Tachycardia, which is characterized by increased heart rate, often has nothing to do with blood pressure readings. A high pulse with normal pressure, if it persists for a long time or occurs with a certain frequency, indicates the development of serious pathologies. To establish the cause and make an accurate diagnosis, you should undergo a full examination.
Validol
Validol belongs to the group of vasodilators and has a sedative effect. These tablets are good for high heart rate, but have virtually no effect on blood pressure levels.
Important! The product is indicated for sublingual (sublingual) use. Thanks to this, the therapeutic effect is achieved 3-5 minutes after the tablet is dissolved.
Contraindications:
- hypersensitivity to the components of the drug;
- sugar intolerance;
- diabetes mellitus (with caution).
Side effects:
- allergic reaction - itching, skin rashes, urticaria, Quincke's edema;
- lacrimation;
- nausea;
- dizziness.
Adverse symptoms disappear on their own after reducing the dosage or stopping therapy.
Why does rapid heartbeat occur?
The occurrence of rapid heartbeat can be triggered by various factors, including both the body’s natural reactions to the influence of external stimuli and the presence of pathological changes in organs or systems.
Rapid pulse has two forms of occurrence: physiological and pathological. Physiological palpitations appear against the background of psychoemotional disorders, excessive physical exertion, prolonged exposure to sunlight, overeating, insomnia, consumption of alcohol, caffeine, drugs, hormonal activity with increased arousal. Heart rhythm disturbances due to such influence factors are a natural compensatory reaction of the body. Treatment of physiological tachycardia is not required. To stop an attack, just calm down and rest.
The pathological form of a rapid pulse occurs due to the presence of concomitant diseases, in which rhythm disturbance acts as a symptom, and treatment of cardiac tachycardia with tablets is an integral process.
Such pathologies include:
- hypertonic disease;
- heart disease (myocarditis, cardiomyopathy, heart failure);
- pathologies of the endocrine system (hypothyroidism, hypoglycemia, diabetes mellitus);
- diseases of the hematopoietic organs (anemia, leukopenia);
- renal failure;
- malignant neoplasms;
- internal bleeding;
- brain damage;
- infectious pathologies.
Treatment of palpitations, which is determined solely by the attending physician, directly depends on the etiology of the condition.
In pregnant women, the condition is diagnosed in 70%. The increase in pulse rate in this category of patients occurs by 10-20 units even in a normal state. This process is natural, since a woman gains weight and often succumbs to stress. As a medicine for discomfort during tachycardia, you can use sedative drugs with a natural composition, for example, valerian or motherwort.
Asparkam
Asparkam is a medicine from the group of antiarrhythmics. It also does not cause a decrease in blood pressure. The daily dose for an adult is no more than 6 tablets, which must be divided into three doses.
Asparkam should be taken after meals.
Contraindications:
- increased sensitivity to the component composition;
- cardiogenic shock;
- severe myasthenia gravis;
- dehydration;
- increased content of magnesium and potassium in the body;
- oliguria;
- anuria;
- metabolic acidosis;
- atrioventricular block 2–3 degrees;
- liver dysfunction;
- high risk of developing edema.
Side effects:
Causes of rapid heart rate with normal blood pressure
- nausea, vomiting, epigastric pain;
- loose stools;
- dry mouth;
- abdominal discomfort;
- decreased blood pressure;
- myocardial conduction disturbance;
- paresthesia;
- convulsions;
- skin rashes;
- itching;
- facial redness;
- feeling of heat.
Pathological causes
A rapid pulse can be observed against the background of normal blood pressure with congenital and acquired heart defects. These pathological conditions are characterized by a variety of manifestations and have varying degrees of danger. In most cases, the problem can only be eliminated surgically.
Another common cause of rapid pulse associated with the development of cardiac pathologies are inflammatory diseases that affect the structure of the heart muscle. These are myocarditis, endocarditis, rheumatism, etc. Without appropriate therapy, these diseases pose a threat to life.
Rapid pulse also occurs for the following pathological non-cardiac reasons:
- Dehydration. When the body loses a lot of fluid, the blood thickens. This increases the load on the heart muscle, which causes it to contract more intensely.
- Infectious diseases. When the temperature rises, the body becomes intoxicated. In order to quickly remove harmful substances from the body and normalize the condition, the heart begins to pump blood faster.
- Neurotic diseases. The level of stress increases in such cases due to the release of large amounts of stress hormones.
- Hormonal disorders. As a rule, they are associated with dysfunction of the thyroid gland and adrenal glands. An increased amount of hormones leads to intoxication of the body. Against this background, the heart muscle begins to work more intensely.
- The occurrence of severe bleeding. This is due to a violation of the volume of blood circulating in the body. To provide tissues with the necessary amount of nutrients and oxygen, it is necessary to accelerate the pumping of hematological fluid through the vessels.
- Anemia. Most often, increased heart rate is observed with iron deficiency anemia. Additionally, increased fatigue with minimal physical activity and deterioration of the condition of the skin and nails are noted.
Bisoprolol
Bisoprolol is used to normalize pulse at high blood pressure. The active substance is bisoprolol fumarate. The drug belongs to the group of β1-blockers. It has the following effects: antianginal (elimination of symptoms of myocardial ischemia), antiarrhythmic (reduces heart rate), antihypertensive (normalization of blood pressure).
Important! The drug has a fairly large list of contraindications, so before you start taking it you need to make sure that they are absent.
During treatment, a person may experience:
- headache;
- dizziness;
- increased fatigue;
- flushes of blood to the face;
- sleep disorders;
- depression, hallucinations (rare);
- paresthesia;
- disruption of tear production;
- conjunctivitis;
- pain in the abdomen;
- nausea, vomiting;
- stool disorders - diarrhea and constipation are possible;
- muscle weakness;
- convulsions;
- increased sweating;
- bradycardia.
The drug is prescribed with caution to patients with psoriasis, diabetes mellitus in the stage of decompensation, predisposition to allergic reactions and those people whose work is associated with a high speed of psychomotor reactions.
Anaprilin
Anaprilin belongs to the group of beta-blockers. It has hypotensive, antiarrhythmic and antianginal properties. The active ingredient is propranolol. The drug is used if the blood pressure is high and the pulse is significantly increased.
The drug is effective in the initial stage of arterial hypertension, so the drug is used in young patients. A decrease in systolic pressure is accompanied by a decrease in the frequency of myocardial contractions.
Anaprilin is part of the group of beta-blockers
Contraindications:
- arterial hypotension;
- individual intolerance to the component composition;
- heart failure;
- atrioventricular block;
- sinus bradycardia;
- diabetes;
- predisposition to the development of bronchospasm;
- myocardial infarction;
- bronchial asthma;
- period of gestation and breastfeeding.
Side effects: bradycardia, bronchospasm, nausea, vomiting, muscle weakness, hypoglycemia, blurred vision, decreased potency, heart failure. If the regimen and dosage of the drug are not followed, the development of the following conditions cannot be ruled out: arrhythmia, convulsions, difficulty breathing, bronchospasm, dizziness, heart failure.
In case of overdose, Anaprilin can greatly reduce the pulse. The drug should absolutely not be combined with alcohol intake. In this case, death cannot be ruled out. The medicine cannot be combined with antipsychotics and tranquilizers. In the case of long-term course treatment with Anaprilin, the use of cardiac glycosides is recommended.
Physiological reasons
An elevated heart rate can occur for various physiological reasons. In this case, there are no serious threats to human health. Most often, an increase in indicators is noted during intense physical activity that does not correspond to the age and capabilities of a particular person. For example, the heart rate increases in people without adequate physical training after climbing stairs or lifting a heavy load.
Mental stress also causes a high heart rate. This condition is often noted by students when preparing for serious exams or by employees of enterprises before signing important documents. The cause of an increased heart rate against the background of normal blood pressure can be any stressful situations and an unstable emotional situation. In such cases, the occurrence of internal anxiety, sleep disturbances, and in severe cases, panic attacks occur.
Other common physiological causes:
- Climatic conditions. In particular, heat is often a provoking factor. Against this background, the concentration of oxygen in the blood decreases, so the heart begins to pump hematological fluid through the vessels faster in order to prevent hypoxia.
- Drinking large quantities of drinks that have tonic properties. First of all, these include tea and coffee.
- Smoking, drinking alcohol and using drugs. Against the background of addictions, vasoconstriction and impaired blood flow occur. This increases the load on the cardiovascular system.
Persen
Persen belongs to the group of herbal preparations. Extracts of valerian, lemon balm, and peppermint are used as active ingredients. Thanks to its complex composition, Persen has a calming (due to the presence of valerian), mild sedative and antispasmodic effect. The pulse-lowering ability is based on calming the human central nervous system.
Contraindications:
- individual intolerance to glucose, lactose;
- lack of sucrose;
- diseases of the biliary tract – gallstones, cholangitis and others;
- arterial hypotension;
- bearing a child and the period of breastfeeding;
- children's age - Persen is not prescribed to children under 12 years of age;
- intolerance to the component composition of the drug.
In the presence of gastroesophageal reflux disease, the drug is prescribed with caution. During treatment, allergic reactions and constipation may develop. The tablets should be taken orally with the required volume of any liquid.
Persen is a herbal preparation with a calming effect
The duration of the course is no more than 1.5 months. After stopping treatment, withdrawal syndrome does not develop. An overdose of Persen (in case of taking more than 60 or more tablets at the same time) is indicated by the appearance of nausea, general weakness, dizziness, and hand tremors. Treatment of the condition is symptomatic.
The drug should be taken carefully with antihypertensive and hypnotic drugs, since Persen enhances the effect of these medications. If such a need arises, dosage adjustments will be required.
Tablets for tachycardia: what to take if your heart rate is high?
The doctor prescribes therapy for palpitations depending on the cause that triggered the development of the pathological process. The basis of drug treatment is antiarrhythmic drugs, which are supplemented with sedatives and antipsychotics. In severe forms of tachycardia, doctors recommend a comprehensive diagnostic examination (ECG, Holter monitoring, endocardial mapping), which will allow an accurate diagnosis and the cause of the rhythm disturbance to be established.
So, what can you drink in case of an attack of tachycardia without putting your life in danger?
Sedatives. If a rapid pulse occurs due to physiological factors (stress, physical activity), it is enough to take a sedative and try to relax as much as possible. The best options are tablets or infusions of valerian, motherwort, hawthorn, and peony. They are made on the basis of natural ingredients and have no special contraindications. The mechanism of action of such substances is their influence on the inhibitory receptor system, which causes a general relaxation of neural activity.
In the presence of etiological pathologies, sedatives for palpitations are used only in complex therapy, if this remains necessary.
Antiarrhythmic drugs. They have a direct effect on the myocardium. Such drugs include membrane stabilizing substances, calcium antagonists, beta blockers, cardiac glycosides. Each of these groups is prescribed taking into account the type, mechanism and cause of rhythm disturbance, the definition of which is a necessary measure of their application.
Membrane-stabilizing substances are tablets for rapid heartbeat, which help slow down the rate of transfer of electrical potentials responsible for myocardial contractility.
These include:
- Moderate to strong sodium channel blockers. The action of medications is to block currents generated by sodium potential. The use of drugs reduces the electrical activity of cardiomyocytes by reducing the total action potential.
Representatives: “Disopyramide”, “Quinidine”, “Mexiletine”, “Propafenone”.
- Potassium channel blockers. Drugs in this group affect the process of potassium entering the cell, changing the state of the channels through which the trace element enters. A change in its concentration changes the potential ratio on different sides of the membrane, causing a decrease in the electrical activity of myocardial cells.
These are the drugs "Amiodarone", "Dronedarone".
Beta blockers. This is a group of pharmaceutical drugs that have a blocking effect on beta-adrenergic receptors, making them the basic drugs for tachycardia. Beta blockers are an effective remedy for more than just heart palpitations. The group is included in the treatment protocols for myocardial infarction, hypertension, coronary artery disease and heart failure.
The action of beta blockers inhibits the stimulating effect of the hormone adrenaline, as a result of which the contractility of the heart decreases, myocardial conductivity is inhibited and, as a result, the rhythm slows down.
These are the drugs “Atenolol”, “Labetolol”, “Carvedilol”, “Nebivolol”, “Betaxolol”.
Calcium channel blockers. Calcium antagonists promote relaxation of the smooth muscles of the myocardium and arterial walls, and also limit the absorption of calcium into the myocardium. As a result, the strength of the “calcium current” decreases, which leads to a slowdown in the frequency of myocardial contractions, dilation of the arteries, and a decrease in afterload on the myocardium.
If you want to choose a drug for tachycardia, choose a selective beta blocker in a standard single dose (in the absence of prescribed contraindications). This group of remedies will quickly and effectively help you cope with palpitations, gaining time to make an appointment with a cardiologist.
Many calcium channel blockers are not prescribed for tachycardia (Amlodipine) because they have a peripheral effect. They relax the blood vessels, but do not affect the contractile velocity of the myocardium, which does not change the rhythm of the cardiac cycle.
Cardiac glycosides . Digoxin, a cardiac glycoside based on digitalis, can reduce contractility during tachycardia. It is the drug of choice for heart failure accompanied by fibrillation. The drug slows down the rate of transmission of electrical impulses from the atria to the ventricles, but does not have an immediate effect. Medicines from the glycoside category are prohibited for independent use, as they have a number of severe side effects and are indicated for a narrow category of patients.
Each remedy from the presented list is prescribed exclusively by the attending physician. It is the cardiologist who determines what needs to be used based on etiological factors.
Valerian
To normalize a rapid pulse with normal blood pressure, you can use valerian tablets. They contain an extract from the plant as the main active ingredient. The drug helps not only to lower the heart rate by reducing the degree of excitability of the central nervous system, but also has a hypnotic and sedative effect.
Important! The sedative effect develops slowly but is stable.
Contraindications:
- individual reaction to the components of the tablets;
- depression and other conditions accompanied by central nervous system depression;
- galactose intolerance;
- lack of lactase;
- glucose-galactose malabsorption syndrome.
Side effects:
- increased drowsiness;
- dizziness;
- feeling depressed;
- poor performance;
- headache;
- nausea;
- allergic reactions - skin rashes, itching, local swelling - in case of intolerance to the component composition of the drug.
To eliminate unpleasant symptoms, it is necessary to reduce the dosage or completely stop taking Valerian. According to the instructions, adults and children over 12 years of age need to take one or two tablets three times a day. They must be swallowed without chewing, washed down with the required volume of any liquid.
The decrease in heart rate, due to a decrease in the excitability of the central nervous system, occurs slowly. For this reason, the drug is not suitable for emergency use. An overdose is indicated by:
- dizziness;
- drowsiness;
- headache;
- lethargy, general weakness;
- hand trembling;
- dilated pupils;
- visual and hearing impairment;
- feeling of tightness behind the sternum.
Treatment of the condition involves gastric lavage and taking activated carbon tablets. If necessary, carries out symptomatic therapy. Valerian enhances the effect of ethanol, antispasmodics and sedatives. If a person simultaneously takes synthetic sedatives, he needs constant medical supervision.
New generation of drugs
New generation drugs that reduce the pulse to normal but do not reduce blood pressure include Ivabradine and Coraxan
Ivabradin
Ivabradine belongs to the group of antianginal and anti-ischemic drugs. The decrease in heart rate at rest occurs by approximately at least 10 beats per minute. The myocardium works in a more relaxed mode. Additionally, there is a decrease in oxygen consumed by the heart muscle.
Contraindications:
- myocardial infarction;
- significant reduction in blood pressure;
- bradycardia;
- cardiogenic shock;
- sinoatrial block;
- chronic heart failure;
- lactation;
- presence of an artificial pacemaker;
- unstable angina;
- pregnancy;
- allergy to the active ingredient;
- age up to 18 years.
When using Ivabradine, the likelihood of developing bradycardia is minimal
Side effects:
- bradycardia;
- headache;
- dizziness;
- extrasystoles;
- fainting conditions;
- muscle cramps;
- nausea;
- diarrhea/constipation;
- shortness of breath, etc.
Coraxan
Coraxan belongs to the group of antianginal drugs. The active ingredient of the drug is ivabradine. The medicine helps normalize heart rate without having any effect on blood pressure.
Contraindications:
- acute period of myocardial infarction;
- intolerance to the components of the drug;
- bradycardia (with heart rate less than 60 beats per minute);
- cardiogenic shock;
- renal/heart failure;
- arterial hypotension;
- non-adaptive artificial pacemaker;
- age up to 18 years.
Coraxan can be taken with caution and under constant medical supervision (in a hospital setting) in the following cases: congenital long QT syndrome, recent ischemic stroke of the brain, second-degree atrioventricular block.
Coraxan is a dose-dependent drug, therefore, if the prescribed dosage is exceeded, the development of the following side effects cannot be ruled out:
- feeling of heartbeat;
- atrioventricular block;
- acquired weakness of the sinus node;
- atrial fibrillation;
- headache;
- allergic reactions;
- increased drowsiness, fatigue;
- general malaise.
High pulse. Why does this happen? Is it dangerous?
By high pulse we mean an acceleration of the heart rate above 90 beats per minute. It must be borne in mind that the pulse range from 60 to 90 implies a somatically healthy body, for example, with coronary heart disease, 90 beats is no longer normal, since in conditions of constant oxygen deficiency, the most complete blood supply is to the coronary arteries (vessels that directly supply the heart itself) occurs at a frequency of 60 to 65 beats per minute.
Consequently, if a patient with the above pathology constantly has a heart rate above 80 beats per minute, then his shortness of breath will gradually increase, swelling of the legs will appear and heart failure will worsen.....
What types of high heart rate are there?
There are several options for high heart rate:
- The pulse rises during exercise or emotional stress, or when using, for example, coffee, smoking, using energy drinks, or fear. When the stress factor disappears, it returns to normal.
- Heart rate rises regardless of physical activity. You can calmly watch TV, or drink tea, or sit on the sofa, lie in bed - and suddenly it begins to rise sharply. You begin to feel weakness, palpitations, there may be other symptoms in the form of increasing shortness of breath, chest discomfort, unfortunately, there are options when a person, at this moment, loses consciousness, which is a prognostically unfavorable sign. This phenomenon either stops on its own (sometimes, on the recommendation of loved ones, Corvalol and other medications available in the house are used, which is not always correct), or the attack stops by calling an ambulance. The duration of this phenomenon can vary - from a few seconds to several days, or, if professional help is not provided, it can end fatally.
- pulse is always high - both day and night (exceeds 90 beats per minute)
In all the above-mentioned situations, the pulse can be either uniform (simply fast), or uneven or irregular (sometimes faster or slower).
In the first situation, when we talk about the presence of some kind of stress factor, this is, as a rule, a normal, physiological response of the body. In the remaining two cases, it is already a pathology and requires clarification of the causes of such phenomena and appropriate treatment.
What is this pathology called?
These phenomena are called tachycardia (tachyarrhythmia). There are many types of arrhythmias. The most dangerous of them are ventricular tachycardias (when the pathological focus is located directly in the ventricles of the heart). Unfortunately, this type of arrhythmias most often manifests itself as a pronounced deterioration in well-being in the form of syncope (loss of consciousness) and, in the absence of outside help, can lead to death.
It is necessary to take into account that the concept of “syncope” is very broad and can occur not only for this reason, but also, for example, during asystole (temporary cardiac arrest) and in other situations.
Why is this happening?
The reasons for these manifestations can be divided into two groups:
1. Having an “wrong” lifestyle that causes overstrain of the heart (anything that changes the electrolyte composition of the heart (balance of potassium, magnesium, calcium, sodium, etc.) can cause a high pulse):
- Alcohol and smoking (we are not trying to take away the joys of life from you, but if genetics has “awarded” you with the ailments described above, then you have to choose in favor of health and give up something. These two “substances” indeed significantly affect the electrolyte composition of the heart muscle)
- Brewed coffee
- lack of sleep, overwork
- energetic drinks
- excessively intense physical activity (otherwise, additional intake of vitamins and microelements is necessary, but even this may not help)
- emotional stress
2. Presence of congenital and/or acquired disease:
- hypoxia (lack of oxygen), for example, lung diseases (COPD, bronchial asthma)
- dehydration, for example, due to overdose of diuretics or insufficient fluid intake.
- pathology of the thyroid gland in the form of thyrotoxicosis (hyperfunction of the thyroid gland)
- autonomic disorders (disorder of the autonomic nervous system is manifested by various functional disorders with a disorder of vascular tone and the development of neuroses
- overweight
- various heart diseases (WPW syndrome, long QT syndrome, Brugada syndrome, short PQ syndrome, coronary heart disease, myocarditis, pulmonary embolism (PE), heart attacks, various cardiomyopathies, etc.)
- anemia (low hemoglobin in the blood)
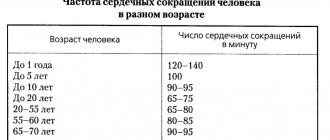
- fever (an increase in body temperature by one degree increases the pulse by an average of 10 beats per minute).
What examinations should I undergo?
At the outpatient stage, the following examinations are most often prescribed:
- electrocardiogram
- daily (Holter) ECG monitor (quite often the monitor does not detect arrhythmia, since it does not happen every day; in this situation, this study is used, among others, to exclude contraindications when prescribing antiarrhythmic therapy.
- if necessary, a stress test (some variants of arrhythmias appear only during exercise)
- thyroid hormone tests (TSH or T4) to rule out hyper or hypothyroidism
- a routine clinical blood test to determine hemoglobin levels.
24-hour (Holter) ECG monitor
How to treat high pulse?
- exclusion of the provoking factors described above
- treatment of the underlying disease
- if tachycardia persists, symptomatic (conservative) therapy is prescribed; if there is no effect or if there are indications, surgical treatment is performed.
The operation involves cauterizing the area of the heart that causes tachycardia.
Under local anesthesia, a puncture is made in the vessel, usually in the area of the wrist joint or inguinal fold, the conductor is inserted into the heart cavity, the localization of the source of arrhythmia is searched and ablation (cauterization) occurs, and also, in case of life-threatening tachycardias, an ICD (cardioverter) can be installed - defibrillator, a device that releases a shock and restores the rhythm when an arrhythmia occurs)
Unfortunately, surgery to cauterize the source of arrhythmia does not provide a 100% guarantee of the absence of relapse, but the probability of cure is above 90%.
How to stop an attack of high pulse once, you need to consult your doctor, since these drugs are selected individually, taking into account contraindications.
Thank you for your attention. See you!
Additional recommendations
High pulse and low blood pressure are a serious condition, since many drugs intended to normalize heart rate further reduce blood pressure. Beta-blockers, cardiac glycosides, medications intended to replenish magnesium and potassium deficiency, drugs with a sedative effect, and tranquilizers can stabilize the pulse and at the same time increase blood pressure.
For low pulse and high blood pressure, medications should be selected by the attending physician. With such a combination, there are no emergency remedies. The most commonly used long-acting antihypertensive (BP-lowering) drugs are:
- angiotensin receptor blockers – Valsacor, Lozap;
- ACE inhibitors – Capoten, Enalapril;
- alpha-blockers – Tonacardin, Doxazosin;
- diuretics – Hypothiazide, Furosemide.
The majority of these drugs are available only by prescription. Regardless of the type of problem that arises, medications should be selected by a specialist. Self-medication can only aggravate your well-being and provoke deterioration. This is why it is so important to obtain specialized medical advice.