Why is this necessary?
If you have suffered deep vein thrombosis of the lower or upper extremities, your doctor will most likely prescribe you indirect anticoagulants.
The main drug in this group today, both here and abroad, is warfarin. In our country, another drug of this group is used quite widely - phenylin. Other coumarin drugs (acenocoumarol, marcumar, marivan) can be used. The recommendations given are mostly applicable to any anticoagulant. The purpose of this medication is to prevent blood clots from recurring, which could cause your condition to worsen or cause life-threatening complications. The risk of recurrence of thrombosis is quite high during the first year after the first episode of the disease, therefore, taking into account various factors, warfarin is prescribed for a period of 2 to 12 months. In rare cases, longer therapy is performed. Indirect anticoagulants have no effect on an already formed blood clot.
To determine the duration of treatment, special (including genetic) blood tests are sometimes required to identify an increased tendency to blood clots.
A very large number of patients around the world receive the treatment you have prescribed. It is used not only in phlebology, but also in such areas of medicine as vascular surgery. In addition to deep vein thrombosis, the basis for prescribing anticoagulant therapy is often previous heart attacks, cardiac arrhythmias, valve and peripheral vessel replacement, and much more.
Indications for use of Warfarin
The drug is used for the treatment and prevention of embolism and thrombosis of blood vessels. The following indications for the use of Warfarin are determined:
- venous thrombosis in acute form, as well as recurrent;
- pulmonary embolism;
- strokes , transient ischemic attacks ;
- prevention of thromboembolic complications in people who have had myocardial infarction ;
- secondary prevention of myocardial infarction ;
- prevention of thromboembolic complications in people with heart valve damage, atrial fibrillation, as well as in those who have undergone heart valve replacement;
- prevention of postoperative thrombosis .
How to monitor treatment
Carrying out antithrombotic (anticoagulant) therapy can save your life and health, but requires increased attention and mandatory compliance with the doctor’s recommendations. Warfarin is a drug that reduces the ability of blood to clot, so its excess can lead to hemorrhagic complications, i.e. to bleeding. To avoid complications, the required dose of warfarin is monitored using a blood test called INR (International Normalized Ratio). This may sometimes be referred to as INR in laboratory responses. During the entire period of taking warfarin, the INR should be in the range of 2.0 - 3.0. If the INR is less than 2.0, then blood clotting is not reduced and thrombotic complications are possible. If the INR is more than 4.0, hemorrhagic complications are very real. An increase in INR from 2.5 to 4.0 indicates the need to reduce the dose of the drug, but usually does not pose a direct threat. For some diseases, the required upper limit of INR is 4.0 - 4.4.
In the absence of the ability to determine INR, monitoring by prothrombin time (PT) is acceptable, but this method is much less reliable. No other blood tests are needed to calculate your warfarin dose. To identify the side effects of the drug, a general blood test, urine test and some biochemical tests are periodically prescribed.
Warfarin price, where to buy
Price Warfarin Nycomed – from 115 rubles. per pack 50 pcs. Packing of tablets 100 pcs. costs on average 180 rubles.
- Online pharmacies in RussiaRussia
- Online pharmacies in UkraineUkraine
- Online pharmacies in KazakhstanKazakhstan
ZdravCity
- Warfarin Nycomed tablets 2.5 mg 100 pcs. Takeda Pharma Sp.
z o.o. 167 RUR order - Warfarin-OBL tablets 2.5 mg 100 pcs. JSC Obolenskoe farm. company
127 RUR order
- Warfarin tablets 2.5 mg 100 pcs. OzonOzon LLC
118 RUR order
- Warfarin-OBL tab. 2.5 mg No. 50AO Obolenskoe farm. company
87 RUR order
- Warfarin Nycomed tablets 2.5 mg 50 pcs. Takeda Pharma Sp. z o.o.
109 rub. order
Pharmacy Dialogue
- Warfarin Nycomed (2.5 mg tablet No. 50)Nycomed
105 rub. order
- Warfarin (2.5 mg tablet No. 50) Ozon LLC
71 RUR order
- Warfarin (2.5 mg tablet No. 100)Canonpharma Production
106 rub. order
- Warfarin Nycomed (2.5 mg tablet No. 50)Takeda
99 RUR order
- Warfarin Nycomed (2.5 mg tablet No. 100)Takeda
RUB 151 order
show more
Pharmacy24
- Warfarin-FS 2.5 mg N100 tablets Pharma Start TOV, Ukraine
78 UAH order - Warfarin-FS 3 mg No. 100 tablets Pharma Start TOV, Ukraine
91 UAH order
- Warfarin 2.5 mg No. 100 tablets Takeda Pharma A/S, Denmark/Takeda Pharma Sp.z.o.o., Poland
105 UAH order
PaniPharmacy
- WARFARIN tablets Warfarin tablets. 3mg No. 30 Finland, Orion
80 UAH order
- WARFARIN tablets Warfarin tablets 5 mg No. 100 Finland, Orion
185 UAH order
- WARFARIN tablets Warfarin Nycomed tablets 2.5 mg No. 100 Denmark, Takeda Pharma
110 UAH order
- WARFARIN tablets Warfarin tablets 3 mg No. 100 Ukraine, Pharma Start LLC
98 UAH order
- WARFARIN tablets Warfarin tablets. 3mg No. 100 Finland, Orion
190 UAH order
show more
How to take the drug
Warfarin is available in 2.5 milligram tablets. Most often, the “starting” and “maintenance” doses of the drug are 5 milligrams (2 tablets) per day. In many cases, for more “fine” adjustments, you will change the dose of the medicine that you take not per day, but per week. This may require either dividing the tablet in half or taking different numbers of tablets on different days. To make it easier to monitor your treatment, you may be given a special account book, or you can keep a notebook with a treatment diary, where it is useful to note the doses of warfarin, INR level, and other laboratory data.
Warfarin is taken in the entire daily dose at one time, preferably at 17:00 - 19:00. Take the tablets with water. It is not recommended to take it with food, but can be taken on an empty stomach. Phenyline is usually taken in 2 doses.
Reviews about Warfarin
Users write different reviews about Warfarin Nycomed. Many patients have been taking this medication for many years and it is an effective blood thinner. As side effects, users note the periodic development of nausea , increased bleeding , and dizziness . At the same time, patients note that the key to the effectiveness of the medicine is strict adherence to the treatment regimen and monitoring of the body’s condition.
Warfarin dose selection
The most difficult and responsible stage. “Loading” initial doses of warfarin (more than 5 mg) are not recommended.
Dose selection can be carried out both with and without the use of low molecular weight heparins (Fraxiparine, Clexane), both in the hospital and on an outpatient basis. The selection period on average takes from 1 to 2 weeks, but in some cases it increases to 2 months. At this time, you will need frequent INR determinations, up to 2 - 3 times a week or daily. Each time, after receiving the next test result, your doctor will determine a change in the dose of the medication and the date of the next test.
If in several tests in a row the INR remains in the range of 2.0 - 2.5, this means that the dose of warfarin has been adjusted. Further monitoring of treatment will be much easier.
special instructions
During treatment, the patient must adhere to the prescribed dosage.
It should be taken into account that patients suffering from dementia or alcoholism may be unable to comply with the dosage of the drug.
The effect of the drug may be enhanced under certain conditions: fever, decompensated heart failure, hyperthyroidism , alcoholism with liver damage. In case of nephrotic syndrome or renal failure, the effect may be either decreased or increased. In case of liver failure, the effect is enhanced. In all of these conditions, it is important to monitor the INR.
People undergoing warfarin treatment are recommended to use Tramadol , paracetamol or opiates as painkillers.
People with a mutation in the gene that codes for the CYP2C9 enzyme have a longer half-life. Therefore, such patients need to be prescribed lower doses of the drug.
Warfarin is not prescribed to patients with lactase enzyme deficiency, galactose intolerance, impaired absorption of glucose and galactose. If it is necessary to obtain a rapid antithrombotic effect, it is recommended to begin therapy with the administration of heparin, then carry out combined treatment with heparin and Warfarin for 5-7 days until the MHO level remains stable for two days.
To avoid coumarin necrosis, people who have a hereditary deficiency of antithrombotic protein C or S should initially be given heparin. It must be administered within 5-7 days. The initial dose of Warfarin should not be higher than 5 mg.
If individual resistance to Warfarin occurs, the patient needs to be given 5-20 loading doses of the drug.
Monitoring the dose of warfarin
If the dose of the drug is selected, less frequent monitoring is sufficient - first once every 2 weeks, then once a month. The frequency of additional studies is determined separately. The need for an extraordinary determination of the INR may arise in a number of cases, which we will discuss below. If in any doubt, ask your doctor for advice.
Currently, there are portable devices for self-determination of INR (similar to systems for monitoring blood sugar levels in patients with diabetes), but their cost is very high and, in most cases of deep vein thrombosis, purchasing them is impractical.
What may affect treatment
- Any concomitant diseases (including “colds” or exacerbation of chronic diseases)
- The use of drugs that affect the blood coagulation system. This is especially true for a large class of drugs that includes aspirin. It also includes many drugs prescribed as anti-inflammatory and painkillers (diclofenac, ibuprofen, ketoprofen, etc.). As a mild analgesic during treatment with warfarin, it is better to use paracetamol in normal dosages. In any case, the need for a new medication and the duration of its use must be agreed with the attending physician. When warfarin and aspirin are prescribed simultaneously, the INR is maintained in the range of 2.0 - 2.5.
- The use of drugs that affect the absorption, excretion and metabolism of warfarin. Most often, it is necessary to take into account the prescription of broad-spectrum antibiotics and oral antidiabetic agents. However, taking any new medicine may change how warfarin works. If concomitant treatment is necessary, additional INR analysis is usually prescribed at the beginning and end of therapy.
- Diet changes.
Warfarin acts on blood clotting through vitamin K, which is found in varying amounts in food.
There is no need to avoid foods high in vitamin K! Nutrition should be complete. You just need to make sure that there is no significant change in their proportion in the diet, for example, depending on the season. If you significantly increase your intake of foods rich in vitamin K while on a stable dose of warfarin, this may greatly weaken its effect and lead to thromboembolic complications.
The maximum amount of vitamin K (3000 - 6000 mcg/kg) is found in dark green leafy vegetables and herbs (spinach, parsley, green cabbage), and in green tea up to 7000 mcg/kg; intermediate amounts (1000 - 2000 mcg/kg) - in plants with paler leaves (white cabbage, lettuce, broccoli, Brussels sprouts). A significant amount of the vitamin is found in legumes, mayonnaise (due to vegetable oils), and green tea. Fats and oils contain varying amounts of vitamin K (300 - 1000 mcg/kg), more of it in soybean, rapeseed, and olive oils. The content of vitamin K in dairy, meat, bakery products, mushrooms, vegetables and fruits, black tea, coffee is low (no more than 100 mcg/kg). Regular consumption of berries and cranberry juice may increase the effect of warfarin.
Small doses of alcohol with normal liver function do not affect anticoagulant therapy, but alcohol consumption must be treated with caution.
Taking multivitamins that contain vitamin K may reduce the effect of warfarin.
Indirect anticoagulants: warfarin
20s of the XX century. North America. An epidemic of an unknown disease among... cattle. Death of bulls from bleeding during castration and after removal of horns. Spontaneous bleeding during milking in cows. It's all due to moldy clover.
In 1921, local veterinarian Frank Scholfield noticed that all these animals were feeding on sweet clover (Melilotus) silage, which had become moldy in the damp conditions. Scholfield conducted a series of experiments on rabbits and confirmed his hypothesis: the rabbits actually died from bleeding after feeding with moldy sweet clover.
A group of rabbits that ate uninfected hay were alive, active and healthy. Farmers' financial situation did not allow them to replace feed, and the situation remained deplorable and bleeding. American veterinarian L. M. Roderick in 1929 established exactly how blood stops clotting: this is due to dysfunction of coagulation factor II - prothrombin. What kind of substance affects clotting was discovered only 11 years later, and this merit rightfully belongs to a research group at the University of Wisconsin led by Professor Karl Link. One of the researchers, Harold Campell, isolated dicumarol.
Dicumarol is a derivative of plant coumarin, the smell of which we smell next to freshly cut grass. However, coumarin itself does not affect coagulation, but acquires anticoagulant properties only after fermentation (metabolism by fungi of the genera Fusarium, Stachybotrys, Aspergillus, Monopodium and bacteria Clostridium Perfrigens, Escherichia Coli), which is what happened with moldy clover. The result is a full-fledged mycotoxin - dicoumarin.
People first started talking about it as a medicine in 1941. Karl Link, the same professor from Wisconsin, decided to profit financially from his work and register a new rat poison, which was in great demand on farms at that time. Especially for this purpose, in 1948, a new anticoagulant was synthesized and called it warfarin, not forgetting to reflect the group of discoverers (Wisconsin Alumni Research Foundation) in the name. The ending “-arin” hints at coumarin, of course, of which it is a derivative (4-hydroxycoumarin). And only 6 years later it began to be used for medical purposes. The mechanism of action was unknown for a long time, but today we can fully describe it.
Warfarin is called a vitamin K antagonist because it disrupts the synthesis of vitamin K-dependent blood coagulation factors, which are II (prothrombin), IX (Christmas factor), VII (proconvertin), X (Stuart-Prower factor), as well as proteins C (vitamin K-dependent proteolytic enzyme) and S (plasma glycoprotein). The listed coagulation factors depend on vitamin K functionally: the epoxy (oxidized) form of vitamin K is reduced to its hydroquinone form (reduced vitamin K) under the action of the enzyme vitamin K epoxide reductase. Oxidation to the epoxide form (reverse) occurs with the help of gamma-glutamyl carboxylase. It is this enzyme that converts inactive forms of coagulation factors into biologically active ones by carboxylation of their glutamate residues. After carboxylation, coagulation factors can interact with phospholipids of the vascular endothelium and participate in the hemostatic cascade (Fig. 1).
Figure 1 | The mechanism of action of warfarin
But then warfarin bursts in and irreversibly blocks the enzyme vitamin K epoxide reductase, therefore, vitamin K is not restored, and the entire cycle of transformations stops. Gamma-glutamyl carboxylase does not activate clotting factors. The latter circulate in the blood in a functionally inactive form; they are even given the special name PIVKA (proteins induced by vitamin K absence).
For example, the second factor blocked by warfarin, contained in the blood in an inactive form, is called PIVKA-II. Other indirect anticoagulants (phenindione, acenocoumarol, neodicoumarin) also work by this mechanism, but only warfarin has firmly entered into cardiological practice as the drug of choice for the prevention of thrombosis.
Since all these processes occur in the liver, at a systemic level, it is not possible to recreate the effect of the drug in vitro, as is the case with heparin. For the same reason, the effect of hypocoagulation does not occur immediately (after 5–6 days for warfarin, 4–5 days for acenocoumarol), but when the reserves of active coagulation factors in the blood are depleted.
Pharmacokinetics
The drug is used primarily for oral administration, as it is well absorbed from the gastrointestinal tract (80–90%) - therefore, it is convenient for long-term self-administration, but is also used in the form of intravenous injections.
Bioavailability when taken orally reaches 100%. The maximum concentration in the blood is after 4 hours. Capable of accumulation, both material (in the liver, especially with its pathology), and functional, reducing the rate of synthesis of coagulation factors. An important aspect is that warfarin binds to plasma albumin by 97–99%, and the drug has its effect only in free form.
Thus, it is necessary to be careful when combining warfarin with other drugs that also actively bind to blood proteins, since they can displace warfarin from binding to the protein, which increases the level of free (active) warfarin in plasma, and therefore increases the risk of bleeding.
Other drugs that increase the risk of bleeding when used together with warfarin:
- Antidepressants (serotonin reuptake inhibitors). They block platelet aggregation, and their administration together with warfarin increases the risk of bleeding.
- Antibiotics that inhibit the intestinal microflora that synthesizes vitamin K,
- Acetaminophen. Its active metabolite (N-acetylbenzoquinoneline) blocks vitamin K carboxylase even at a therapeutic dose, which is reflected when measuring INR.
99% of the drug undergoes biotransformation in the liver, and this is another pressing issue regarding the combination of drugs. Warfarin, in particular its active S-form, is metabolized in the liver with the participation of cytochrome P450.
Some drugs (for example, cotrimoxazole, metronidazole, ciprofloxacin, norfloxacin, pefloxacin, amiodarone, etc.) block cytochrome P450 and interfere with the biotransformation of warfarin in the liver, resulting in an increase in its concentration in the blood and an increased risk of bleeding.
But there are also drugs that increase the activity of cytochrome, for example, rifampicin, when taken the opposite occurs: warfarin is actively metabolized and excreted from the body, as a result of which the risk of thrombosis increases. Metabolites do not have anticoagulant activity and are excreted by the kidneys (90%) and bile (10%). The drug penetrates the placenta and, as you understand, we will return to this point in the “contraindications” section.
A minute of personalized medicine
The CYP2C9 gene encodes an enzyme involved in the metabolism of warfarin - cytochrome P450. Some alleles of this gene (CYP2C9*2 and CYP2C9*3) determine low enzyme activity, which means slow metabolism of warfarin, high concentration of the drug in the blood and its long-term presence there, hence a strong anticoagulant effect. Such patients require lower doses of the drug to achieve a therapeutic effect.
The VKORC1 gene is also known, encoding the enzyme vitamin K epoxide reductase, the “target” of warfarin. Patients with a G to A substitution at position 1639 of the polynucleotide express less enzyme and are more sensitive to warfarin, and therefore lower doses of the drug are indicated for them.
It seems that this does not find clinical use in modern realities, but the figures vary strikingly: 95% of the population of Asian countries have the A allele and are sensitive to low doses, while among Africans only 14% have it. Mutations in this gene can lead to complete resistance to warfarin.
Indications
The drug is used to prevent thrombosis and thromboembolism. Four pathologies are absolute indications for the use of warfarin for the prevention of thromboembolic complications:
- Atrial fibrillation;
- Venous thrombosis;
- TELA;
- Prosthetic heart valves.
It is also possible to use it in combination with antiplatelet agents to prevent thromboembolic complications in patients with myocardial infarction. It is also used in patients with AF after stenting in the form of triple antiplatelet therapy in combination with acetylsalicylic acid and a P2Y12 inhibitor (clopidogrel/ticagrelor).
However, recent studies show that replacing warfarin with dabigatran in TAT in the combination of aspirin + clopidogrel/ticagrelor has undeniable advantages due to a reduced risk of major or clinically significant minor bleeding.
Dosage regimen
To select the dose and monitor efficacy and safety, the international normalized ratio (INR) is used. This is an assessment method based on comparing the patient’s prothrombin time with the norm, which is expressed by the ratio (note - ISI - international sensitivity index, factory indicator of thromboplastin activity, written on the reagent label):
Prothrombin time, as we know from the course of normal physiology, is the time during which a fibrin clot forms in the blood when calcium chloride and thromboplastin are added to it, thanks to which it is possible to evaluate the external path of hemostasis and the activity of factors I, II, V, VII and X, three of which are blocked by warfarin.
The INR norm for a healthy person not taking warfarin is: 0,8–1,2.
The target INR values when taking warfarin are different for each pathology: for atrial fibrillation, the target INR range is 2–3 , for patients with a prosthetic valve, the INR is 2.5–3.5 .
It is worth remembering that when the INR increases above the recommended figures, there is a high probability of bleeding; when the INR decreases below 2, there is a risk of thrombosis, therefore, when treating with indirect anticoagulants, its strict control is necessary.
Since indirect anticoagulants reveal their therapeutic potential approximately on the 4th day of administration, to prevent thrombosis after cardiovascular accidents, its combination with LMWH (enoxaparin) is recommended according to the following scheme:
In case of asymptomatic risk of bleeding, proceed according to the following scheme:
- INR = 3.5–4.0 : reduce the single dose of the drug by a quarter of a tablet, check the INR after 1 day;
- INR = 4.0–5.0 : reduce the dose by half a tablet, control the INR every other day;
- INR more than 5 : discontinue the drug for a day, control after one day, start therapy with INR less than 3.5; subsequently the dose is reduced by 1 tablet.
If it is necessary to switch to NOAC therapy, it is necessary to bring the INR to <2 (drug discontinuation and daily monitoring of the INR). For your convenience, dear subscribers, we invite you to familiarize yourself with two algorithms for prescribing warfarin: British and American.
Side effects of warfarin
- Bleeding (mainly from the gastrointestinal tract, genitourinary system and even into the ventricles of the brain)
- Liver dysfunction;
- Allergic reactions;
- Necrosis of the skin of the extremities due to thrombosis in the first days of taking the drug (anticoagulant activity appears on the 4th day of use, therefore a combination of low molecular weight heparins and indirect anticoagulants according to the above scheme is necessary);
- Purple toe syndrome (big toe) - it is believed that indirect anticoagulants contribute to the deposition of cholesterol in the veins of the extremities, resulting in impaired blood flow, blood stagnation and soft tissue swelling;
- Teratogenic effect (warfarin penetrates the placenta and can affect the fetus, as it blocks osteocalcin, which leads to hypoplasia of the skull bones, in particular the nose);
- Miscarriages, uterine bleeding, fetal bleeding: all these are terrible consequences of taking warfarin during pregnancy.
Contraindications to taking warfarin
- Pregnancy;
- Erosive diseases of the gastrointestinal tract (erosive gastritis, peptic ulcer and duodenum, ulcerative colitis), the combined use of warfarin with NSAIDs for the listed pathologies increases the likelihood of bleeding from the gastrointestinal tract;
- Urolithiasis, hematuria;
- With caution - in case of liver pathology;
- Age over 80 years;
- Hemorrhagic stroke.
However, it is possible to use warfarin for chronic kidney disease of any stage, unlike NOACs. In case of massive bleeding (often gastrointestinal bleeding), a transfusion of fresh frozen plasma is necessary.
Also, in case of an overdose of warfarin, vitamin K preparations are used. A careful study of the mechanism of action of warfarin begs the question: it is not the vitamin that is blocked, but the enzyme that restores it - how can taking vitamin K change the situation?
The fact is that in addition to vitamin K-epoxide reductase, epoxide can also be reduced by DT-diaphorase, the action of which requires a significantly larger amount of vitamin K, which we will provide by introducing a vitamin K preparation, for example, Vicasol (menadione) or phytomenadione.
Vikasol is administered intramuscularly at a dose of 10–15 mg 2–3 times a day; oral administration of 15–30 mg three times a day is possible. It is also used three days before surgery to prevent massive bleeding. Phytomenadione is taken orally at 0.01–0.02 mg 3–4 times a day. Strict INR control is necessary to prevent thrombosis.
In conclusion, I would like to note that despite the fact that warfarin is the drug of choice for the prevention of thromboembolic complications of cardiovascular accidents, it is imperfect in many aspects: narrow therapeutic window, frequent laboratory monitoring, the influence of food and other drugs on the anticoagulant effect, slow onset and the end of the action.
They were replaced by NOACs, but were never forced out of use: warfarin is cost-effective, it can be used for CKD of any stage, and it is possible to assess the level of coagulation and select the dose, despite the obligation to frequently monitor them.
Sources:
- Wardrop D., Keeling D. The story of the discovery of heparin and warfarin //British journal of haematology. – 2008. – T. 141. – No. 6. – pp. 757-763.
- Kester M., Karpa KD, Vrana KE Elsevier's Integrated Review Pharmacology E-Book: with Student consult Online Access. – Elsevier Health Sciences, 2011.
- Kukes V. G., Mosolov S. N. Clinical pharmacology. – 2004.
- Richard D.H. et al. Lippincott's illustrated reviews: Pharmacology //Philadelphia. – 2006. – T. 3. – P. 413-415.
- Kharkevich D. A. Pharmacology. – GEOTAR-MED, 2003.
- Dean L. Warfarin therapy and the genotypes CYP2C9 and VKORC1. – 2016.
- Juurlink DN Drug interactions with warfarin: what clinicians need to know //Canadian Medical Association Journal. – 2007. – T. 177. – No. 4. – pp. 369-371.
- Martsevich S. Yu., Lukina Yu. V. Warfarin and its significance in the era of new oral anticoagulants. Issues of monitoring the effectiveness and safety of treatment // Rational pharmacotherapy in cardiology. – 2017. – T. 13. – No. 5.
It is important
Always tell any health care professional you see that you are taking anticoagulants. It is advisable to carry your “account” book or treatment diary with you.
Most dental procedures (except tooth extraction) can be performed without changing your treatment regimen. When removing a tooth, it is usually sufficient to use a tampon with a local hemostatic agent (aminocaproic acid, thrombin sponge).
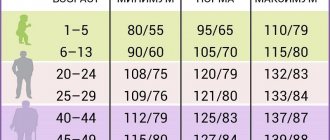
If you have problems with blood pressure, you need to regularly monitor it and maintain it at a level not higher than 130/80 mmHg.
Contraindications
Before taking medications, you need to take into account the contraindications that are indicated in the instructions for the drug:
- manifestation of high sensitivity to the components of the product or suspicion of hypersensitivity;
- acute bleeding;
- severe liver and kidney diseases;
- the first trimester of pregnancy and the last 4 weeks of gestation;
- acute DIC syndrome;
- thrombocytopenia;
- lack of proteins C and S;
- varicose veins of the digestive tract;
- aneurysm ;
- increased risk of bleeding, including hemorrhagic disorders ;
- stomach and duodenal ulcers;
- severe wounds, including post-operative wounds;
- lumbar puncture;
- bacterial endocarditis;
- hypertension malignant;
- intracranial hemorrhage;
- hemorrhagic stroke.
Warfarin and pregnancy
During pregnancy, taking warfarin is contraindicated. In the event of pregnancy, indirect anticoagulants are immediately discontinued; if further prevention of thrombosis is necessary, heparins are usually used. Therefore, if you suspect pregnancy, refrain from taking the drug until you consult your doctor.
It is possible to use warfarin during breastfeeding. Warfarin is excreted in breast milk in extremely small quantities and does not affect the baby's blood clotting processes, but for complete safety it is recommended to refrain from breastfeeding during the first three days of the mother's treatment with the drug.
Pharmacological properties of the drug Warfarin nikomed
Antithrombotic agent. Warfarin blocks the synthesis of vitamin K-dependent blood coagulation factors in the liver, for example, factors II, VII, IX and X. The concentration of these components in the blood decreases and the coagulation process is inhibited. The optimal effect is observed on the 3-5th day from the start of the drug. The effect of warfarin stops 3-5 days after the end of treatment. The drug is almost completely absorbed in the digestive tract. Binding to blood plasma proteins is 97–99%. Therapeutic concentration in blood plasma is 1–5 mcg/ml (0.003–0.015 mmol/l). In the human body, warfarin is found in the form of a racemic compound, and the levorotatory form has greater pharmacological activity than the dextrorotatory form. Metabolites produced in the liver are inactive or weakly active compounds. They are reabsorbed from bile, with the levorotatory form being metabolized more quickly. The elimination period of racemic warfarin is approximately 40 hours and is excreted in the urine.