Published: 07/07/2021 11:15:00 Updated: 07/07/2021
Thrombosis is a complete or partial blockage of the lumen of a vessel by a parietal or mobile thrombus. A thrombus is a dense blood clot that appears as a result of a change in its fluidity. Normally, thrombus formation is a protective mechanism. Damage to the vascular wall leads to a slowdown in blood flow and accumulation of platelets around the damage. The thrombus literally “darns” the wall of the vessel.
The classic causes of thrombosis are described by Vikhrov’s triad: damage to the vascular wall, slowing of blood flow and changes in blood properties [3]. Some blood clots (they are called emboli) are able to move to narrower areas of the vessel, which are completely or partially blocked. Every year, about 25 million people die from thrombosis, and even more face trophic disorders caused by blood clots [3].
How do blood vessels bleed?
Bleeding can be mild, moderate or severe. His character may be:
- arterial - strong, jet;
- venous - blood loss occurs gradually;
- capillary - minor discharge due to damage to small vessels.
The problem itself can be stable/unstable, recurrent. Vessels of the mucosa, submucosal and intermuscular plexus, as well as those located outside the gastrointestinal tract, can bleed.
The expiration can last for several hours or days. In medicine there are:
- profuse blood loss - the patient loses more than 1 liter of blood in 1-3 hours and needs urgent medical attention;
- acute - less than 1 liter expires in 1-2 days, the patient’s vital signs are relatively stable;
- chronic - develops slowly, often over several weeks or even months, the intensity of symptoms gradually increases.
Course of the disease
The disease progresses very quickly. The heart attack stage occurs within 6-12 hours and can last a day. Patients at this time feel relief, but there is nothing good about this - the patient stops feeling pain, since pain receptors die as a result of the death of the intestine. After another 12 hours, new symptoms appear: high leukocytosis, increased heart rate, dry tongue and increased pain. The prognosis at this stage for the patient is extremely unfavorable and in almost all cases ends in death.
Why is there a problem?
Medicine knows about 200 causes of bleeding in the digestive tract. At the first symptoms, you should seek professional help from a doctor and under no circumstances self-medicate, as this will only worsen the condition.
Ulcer
The most common reason. With an ulcer, the integrity of the mucous membrane of the organ is disrupted, and the main difference of the disease is deep tissue damage. The disease is chronic - with remission and exacerbations. On the mucous membrane of the stomach, esophagus or duodenum, areas of inflammation are formed, in which the protective function (mucus secretion) is reduced. Gradually, the mucosal tissues, including the walls of blood vessels, become thinner, which leads to their rupture.
Phlebeurysm
The problem may occur in the esophagus or stomach due to increased pressure in the portal vein. The most common cause is cirrhosis of the liver. Rupture of a large vessel with varicose veins is extremely dangerous, since at this moment there is a copious outflow of blood. According to statistics, in 40% of cases it stops spontaneously. And the activity of bleeding depends on the degree of liver damage.
Colon diverticulosis
With this disease, the lining of the colon bulges, forming diverticula. The reasons for their formation in medicine are not completely clear; they are mainly associated with increased intraluminal pressure. Basically, the pathology is typical for adult patients over 50 years of age. In the acute course of the disease and rupture of intrawall blood vessels in the area of diverticula, intestinal bleeding occurs.
Tumors and polyps
They occur in the small and large intestines and are benign neoplasms that grow into the intestinal lumen. Most often, bleeding is minor and chronic. The danger lies in possible degeneration into malignant tumors.
Haemorrhoids
This is the formation of venous nodes around the rectum in the anal area. The main causes are thrombosis or tissue inflammation. The disease can be acute or chronic, and its common causes are a sedentary lifestyle, excessive exercise, and obesity. Bleeding (the color may be scarlet or dark) is minor and occurs most often after bowel movements.
More rarely, esophagitis, acute hemorrhagic gastropathy, erosive duodenitis, and Mallory-Weiss syndrome are found as causes of bleeding in the upper gastrointestinal tract. In the lower part, bleeding can be caused by tumors, vascular malformations, and various inflammations.
Treatment and prevention of thrombosis
Treatment of thrombosis includes anticoagulant and antiplatelet therapy, thrombolytic therapy, installation of an inferior vena cava cava filter, and surgical removal of the thrombus [5].
Complications of anticoagulant therapy must be kept in mind: major bleeding, heparin-induced thrombocytopenia and warfarin-induced skin necrosis [5]. To reduce the risk of continued thrombus formation, NSAIDs are used [2]. For the purpose of secondary prevention, small doses of heparin are prescribed. Non-drug treatment methods are also prescribed - elastic bandaging, compression hosiery, local hypothermia and exercise therapy [2, 4].
Prevention of thrombosis includes a number of measures used in situations of increased risk of thrombosis.
Primary prevention of atherothrombosis:
- systematic physical activity in the form of walking or morning exercises;
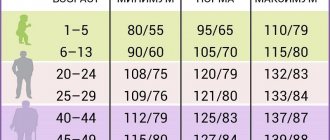
- blood pressure control, maintaining working blood pressure below 140/90 mmHg;
- control of blood sugar levels (less than 6 Mmol/l), early detection and treatment of diabetes mellitus;
- weight loss, body mass index less than 25 kg per m2;
- a diet limited in cholesterol and high-density fat (total cholesterol less than 5 mmol/l), fruits and vegetables;
- smoking cessation [3,7].
Primary prevention of venous thrombosis:
- compression underwear;
- bandaging with elastic bandages;
- drinking plenty of fluids, especially after surgery;
- regular exercise, walking, especially when traveling;
- prohibition of taking alcohol and sleeping pills in large doses;
- prohibition of the use of compressive shoes and clothing [2,5,6].
Sometimes, during periods of particular risk, anticoagulants are prescribed several days before the flight. There is no point in taking aspirin in such cases [5].
Who is at risk?
Basically, diseases that lead to bleeding are observed in adults. Moreover, according to statistics, men are 2 times more likely than women to be diagnosed with problems with the gastrointestinal tract - the stomach, duodenum. As we noted above, ulcerative pathologies hold first place in terms of the number of diseases. The peak age for diseases is 40-45 years.
However, the problem is not limited to adults. The diagnosis associated with ulcerative lesions of the gastrointestinal tract is often made to adolescents who uncontrollably consume junk food and drinks. Cases of the formation of intestinal polyps are also common.
Gastric and intestinal bleeding is increasingly being detected even in newborns. Basically, they are caused by intestinal volvulus. In 3-year-old children, leakage can be caused by the formation of a diaphragmatic hernia, as well as abnormalities in the development of the organs of the lower gastrointestinal tract.
Forecast
If timely treatment is not carried out, intestinal necrosis leads to death in 100% of cases. But even after the operation, the patient may die; complications such as infections, sepsis, and intestinal obstruction are possible. Many patients die from complications associated with the underlying and concomitant diseases. After surgical removal of the necrotic part of the intestine, the danger does not completely disappear, and the equally difficult task of further management of the patient falls on the shoulders of doctors. High risk of disability.
The International Clinic Medica24 employs highly qualified surgeons, resuscitators and other specialists. They provide assistance to patients as quickly as possible, in accordance with modern international standards. Our clinic has operating rooms and intensive care wards equipped with the most modern equipment. Thanks to all this, we can help patients with various severe, dangerous pathologies and ensure the best prognosis.
The material was prepared by oncologist, endoscopist of the International Clinic Medica24, Konstantin Yuryevich Ryabov.
What symptoms to look out for
Patients with the diagnoses we listed above should be especially monitored for the appearance of alarming symptoms. If you are taking medications for the liver and gastrointestinal tract, carefully monitor your well-being. If you are concerned about the changes discussed below, consult your doctor. However, knowing these signs is useful for every person, since many diseases of the lower and upper gastrointestinal tract develop without obvious painful sensations. Often their first manifestation may be the symptoms of bleeding.
Weakness
This is the main sign of any prolonged bleeding. Weakness gradually increases, the patient's skin turns pale, he feels cold sweat, a ringing in the ears, and trembling of the limbs. The weakened state may last for several minutes, after which it passes and returns periodically. If blood is bleeding actively, fainting or semi-fainting and even shock are possible.
Vomit
This symptom accompanies severe blood loss - more than 0.5 liters. If the vomit is dark cherry in color, it is most likely coming from a vein near the esophagus. If unchanged blood is clearly visible in the vomit, the integrity of the artery in the esophagus is most likely compromised. If the patient vomits so-called “coffee grounds” of brown color, the problem lies in the gastric vessels. Only a doctor can accurately determine the nature, location and intensity of blood loss.
Chair
Traces of blood in the stool may appear within a few hours or 1-2 days after the integrity of the blood vessels is damaged. With significant problems with the stomach or duodenum, as well as blood loss in a volume of more than 0.5 liters, you can observe melena - loose stools that resemble tar in color and consistency. If the blood loss is smaller, which often happens, for example, with intestinal bleeding, then the stool remains formed, but its color darkens.
Please note that darkening of the stool can occur due to eating foods that contain dark coloring substances, for example, blueberries and cherries. Dark stools are not an absolute sign of the presence of blood in the stool and problems in the upper or lower gastrointestinal tract. The diagnosis can only be made by a qualified specialist.
Pathogenesis
The pathogenesis of thrombosis has been studied and is well described by Virchow's triad. The main links in thrombus formation are: damage to the vascular endothelium, changes in blood flow and hypercoagulation (violation of the rheological properties of blood), the development of each of which has its own reasons.
The formation of intravital blood clotting in a vessel occurs in several stages and includes platelet agglutination, fibrinogen coagulation, erythrocyte agglutination and precipitation of plasma proteins.
How to make a diagnosis
The doctor examines the patient, assessing his external condition, the shade of the skin and mucous membranes. Then he measures blood pressure - often it is low.
In the clinic, the patient undergoes a general blood test. Using it you can quickly get an idea of the level of hemoglobin and the volume of other blood cells. Additionally, the diagnosis is made by biochemical analysis, but it is usually prescribed several days after the onset of blood loss, since the chemical composition of the blood changes only over time.
The main diagnosis concerns the detection of the very cause of the violation of the integrity of blood vessels. To do this, doctors use the following hardware examinations.
- Endoscopy - examination of the esophagus, stomach, duodenum using a flexible tube with a miniature camera allows you to quickly detect a problem area;
- Contrast radiography - an effective method for detecting bleeding in the gastrointestinal tract involves injecting a safe contrast solution into the organ, followed by an X-ray;
- Magnetic resonance imaging is a modern method that allows you to obtain comprehensive information about the condition of all tissues of a particular organ of the gastrointestinal tract.
Causes
The immediate causes of a blood clot in the vascular bed of the mesentery are changes in the vascular walls against the background of slow blood flow and increased blood clotting. Indirect causes of the development of a blood clot in the arterial bloodstream of the intestine are: chronic heart failure , hypercoagulable processes , cardiosclerosis , endocarditis , vascular atherosclerosis , pancreatitis , trauma .
The causes of intestinal thrombosis in the venous vessels of the intestine are mechanical (strangulation of the mesentery, adhesions, volvulus), closed abdominal trauma with damage to the mesenteric veins/intestinal contusion, blood diseases (thrombocytosis), hemodynamic disorders, increased intra-abdominal pressure, taking oral contraceptives, portal hypertension , malignant neoplasms, destructive forms of pancreatitis , appendicitis , cholecystitis cardiac decompensation , taking hormonal drugs, Crohn's disease , ulcerative colitis , intra-abdominal infections of the abdominal organs, abscesses .
List of sources
- Pokrovsky A.V., Yudin V.I. Acute mesenteric obstruction // Clinical angiology: Guide / Ed. A. V. Pokrovsky. T. 2. M.: Medicine, 2004. P. 626-645.
- Savelyev V. S., Spiridonov I. V., Boldin B. V. Acute disorders of mesenteric circulation. Intestinal infarction: Guide to emergency surgery / Ed. B. S. Savelyeva. M.: Triada-X, 2004. pp. 281-302.
- Solomentseva T. A. Acute disorders of mesenteric circulation in a therapeutic clinic // Acute and emergency conditions in medical practice. 2011. No. 2. P. 8-14.
- Yushkevich D.V., Khryshchanovich V.Ya., Ladutko I.M. Diagnosis and treatment of acute disturbance of mesenteric circulation: current state of the problem // Med. magazine 2013. No. 3. P. 38-44.
- Katerina J.M., Kahan S. Emergency Medicine: Trans. from English - M.: MEDpress-inform, 2005. - 336 p.