Home » Hemorrhoids » Thrombosis of hemorrhoids
Sign up for a consultation with a proctologist for the treatment of hemorrhoids for 3,500 rubles and receive a treatment prescription within 30 minutes for 1 appointment
Find out what day you need to make an appointment to get a consultation without a queue.
Experience 44 years 73 operations per month 876 operations per year 171 reviews Author of 73 scientific papers Has 9 patents 6,818 requests per month
Call
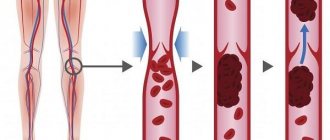
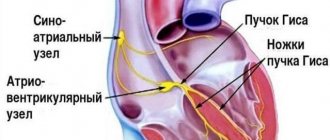
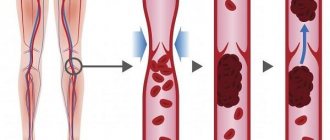
Thrombosis of hemorrhoids is a complicated stage of chronic hemorrhoids. The disease develops due to impaired bleeding. Blood clots form in the structure of the cavernous vascular plexuses. The acute process lasts for a week. After this, the thrombosed node is replaced by connective tissue. In the absence of timely treatment, necrosis of ulcerative formations on the intestinal mucosa develops.
As a result, complications arise: a blood clot that formed earlier blocks the vascular lumen and prevents the reverse flow of blood from the nodular protrusion. This is why blood clots occur.
Depending on the location, the following types of hemorrhoidal thrombosis are distinguished:
- interior;
- outer;
- combined;
Proctological pathology is classified into three degrees of severity, which have different etiologies, symptoms and neglect.
What are external hemorrhoids? A little anatomy
External hemorrhoids (plexuses) are formations located under the skin on the border of the anal canal and perianal (around the anus) skin. They are venous plexuses (Fig. 3). Usually they do not manifest themselves in any way, are not visible and cannot be detected by touch. As the condition worsens chronically
changes occur in internal hemorrhoids and in external hemorrhoids, leading to their enlargement and loss of connection with the muscular ring of the anal canal. However, the most significant changes in the external nodes occur when a blood clot occurs in them.
Rice. 3. Diagram of the anal canal, at the exit of which the external hemorrhoids are located (number 7 in the diagram).
Treatment of urethral polyps in women and men
It is extremely important to understand that at the first manifestations of the disease you need to consult a doctor. It is impossible to cure such a tumor with folk remedies or medications. Over time, the situation will only get worse. The only treatment method is surgery.
Preparing for surgery
Before the intervention, the patient needs to undergo urine and blood tests. Also, the doctor often prescribes diagnostic methods such as:
- urethroscopy;
- smear for sexually transmitted diseases;
- coagulogram.
Polypectomy techniques
The tactics for treating polyps of the urethra and bladder are removal of tumors with cleaning of the bed using an extremely gentle technique. The technique is selected taking into account the characteristics of the disease and the patient’s condition.
Preference is given to the TUR intervention technique - transurethral resection. Access to the tumor is carried out through the urethra - without punctures or incisions. To do this, microsurgical instruments and an endoscope are used - a device with a flexible cable, a miniature video camera and a light source. If, due to the location, size of the polyp, combined pathologies, and other factors, TUR is not possible, endoscopic access is used - without incisions, through punctures in the abdominal wall.
Anesthesia during surgery - local, epidural or general anesthesia (decided by the anesthesiologist after consultation and diagnosis). The duration of the intervention, depending on the volume, is 20-40 minutes. Open operations with opening of the abdominal cavity are rarely performed, in especially complex cases.
Features of the removal of urethral polyps in men and women
In women, polyps are more often localized outside the urethra or throughout the entire area of the urethra. In men - at the entrance of the urethra to the prostate and in the area of the seminal tubercle. When located in the lower parts of the urinary system in women, you can do without a urethroscope. In men and when urethral polyps are localized in the upper parts of women, TUR is used.
Content
Prevention of hemorrhoids is considered a pressing problem in Russian healthcare. After all, this pathology is the most common reason for men and women to consult a proctologist. The prevalence of the disease is 130-145 adults per 1000 population. The disease often leads to serious complications and significantly reduces the quality of life of patients 1 .
Why do hemorrhoids develop?
The best prevention of hemorrhoids is to combat the causes of their occurrence. Currently, the etiology of the disease is considered to be sufficiently studied, which makes it possible to select more effective measures for its treatment and prevention.
The main trigger of the disease is considered to be a violation of the relationship between the inflow and outflow of blood from the choroid plexuses of the distal rectum and anus. This is facilitated by increased pressure inside the abdominal cavity and congestion in the pelvis. Also, a significant role is played by dystrophic changes in the muscular-ligamentous apparatus, which holds hemorrhoids in one position 2.
The development of the disease is facilitated by the sedentary (adynamic) lifestyle of modern man. Sedentary work and constant presence at the computer create ideal conditions for the occurrence of pathological changes in the hemorrhoidal plexuses of the rectum. The following factors contribute to the formation of hemorrhoids:
- pregnancy and childbirth (this is why the prevention of hemorrhoids in women at the preconception stage (before conception) and during all three trimesters is so important);
- regular constipation or diarrhea;
- frequent straining during bowel movements;
- obesity;
- excessive consumption of hot, spicy foods that irritate the intestinal mucosa, coffee and alcohol;
- smoking;
- diseases of the pelvic organs, leading to stagnation in the circulatory system of the rectum (benign and malignant tumors, adhesions, etc.);
- vascular diseases (lack of valves in the drainage veins of the cavernous plexuses, etc.);
- heavy physical work, especially associated with lifting loads (this is why the prevention of hemorrhoids in men whose
- the profession is associated with forceful loads on the body);
- weightlifting;
- prolonged hacking cough.
Over time, under the influence of a complex of various factors, hemorrhoids can shift towards the anus and fall out. Other symptoms of the disease also appear, the main ones being bleeding and pain in the rectum 1,2,3.
Frequent increases in blood pressure (BP) are the cause of the development of serious diseases (stroke, myocardial infarction, etc.). Hypertension in Russia is diagnosed in every third elderly person. To combat hypertension, many patients have to take medications throughout their lives to prevent complications.
Modern pharmacological companies offer a large selection of drugs that are effective for hypertension. If you don’t know how to choose high blood pressure pills, check out the rating below. The TOP includes the best medications taking into account effectiveness, cost and reviews.
How does acute thrombosis of the external hemorrhoid manifest?
Patients with acute thrombosis of the external hemorrhoid complain of a protrusion, “bump” (neoplasm) and/or pain of varying intensity in the anus. The size of the “bump” can range from several millimeters to several centimeters and is often accompanied by swelling of the surrounding tissues (up to the entire circumference of the anal canal). In some patients, the disease proceeds without pain, but most assess the pain as significant or unbearable.
To assess the degree of pain, a special visual analogue scale is used, in which you can independently determine the severity of pain. After all, this is the key point when choosing a treatment method. Surgical treatment will be most effective when the severity of pain is 7 or more points, while for pain up to 4 points, a conservative method of treatment can be considered optimal.
Rice. Visual analogue scale for pain assessment.
Pain usually worsens during bowel movements and/or sitting. The pain and swelling can be severe, even unbearable for several days. The intensity of pain depends on the size of the blood clot and its location in relation to the anal sphincter muscles. In general, manifestations of the disease can persist for several weeks, in exceptional cases longer. Sometimes spontaneous evacuation of a blood clot from a hemorrhoid occurs. This is preceded by necrosis (destruction) of the skin over the thrombus, and the thrombus seems to “fall out” of the node. Externally, this is accompanied by the sensation of a “bursting” ball and the release of a small amount of blood. Usually, after evacuation of the blood clot, the pain and discomfort in the anus gradually decrease. However, necrosis of the mucous membrane above the thrombus does not always end only with the evacuation of the thrombus; necrosis can continue to spread to the hemorrhoid itself and surrounding tissues, which is why this condition requires consultation with a specialist. After acute thrombosis subsides, the patient is most often left with so-called “skin fringes” - excess skin where the thrombosis was. They do not require medical treatment, but may cause cosmetic discomfort.
Benefits of the procedure
Hemorrhoidal thrombectomy has many advantages:
- Efficiency;
After removing blood clots in the anus, the risk of recurrence of the disease is reduced to zero. Thanks to the use of anesthesia, the therapy is completely painless and does not cause discomfort to the patient.
- safety;
During surgery, healthy organs and soft tissues are not affected. The duration of thrombectomy is forty minutes, after which the patient can go home and continue treatment with medication.
- Availability.
The price of services is of great importance in our time. The cost of the procedure in the clinic gives everyone the opportunity to start a life without pain.
Thrombectomy of a hemorrhoidal node has virtually no contraindications and is safe for all age categories. After surgery there is no bleeding, which speeds up the wound healing process.
What causes acute thrombosis of the external hemorrhoid?
The occurrence of thrombosis is often caused by overflow of the veins of the external hemorrhoidal plexus with blood, followed by a slowdown in blood flow in these vessels and the occurrence of blood clots. Thrombosis against the background of venous congestion most often develops after sudden or prolonged stress. Classic examples of such overexertion are heavy lifting, straining during constipation or diarrhea, and childbirth. Chronic stagnation of blood in the pelvic organs (which includes the anal canal) occurs with prolonged sitting, excess body weight, and insufficient physical activity.
Features of diagnosing external hemorrhoids at the Laser Surgery Center “ATLANTiK”
We are distinguished by:
- Tactfulness and politeness, as well as professionalism of doctors;
- High-quality equipment for examining the rectum, equipped with the ability to photograph and video record the resulting images;
- Possibility of performing video sigmoidoscopy and video colonoscopy on the day of treatment;
- Possibility of collecting and performing tests on the day of treatment;
- Possibility of examination for oncology on the day of treatment;
- High accuracy of diagnoses.
For patients who live in other regions, we can offer preparation for examination and treatment on site on the day of treatment, a flexible schedule of consultations and operations.
How to distinguish acute thrombosis of the external hemorrhoid from other diseases?
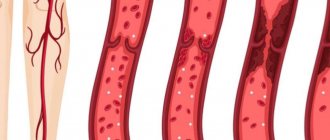
Usually, to diagnose acute thrombosis, it is enough to examine the patient and find out how the disease developed and what complaints are of concern. Upon examination, you can see an enlarged (sometimes up to several centimeters) node, often dark red in color, located outside the anus, possibly with a focus of necrosis in the center. When palpating (feeling) in the first few days, you can clearly identify a blood clot in the node; when examined at a later date, the blood clot is no longer so easy to determine; it begins to gradually “dissolve” and is partially replaced by scar tissue. Thrombosis of the external hemorrhoid must be distinguished from
strangulation of a prolapsed internal hemorrhoid. In this situation, prolapse of the internal hemorrhoidal node, normally located inside the anal canal, compression of its pedicle, in which the vessels feeding it pass, and disruption of the blood supply (ischemia) with death of the tissue of the node (Fig. 4 and 5). It is not difficult for a specialist to distinguish between these conditions, but it is quite difficult for a patient to independently understand which node is causing him discomfort. It is important to distinguish between these diseases, as their treatment varies significantly. When an internal hemorrhoid is strangulated, urgent surgical treatment is usually required.
Rice. 4. A strangulated prolapsed internal hemorrhoid with signs of tissue necrosis of the node.
Fig.5. Schematic representation of a strangulated internal prolapsed hemorrhoid.
Acute (exacerbation of chronic) anal fissure - accompanied by the same pain syndrome as with thrombosis, but much more pronounced at the time of bowel movement. With this disease, a rupture of the anal canal mucosa occurs. The appearance of an acute fissure is often associated with a reflex “protective” spasm of the sphincter apparatus, which complicates wound healing. Conservative and surgical treatment of diseases are different.
Acute paraproctitis - similarity with acute thrombosis lies in the appearance of a space-occupying formation in the anus, severe pain. Paraproctitis is an infectious and inflammatory disease with the formation of an abscess (abscess) in the pararectal area. The disease is accompanied by an increase in body temperature and general symptoms of intoxication. A mass formation in the anal canal area is much larger and more painful than with thrombosis. There is often discharge of pus onto the skin or into the lumen of the rectum. Ultrasound examination is used for accurate diagnosis. The disease is extremely dangerous due to the development of chronic purulent fistulas of the perianal area in the absence of adequate and timely treatment.
Stages of disease development
Chronic hemorrhoids are divided into four stages.
Stage I – Periodic bleeding from the rectum without prolapse of hemorrhoids. The method of treatment is conservative therapy.
Stage II - Hemorrhoids fall out during defecation, but are reduced on their own. There may or may not be bleeding. It is also possible for nodes to fall out during intense physical activity.
The second stage combines conservative treatment and minimally invasive proctological manipulations, which are carried out by Medical specialists in an outpatient setting.
Stage III – Manual assistance is required to reduce the nodes into the anal canal. Bleeding becomes more profuse, and periodic inflammation of the hemorrhoids is observed.
Treatment is surgical. The operations are performed by proctological surgeons at the Medical Outpatient Surgery Center.
IV – Hemorrhoids are constantly in a prolapsed state. This is the most difficult stage. Prolapse occurs even with the slightest stress: change in body position, coughing, release of gas from the intestines. The walls of the node are constantly injured and inflamed.
Only surgical treatment is indicated.
Is it always necessary to treat acute thrombosis of the external hemorrhoid?
The choice of treatment method for this disease is one of the most controversial issues in general proctology. Like hemorrhoids, acute thrombosis does not turn into cancer, does not cause deadly complications, but can significantly affect the patient’s quality of life; the pain syndrome is often described as “unbearable”, with which it is “simply impossible to live.”
Our Clinic has adopted a patient-centered approach to choosing a treatment method for acute thrombosis of external hemorrhoids: the doctor, together with the patient, determine how severe the symptoms are, how much the patient’s quality of life suffers, taking into account his employment, and choose a treatment method.
Acute thrombosis of the external hemorrhoid can be treated promptly (perform surgery), conservatively (take pills and use topical ointments and/or suppositories) or not treat at all, but choose a wait-and-see approach. Research and practical experience show that surgical treatment allows you to get rid of the manifestations of the disease in a shorter time; conservative treatment also allows you to get rid of the manifestations of the disease, but over a much longer time. The absence of any treatment also ends with recovery, the timing of which differs only slightly from the timing of intensive conservative treatment. The determining factor in the choice of treatment method is the patient’s choice and his assessment of the severity of the pain syndrome, therefore, the patient’s opinion is crucial for the choice of tactics. If the patient assesses the pain as unbearable, or he urgently needs to return to work, fly to another city or country, it is more reasonable to choose surgical treatment in the scope of removing the hemorrhoidal node or evacuating the blood clot from the node. Surgical treatment usually leads to faster relief of unpleasant symptoms. If the pain syndrome allows the patient to live fully in this condition or the patient is not ready for surgical intervention, it is possible to carry out conservative treatment aimed at reducing the pain syndrome and accelerating the process of organizing and resolving the blood clot.
Contraindications
___• The operation is not performed if the patient’s condition is extremely serious (general exhaustion, complications of cardiovascular diseases, sepsis). ___• Surgical interventions are not prescribed for severe pregnancy (severe anemia, poorly controlled early toxicosis with dehydration, late toxicosis with generalized edema, etc.).
Since thrombectomy is a minimally invasive (low-traumatic) operation, the procedure can be prescribed after the patient’s condition has been stabilized. The decision about surgery or its inadmissibility is made individually, taking into account all risk factors.
How to treat acute thrombosis of external hemorrhoids?
Possibilities of surgical treatment
There are two main operations for the treatment of acute thrombosis of an external hemorrhoid: removal of the entire node or just the thrombus from it. The first operation is called economical (partial) hemorrhoidectomy (removal of only the external hemorrhoid), the second is thrombectomy. Both operations are effective in terms of eliminating pain within 2-3 days after their implementation, however, after an operation to evacuate a blood clot, a relapse (reoccurrence of a blood clot) is more common.
Economical (partial) hemorrhoidectomy of a thrombosed node involves incision of the skin around the node, its isolation and removal along with the thrombus. The operation can be performed under local anesthesia.
After removal of a hemorrhoid, a small wound surface is formed, which can cause pain, especially during bowel movements. But usually the pain is much less pronounced than in the presence of a thrombosed node, and only sometimes requires taking tablet painkillers.
Thrombectomy is performed through a skin incision over the thrombus, after which the thrombus is removed and 1-2 sutures may be placed at the incision site. This intervention is almost always performed under local anesthesia.
Conservative treatment
Conservative treatment (tablets and local remedies - ointments and suppositories) is mainly aimed at relieving pain caused by a blood clot, reducing swelling and inflammation of the hemorrhoid, and normalizing the frequency and quality of stool. Pharmacies offer a large number of drugs for the treatment of hemorrhoidal disease, but they are all approximately equal in effectiveness and can be used to treat acute thrombosis of the external hemorrhoid. Local remedies (ointments and suppositories) mainly have an analgesic and anti-inflammatory effect. Topical agents with an anticoagulant effect in the treatment of acute thrombosis are effective only for the temporary prevention of new blood clots or, if the drug contains an analgesic component, for pain relief. Tablets are also used for pain relief (non-steroidal anti-inflammatory drugs, paracetamol) and normalization of venous blood flow in the pelvis (in the rectal area), for example, flavonoids. In addition, conservative treatment is also carried out after surgery to eliminate possible postoperative symptoms. A conservative treatment regimen can only be determined by a specialist, and it is better to select a combination of drugs in each specific case, depending on the characteristics of each patient.
Features of the postoperative period
After the operation, each patient feels significant relief and a decrease in pain intensity, which subsequently disappears completely after two to three days. In some situations, continued pain relief may be necessary for a short period of time. First of all, after surgery, the patient needs to normalize stool, which means softening stool and minimal straining. For this purpose, a special diet and medications (suppositories) are prescribed to soften the stool.
Often, within the first week after surgery, patients return to their normal lifestyle.
Don't put off visiting your doctor. Take care of your health. After all, the effect of treatment directly depends on timely diagnosis and treatment of the disease. Only a certified specialist will be able to draw up an individual treatment plan for you, depending on your individual characteristics and the course of the disease itself, and will lead you to a speedy recovery.
What will happen after the operation?
Typically, patients feel dramatic relief after surgery and note a decrease in pain (Fig. 6). Sometimes continued minimal pain therapy is required. The main task of the patient in the postoperative period is to normalize stool: soft stool causes much less pain during bowel movements than dense stool. As a rule, patients return to their normal lives 2-3 days after surgery, sometimes the very next day.
a) b)
Rice. 6. View of the anus before (a) and immediately after removal of the external hemorrhoid (b). Before the operation, the patient rated the pain level as 8 out of 10, immediately after the operation it was 4 out of 10.
Why is thrombosis dangerous?
Firstly, thrombosis never resolves on its own. The longer you delay treatment, the worse the pain.
Secondly, over time, tissue necrosis can occur when thrombosed nodes fall off and ulcers form in their place. The ulcers gradually increase in size, and purulent paraproctitis develops, the treatment of which may require serious surgery.
Don’t delay in contacting a proctologist! In most cases, hemorrhoidal thrombosis can be cured in 1 visit to the doctor.
Are there ways to prevent relapses/recurrences of the disease?
Prevention of relapse of the disease is based on excluding possible causes of thrombosis. These include hard stools, constipation or diarrhea, “reading on the toilet,” insufficient or, conversely, excessive physical activity (weightlifting, fitness), and prolonged sedentary work. Unfortunately, there are no unambiguous methods for preventing the occurrence of acute thrombosis of the external hemorrhoid; we can only reduce the likelihood of its occurrence, but not completely eliminate it. However, it should be noted that with conservative treatment the likelihood of recurrence of the disease is higher than after operations.
How is the operation performed?
The procedure can be performed in a gynecological-style chair or on a couch and takes a few minutes. First, doctors give an anesthetic injection that “freezes” the tissue, just like in a dentist’s office. Therefore, the patient is conscious, but does not feel pain.
The surgical intervention takes several minutes and involves three manipulations: ___• opening the affected node (small incision), ___• removing the blood clot, ___• stopping the bleeding (the wound can be sutured, but more often it is not sutured)
After the procedure you can go home.
The exception is those cases of thrombosis when severe complications occur (gangrene of the node, paraproctitis, severe bleeding) that require hospitalization.
What should pregnant women and postpartum women/mothers with acute thrombosis do?
According to statistics, about a quarter of pregnant women and almost half of postpartum women experience various manifestations of hemorrhoidal disease, the most painful of which is acute thrombosis. Usually, postpartum women and especially pregnant women, in response to their complaints to the doctor, hear an offer to be patient. This approach is dictated by the fact that there are many contraindications to the use of the vast majority of medications in pregnant women, and surgical intervention is regarded by the medical community as a factor that can provoke childbirth or stop the process of breastfeeding. In practice, this means that regardless of the severity of the pain syndrome, sometimes very significant, women are forced to remain without any effective treatment. Pain due to thrombosis, in turn, can worsen the psychological state of pregnant or postpartum women and lead to undesirable consequences during childbirth (premature birth) or during breastfeeding (refusal to breastfeeding). Our clinic is a supporter of a personalized approach to the treatment of acute thrombosis in such women. If acute thrombosis categorically prevents the patient from living, it should be actively treated using the entire arsenal of means used in ordinary patients, but taking into account contraindications for medications. In pregnant women in the second and third trimesters, it is possible to perform an operation to remove a thrombosed node (Fig. 7), as well as in postpartum women and women in labor (Fig. 8). During pregnancy, there are some restrictions on the local and general anesthetic drugs that can be used. Specific medications should be selected jointly by both the coloproctologist and the obstetrician so as not to harm the fetus or newborn. The specialists of our Clinic have experience in treating both pregnant and postpartum women with manifestations of acute thrombosis of the hemorrhoid with very good results, reviews of which our patients leave on our website, among other things.
a) b)
Rice. 7. Acute thrombosis of the external hemorrhoid in a 38-week pregnant woman.
Before surgery, pain was rated 8 out of 10, immediately after surgery 3 out of 10.
a) appearance of a thrombosed external hemorrhoid with necrosis, b) appearance after removal of the thrombosed node.
a) b)
Rice. 8. a) acute thrombosis of the external hemorrhoid with severe swelling in the patient on the 5th day after birth, b) the patient’s condition on the 7th day after surgery. On the first day after surgery, pain decreased from 9 to 4 out of 10.
You can read about the treatment of other manifestations of hemorrhoidal disease in pregnant women and postpartum women in the section Hemorrhoids in pregnant women .
Possible complications of the procedure
After a minimally invasive surgical method, complications are possible, as after any other procedure. In most cases, rehabilitation is short-term and healing proceeds without any problems. However, if the patient does not observe the rules of personal hygiene and does not listen to the doctor’s recommendations, the condition worsens and the pain does not go away.
Complications include pain, which intensifies with movement and walking. For such symptoms, the patient is prescribed painkillers and ointments that have an analgesic effect. Candles are also effective. They eliminate swelling and inflammatory processes. A few days after taking the medications, the symptoms disappear.
Possible bleeding. Hemorrhage occurs if the stitches were not applied correctly or hygiene was not observed. An infection may also develop that affects healthy internal organs and negatively affects the functionality of the body.
To avoid the re-development of hemorrhoids, you should follow the rules of hygiene, wash the anal area after each bowel movement, and follow a strict diet. If you have constipation, you should immediately consult a doctor, as the vessels may become deformed again, resulting in anal fissures.
Proctologists and nutritionists advise including vitamins and minerals, plenty of fluids, fruits and vegetables in your diet. Dairy products have a positive effect on intestinal function.
What to do if you have undergone a course of conservative treatment for thrombosis
The abundance of means for the conservative treatment of thrombosis and often the doctor’s disposition to use this technique leads to the fact that most thromboses are treated conservatively. Patients come to our Clinic at different stages of the course of conservative therapy. Often this is a situation where, immediately after the occurrence of a blood clot, conservative therapy was started, some relief of the condition occurred, the pain syndrome decreased, but a “bump” remains in the anus and some pain. Sometimes completely healthy people come in who experienced an episode of acute thrombosis several months or years ago and are now concerned about the presence of skin “fringes,” excess skin in the anus that remain after the acute condition has resolved. They can interfere with the proper hygiene of this area and affect intimate life. What to do in this situation? And again, the main thing for the doctors of our Clinic will be the patient’s opinion. If you want to get rid of the manifestation of acute thrombosis, even if conservative treatment has already been carried out, a lot of time has passed - this can be done surgically.
When is thrombectomy necessary?
At the initial stages of development of thrombosed hemorrhoids, doctors prescribe drug therapy. It consists of using anti-inflammatory ointments and suppositories. The latter reduce swelling and relieve pain. Surgical treatment of hemorrhoids is recommended only at the third stage of the disease.
There are certain indications for thrombectomy:
- severe pain syndrome;
- acute form of hemorrhoids;
- significant risks of developing necrosis;
- insufficient effectiveness of drug treatment.
In some cases, such surgical intervention is the only acceptable method of treating hemorrhoids. This applies to those patients who suffer from allergies to medications and are in poor health.
What to consider when choosing a doctor and medical institution
If you are looking for a medical institution where to go for consultation and treatment of acute perianal thrombosis, then you need to pay attention to several factors.
- The institution has a proctological, and not just a general surgical or oncocoloproctological specialization.
- Knowledge of the Clinic staff about all possible methods of treating acute perianal thrombosis
- Possibility of performing minor coloproctological operations in a hospital setting at the Clinic
- Possibility of performing surgical treatment in the Clinic for “special” groups of patients - pregnant women, patients of the older age group
Is preparation for surgery necessary?
Often, surgical treatment is performed on an outpatient basis using local anesthesia. Therefore, hospitalization and further treatment in a hospital may not even be required. Depending on the clinical situation, the operation can also be performed in an operating room. Then you will need to fulfill a list of requirements before hospitalization, including additional examinations and tests. Special bowel preparation before surgery is not needed in this situation.
surgical treatment of thrombosis