valve leaflets, chordae ruptures, cardiac arrhythmias.
- Characteristics of hemodynamics: regurgitation, its degree, presence of circulatory failure, pulmonary hypertension.
There is still no consensus on the clinical significance of MARS, many of which are unstable due to the growth of the child. Thus, it is possible to reverse the development of an enlarged Eustachian valve, prolapsed pectineus muscles in the right atrium, mitral valve prolapse (MVP), closure of the open oval window, normalization of the length of the mitral valve chords and the diameter of the great vessels. In some cases, MARS change not only qualitatively, but also quantitatively [3]. Exceeding the established threshold level of cardiac stigmatization in healthy children (more than 3 MARS), according to S. F. Gnusaev (1995), indicates possible disadvantage both in relation to factors influencing the formation of health and indicators characterizing it [8].
Considering that MARS are a variant of visceral DST, children, as a rule, have a pronounced polymorphism of clinical and morphological disorders, depending on the degree of DST and the involvement of other organs and systems in the pathological process. An associative relationship has been identified between the number of external phenotypic markers of CTD and MARS [12, 16, 21, 22]. In this case, not only the number of external phenotypic markers matters, but also the “diagnostic weight” of each of them. It has been noted that skin and skeletal dysplasias are most often combined with MARS [12].
The clinical significance of connective tissue pathology in people with CTD is confirmed by data on the high frequency of neurovegetative disorders, changes in the central nervous system (enuresis, speech defects, vegetative-vascular dystonia (VSD)), and mental disorders [5, 12, 24]. As a rule, VSD is always detected in such patients, which is probably due to hereditary (hereditary) features of the structure and function of the limbic-reticular complex, which determine the abnormal nature of neurovegetative reactions [12]. E. V. Bulankina (2002) established a clear relationship between autonomic dysfunction and DST [4]. At the same time, the severity of dysplastic changes was combined with the severity of the processes of maladaptation of regulatory mechanisms and a decrease in the stress resistance of the body. The most common manifestations of autonomic dysfunction are cephalgia, autonomic crises, vegetative visceral paroxysms, pre- and syncope [12, 16]. According to the data of S.F. Gnusaev (1995), insufficiency of segmental autonomic structures was revealed in persons with MVP [8]. Research by T. M. Domnitskaya (2000) made it possible to establish a direct relationship between MVP, abnormally located trabeculae (ART) and the prevalence of neurotic (neurotic reactions, obsessive-compulsive neurosis, panic disorders) and encephalopathic (cerebrasthenic syndrome, stuttering, tics, sleep disorders, enuresis , hyperdynamic syndrome, fears) disorders [10].
MARS is often accompanied by pathological conditions such as cardiac rhythm and conduction disorders, including early repolarization syndrome, sick sinus syndrome, Wolff–Parkinson–White syndrome, increased electrical activity of the left ventricle, right bundle branch block, extrasystole and paroxysmal tachycardia [ 4, 6, 8, 34]. According to L.A. Balykova et al. (2002), in 90% of patients with cardiac arrhythmias, MARS (mainly MVP) were identified using echography [2]. However, not all MARS are accompanied by heart rhythm disturbances and/or may be their cause. Arrhythmogenic MARS include fibromuscular abnormal chordae (APC) and ART, MVP and tricuspid valve prolapse (TVP), atrial septal aneurysm, enlarged and/or prolapsed Eustachian valve.
The presence of conducting cardiomyocytes in the fibromuscular ARH and ART forms additional conducting pathways, which explains the origin of the impulse that advances intraventricular conduction and causes early excitation of adjacent segments with subsequent earlier repolarization [12, 15, 19, 20, 28]. There is histological confirmation of the presence of conducting cells in the ART with diagonal-basal, mid-transverse and longitudinal localization and in the ART connecting the basal septal sections and the lateral wall of the left ventricle [3, 10, 33]. M. Suwa et al. (1986) noted an increase in the frequency of ventricular extrasystoles with increasing chord thickness. According to E. Chesler et al. (1983), the appearance of ventricular extrasystoles is associated with myxomatous changes in the chordae, causing mechanical irritation of the wall of the left ventricle [27]. The fact that ARX and ART are arrhythmogenic is also confirmed by the disappearance of extrasystoles in patients in the event of their independent rupture or surgical dissection, or during physical activity, when the degree of their tension decreases [8, 10, 12]. A fairly common cardiac arrhythmia in patients with ARH and ART is early ventricular excitation syndrome [6, 12].
Arrhythmias during MVP and PTC, according to various authors, occur in 15 to 90% of cases [11]. Among the causes of arrhythmias, autonomic dysfunction, mechanical stimulation of the endocardium, interstitial magnesium deficiency, psychological stress and myxomatous degeneration of valve leaflets are considered [3, 10–12, 18, 27, 29, 37, 39]. A direct correlation has been established between the frequency and severity of rhythm disturbances and the depth of MVP [1]. A number of authors believe that the cause of the development of arrhythmias in MVP and PTC may be turbulent flow resulting from regurgitation through the valve ring during ventricular systole, especially in PTC, when mechanical irritation of the sinus node area occurs [3, 8, 23]. Most researchers consider excessive tension of the papillary muscles due to their abnormal traction during prolapse of the leaflets as a possible mechanism for the development of ventricular extrasystoles in MVP [12, 14, 25, 38].
The development of arrhythmias can be provoked by a prolapsed Eustachian valve and an aneurysm of the interatrial septum: the conditions for the occurrence of arrhythmias arise as a result of their hilly movements and their reflex irritation of pacemaker formations in the right atrium [42].
According to studies by O. A. Dianov (1999), heart rhythm disturbances occurred in children with a borderline narrow aorta, in whom supraventricular and ventricular extrasystoles were recorded in 32.4% of cases and ventricular extrasystoles in 10.8%, indicating decompensation of adaptation, especially in conditions physical activity [4].
According to Yu. M. Belozerov, children with MARS are characterized by reduced cardiohemodynamic capabilities and demonstrate poor tolerance to physical activity [3]. According to N.A. Mazur, a connection has been established between MVP and sudden death syndrome in adults. Enough information has been accumulated that children with MARS are at risk for developing infective endocarditis.
Thus, existing research results indicate that MARS in some cases are the basis of cardiovascular pathology in children. At the same time, it would be unjustified to exaggerate their role in functional disorders of the cardiovascular system. Obviously, in each specific case the significance of structural abnormalities of the heart must be considered individually.
The principles of therapy for children with MARS have not yet been fully formulated. However, today we can propose the following tactics for the management of children with MARS:
- Comprehensive health assessment, including various types of examination of children.
- The choice of therapy depends on clinical, electrophysiological and echocardiographic changes.
- The use of drugs aimed at normalizing connective tissue metabolism.
- Determination of adequate physical activity depending on the functional state of the myocardium.
The use of non-drug treatment methods is generally accepted, including: - age-appropriate organization of work and rest;
- maintaining a daily routine;
- rational, balanced nutrition;
- psychotherapy and auto-training;
- water and balneotherapy;
- massage (manual, underwater, etc.);
- physiotherapy (electrophoresis with MgSO4, electrosleep, etc.);
- physical education classes, exercise therapy.
The issue of admission to sports is decided individually. In the presence of MVP, it is necessary to take into account family history (cases of sudden death in relatives), the presence of complaints of palpitations, cardialgia; syncope; changes on the ECG (heart rhythm disturbances, short and long QT syndrome) are the basis for deciding whether sports training is contraindicated. This also applies to the presence of ARCH, ART with early ventricular excitation syndrome, which, being arrhythmogenic MARS, can provoke cardiac arrhythmias in athletes under conditions of physical and psycho-emotional stress.
Drug treatment includes the use of:
- magnesium preparations;
- cardiotrophic therapy (in case of disruption of repolarization processes in the myocardium);
- antibacterial therapy for exacerbation of foci of infection, surgical interventions (prevention of infective endocarditis);
- antiarrhythmic drugs (according to indications, with pure group extrasystole with impaired repolarization processes).
Currently, therapy with magnesium preparations for MARS is approaching pathogenetic. This is due to the fact that magnesium is part of the main substance of connective tissue and is necessary for the proper formation of collagen fibers. Under conditions of magnesium deficiency, the ability of fibroblasts to produce collagen is impaired [29, 31]. In addition, magnesium has a membrane-stabilizing effect, retains potassium inside the cell, and prevents sympathicotonic effects, which makes it possible to use it for the treatment of cardiac arrhythmias [40, 41].
In the works of O. B. Stepura (1999), O. D. Ostroumova et al. (2004) there is information about a significant decrease in the degree of MVP, symptoms of VSD, and the number of ventricular extrasystoles during therapy with magnesium drugs [17, 18].
The following medications may be considered appropriate:
Magnerot containing magnesium salt and orotic acid. The latter not only enhances the reabsorption of Mg in the intestine, but also has an independent metabolic effect. Children are prescribed 500 mg of Magnerot (32.8 mg of magnesium 3 times a day for 1 week, then 250 mg 3 times a day for the next 5 weeks. The drug is taken 1 hour before meals).
Magne B6. Available in tablets (48 mg magnesium or in oral solution (100 mg magnesium). Children weighing more than 10 kg (over 1 year) - 5-10 mg/kg/day in 2-3 doses. Children over 12 years old — 3–4 tablets per day, in 2–3 doses, course duration 6–8 weeks.
Potassium orotate. For children, the drug is prescribed at a rate of 10–20 mg/kg/day in 2–3 doses, 1 hour before meals or 4 hours after meals. Course duration - 1 month.
Repeated courses of therapy with these drugs should be carried out (3-4 times a year).
To improve the cellular energy of the myocardium, drugs are used that have a complex effect on metabolic processes in the body, and are also active antioxidants and membrane stabilizers:
- L-carnitine (elkar - 20% solution of carnitine hydrochloride). Doses: 1–6 years, 0.1 g/day (14 drops) 3 times a day; 6–12 years – 0.2–0.3 g/day (1/4 tsp) 3 times a day. Course - 1–1.5 months.
- Coenzyme Q10 (ubiquinone) is prescribed to children over 12 years of age, 1 capsule (500 mg) 1–2 times a day. Preparations containing ubiquinone include kudesan: 1 drop per year of life (up to 12 years), then 12 drops 1 time per day. The duration of the course must be at least 1 month.
- Cytochrome C (cyto-mac). Available in ampoules (4 ml = 15 mg). Prescribed intramuscularly, 4 ml, No. 10. 2–4 courses are given per year.
In addition to these drugs, to improve metabolic processes in connective tissue, myocardium and the body as a whole, the use of:
- nicotinamide (vitamin PP) - 20 mg/day for 1.5–2 months;
- riboflavin (vitamin B2) - 10–15 mg/day for 1.5–2 months;
- thiamine (vitamin B1) - 10 mg/day and lipoic acid 100–500 mg/day for 1.5 months;
- limontara (complex of citric and succinic acid) 5 mg/kg/day 3–4 days weekly for 2 months;
- biotin - 2-5 mg/day - 1.5-2 months.
Repeated courses of treatment are indicated (up to 3 times a year).
In the presence of VSD, complex long-term therapy is carried out to restore the balance between the sympathetic and parasympathetic parts of the autonomic nervous system (differentiated herbal medicine, vegetotropic drugs, nootropics, vasoactive drugs - Cavinton, Vasobral, Instenon, cinnarizine, etc.).
Thus, all of the above allows us to conclude that MARS, being a visceral manifestation of connective tissue dysplasia, constitute the morphological basis of functional changes in cardiac activity and neurovegetative disorders. Choosing an individual course of treatment program helps improve metabolic processes in connective tissue and prevents possible complications of CTD in children and adolescents.
For questions regarding literature, please contact the editor.
N. A. Korovina , Doctor of Medical Sciences, Professor A. A. Tarasova, Candidate of Medical Sciences, Associate Professor T. M. Tvorogova, Candidate of Medical Sciences, Associate Professor L. P. Gavryushova, Candidate of Medical Sciences, Associate Professor M. S. Dzis RMAPO , Moscow
Treatment of the disease
If the false chord is not life-threatening and does not affect health, preventive monitoring by a cardiologist is indicated. Moreover, treatment as such is usually not prescribed - the patient regularly visits a specialist every 3-6 months.
If the situation is dangerous and the chord threatens the functioning of the heart (can lead to cardiac arrest), surgical intervention is indicated to remove it. Such a decision is made if the functioning of the heart is severely impaired, causing regular disruptions in the distribution of blood flow.
It is also allowed to use folk remedies (in consultation with the doctor):
- Take a handful of raisins every day in the morning (on an empty stomach);
- take valerian decoctions;
- drink tea based on peppermint or calendula flowers.