Contraindications for carrying out
The procedure is minimally invasive with minimal tissue intervention, but there are limitations for the following conditions:
- acute inflammatory diseases
- exacerbation of chronic diseases
In addition, sclerotherapy for hemorrhoids has the following contraindications:
- inflammation of the hemorrhoid (the process should be stopped before surgery);
- thrombosis of the veins of the hemorrhoidal plexus;
- inflammatory process in the mucous membrane of the rectum or in the surrounding adipose tissue (proctitis, paraproctitis);
- anal fissure
The traditional contraindication to surgery is pregnancy. Treatment of hemorrhoids during pregnancy and the postpartum period is carried out using conservative methods, since the enlargement of nodes is often associated with physiological changes in the body.
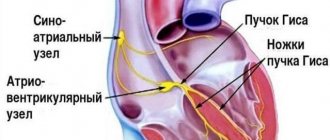
Causes of recurrence of hemorrhoids
The first reason is the presence of a plexus. In the rectum there is an external and internal rectal, or it is called hemorrhoidal, venous plexus. With severe straining during constipation, physical exertion, and childbirth, excessive venous congestion occurs. The wall of the vein bulges under increased pressure, and hemorrhoids form.
When straining, the entire venous network is instantly and simultaneously exposed to increased pressure in all areas of the plexus, including in the operated area and next to it, and at the site of sclerosis, or the application of a rubber ring, or coagulation, depending on what kind of operation was performed. Thus, wall protrusion can occur at any location in the plexus. Thus, the anatomy of the plexus itself contributes to relapse.
The second reason for the recurrence of hemorrhoids is a violation of trophism. As is known, the nervous system regulates the growth, division, and nutrition of organ tissue cells, preserving their structure and function.
The tissues in the anal area, the venous plexus and the rectum are under constant control of the nervous system. These control structures, the subcortical nerve centers, are located in the medulla oblongata of the brain stem. If the control structures malfunction, the trophism of the venous plexus in the rectum is disrupted, its walls become loose and pliable, and therefore bulge easily, which is how relapses occur. Trophic disturbance can also manifest itself as long-term non-healing cracks due to slow tissue regeneration. Anal itching, reduced local immunity. This results in easy infection of the tissues of the perianal area.
Therefore, despite various methods of surgical treatment, none of them guarantees a complete cure. In a significant number of cases, the disease recurs, which forces repeated surgical interventions.
Advantages of the method
Sclerotherapy is affordable, popular and easy to perform. In addition, the advantages of the method include:
- absence of a difficult preparatory period;
- safety;
- no need for anesthesia;
- no pain;
- the procedure is carried out on an outpatient basis, there is no need to go to the hospital;
- short rehabilitation period not associated with strict restrictions;
- can be used to treat elderly people for whom other methods are contraindicated due to the fragility of blood vessels;
- the ability to consistently get rid of all hemorrhoids;
- affordable price.
results
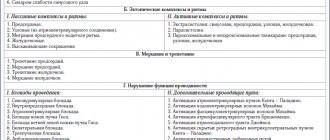
The results of treatment with a follow-up period of 2 years were assessed.
If there was no relapse after treatment, the result was considered good. If it is necessary to repeat the treatment – satisfactory. If it is ineffective, it is bad. The following results were obtained (Table 2):
Table 2 Patient treatment results
| Sclerotherapy with ultrasound | Good | Satisfactory | No effect |
| N=486 patients | 89,5% | 9,1% | 1,4% |
| Traditional sclerotherapy | Good | Satisfactory | No effect |
| N=585 patients | 62,9% | 26,2% | 10,9% |
Features of preparation for the procedure
In order to prepare for the procedure, you do not have to seriously limit yourself in anything or change your usual rhythm of life. However, the following requirements must be met:
- follow a diet that will limit the process of gas formation;
- in the morning before sclerotherapy, cancel breakfast, the procedure should take place on
- empty stomach;
- on the eve of the operation, before going to bed, you need to cleanse the intestines with an enema;
- a day before the procedure, you need to do a skin test for sensitivity to the drug;
How is sclerotherapy performed?
The procedure takes place in a specially equipped room, where there is an anoscope, a proctology chair, devices for administering sclerosant and providing emergency medical care. Administration of the drug takes no more than 10 minutes, and the patient remains under medical supervision for about an hour.
Sclerosis occurs in the following order:
The patient is in a gynecological chair or on the operating table in a supine position, while pulling his legs to his chest or taking a knee-elbow position.
The doctor treats the hands, anus and intestinal lumen with a disinfectant solution.
An anoscope is inserted into the anus and is used to view the hemorrhoids.
Sclerosants are administered through a syringe. First, the internal node is sclerosed. The needle penetrates to a depth of approximately 10 millimeters. The volume of the drug is selected taking into account the size of the node.
Similar actions are performed for each hemorrhoid. In the case of stage 4 hemorrhoids, sclerosants are first injected into the bleeding area.
The needles are gradually removed after the injection is completed. This way you can avoid leakage of the drug and bleeding. The needle is removed after it has been in a calm state for several minutes.
The injection is performed at the point where the blood supply to the hemorrhoid occurs. After administration of the drug, the vessels lose their patency, thrombose, and aseptic inflammation begins. As a result:
- the size of the nodes decreases;
- the tone of the anus decreases;
- the swelling that causes hemorrhoids is eliminated.
After sclerotherapy of hemorrhoidal veins, the patient remains in a lying or sitting position for an hour. If there is no discomfort or any complications after this time, you can leave the clinic.
Introduction
Hemorrhoids are a widespread disease. Among the adult population, it occurs with a frequency of up to 10%; among patients in coloproctology departments it accounts for 40% to 50%.
In standard practice, 50% to 80% of patients undergo surgical treatment. In clinics using minimally invasive methods of treating hemorrhoids, the number of patients requiring surgery is reduced to 30% -40%.
In Russia, the most common type of operation for hemorrhoids is the Miligan-Morgan type operation in the modification of the GNCC. After hemorrhoidectomy, according to the literature, the postoperative period is quite difficult, and the patient’s quality of life is significantly reduced. In 20–30% of cases, severe pain occurs, requiring the use of narcotic and non-narcotic analgesics for 7–12 days.
In 15 - 25%, urinary disorders occur that require drug treatment and the use of catheters, in 2 - 4% - postoperative bleeding, in 3 - 5% - inflammatory complications. The patient's rehabilitation period after surgery is at least 4 weeks. Long-term complications are also observed:
- in 2 - 4% - insufficiency of the anal sphincter;
- in 6 - 9% - stricture of the anal canal.
Hemorrhoidectomy is considered the gold standard for the treatment of hemorrhoids, and despite this, relapses of the disease are observed in 2–3% in the first 3 years and up to 10% in 8–10 years.
Recent studies by domestic and foreign coloproctologists show that hemorrhoidectomy is indicated for stages III and IV of the disease and in no more than 30% of patients.
In our opinion, only patients with stage IV of the disease are subject to surgery, when the nodes not only easily fall out of the anus, but have fibrous changes or do not fit into the anal canal.
Hemorrhoidectomy is also indicated in the presence of large external hemorrhoids.
This change in tactics occurred after the widespread introduction into clinical practice of minimally invasive methods for the treatment of hemorrhoids. This is, first of all, the most common method - latex ligation of hemorrhoids, as well as sclerotherapy, infrared photocoagulation and disarterization of internal hemorrhoids under the control of ultrasound Dopplerography.
However, with all methods of minimally invasive treatment of hemorrhoids, there is a fairly high percentage of disease recurrence in the long term - from 15% to 40%. In addition, each method has certain disadvantages. Thus, with latex ligation, quite often there is a pronounced pain syndrome after the procedure, which lasts up to two or three days. After the hemorrhoid is rejected, a flat wound is formed on the mucous membrane of the anal canal and the external node sinks lower, creating discomfort and a feeling of prolapse.
With sclerotherapy for hemorrhoids, sclerosis of the corpora cavernosa and a decrease in the volume of the node occurs, but in the later stages of the disease, when degeneration of the ligaments of Treitz and Parks is observed, the prolapse and prolapse of the anal canal mucosa continues, like a “removable stocking.” Patients in this situation consider the treatment result to be unsatisfactory.
During disarterization of hemorrhoidal nodes under the control of Doppler ultrasound, the cavernous body of the node remains, albeit empty, which over time can be revascularized, which will lead to relapse.
According to generally accepted theories of the pathogenesis of hemorrhoids, the main causes and factors in the development of the disease are hereditarily determined weakness of the connective tissue, which leads to degeneration of the ligamentous apparatus of the hemorrhoid, rupture of the partitions in the cavernous bodies and increased blood supply. This, in turn, leads to an increase in the size of hemorrhoids and their loss during bowel movements. Congestion during prolapse of nodes contributes to bleeding at the slightest damage to the mucosa.
In 2001, we patented and introduced into clinical practice a method of sclerotherapy of hemorrhoids with ultrasound.
This technique is painless for the patient, does not interfere with work ability, is easy to use, takes 3–4 minutes, and can be used simultaneously on 3 hemorrhoids.
In our opinion, this method is close in effectiveness to sclerotherapy for hemorrhoids with ultrasound, close in effectiveness to surgical treatment, while remaining, perhaps, the most minimally invasive method of treatment. Even when compared with conventional sclerotherapy, we note significantly fewer pain reactions and discomfort in patients who have undergone sclerotherapy with ultrasound.
The method effectively affects several pathogenetic factors:
- firstly, more active sclerosis of the cavernous bodies occurs.
- secondly, at the end of the instrument, the effect of ultrasonic “welding” of tissue occurs, which leads to fixation of the node in the anal canal.
- thirdly, due to the thermal effect inside the node along the instrument, a channel is formed through which, after the procedure, excess sclerosant is poured into the anal canal, which leads to decompression and a decrease in the toxic effects of the sclerosant.
Rehabilitation after sclerotherapy
The patient can leave the clinic on the day of the procedure. But at the same time, the doctor will explain in detail the rules of precaution and the need for attention to his own well-being.
For 2 to 3 days, patients with hypersensitivity may feel discomfort or mild pain at the injection site. Usually such sensations go away on their own.
The pain may intensify at the time of defecation - this is a short-term and expected reaction of the body. As soon as the nodes begin to decrease in size, you feel better.
There is no need for special treatment of the injection site. But in the morning and evening, as well as after each bowel movement, you need to wash yourself with cool water, a decoction of chamomile or calendula.
If you are prone to constipation, you should consult a doctor, he will prescribe medications to soften the stool.
Possible complications
Possible complications with chemical sclerotherapy are:
- A doctor’s mistake when inserting a needle into the muscle layer of the intestine, which is accompanied by pain. However, the doctor can immediately correct its position.
- The same category of errors also includes penetration of a needle into an artery, which is accompanied by bleeding during the procedure. Stopping him is easy enough.
- Bleeding a few days after sclerotherapy may be caused by an excessive amount of the drug used. Treatment of this consequence is carried out conservatively with the help of tablets.
- Erroneous introduction of a substance into the bloodstream through a vein is characterized by pain under the ribs on the right side and an unpleasant taste in the mouth.
- Also, the injection can be carried out into the prostate, resulting in stagnation of urine, prostatitis or purulent inflammation in this area.
- Incorrect penetration of the sclerosing agent into the subcutaneous tissue is accompanied by the development of paraproctitis.
- Pain when injecting into the wrong area of the node.
- Recurrence of hemorrhoids, which can also occur through the fault of the patient himself.
- Thrombosis in this area is the formation of blood clots in the vessels.
Since sclerotherapy is technically easy to implement, from the point of view of modern medicine, and does not require specific equipment, its spread is understandable. Each medical institution independently sets the cost for this procedure based on its professional level and experience of the doctor. When choosing an institution, you should rely on these characteristics, and not chase the lower price level. It is worth considering that the price will certainly increase if it is necessary to repeat sclerotherapy.
Why you should contact the multidisciplinary clinic “Your Doctor”
Modern diagnostic equipment
Highly qualified specialists
High-tech medical care
The procedure is carried out by specialists with many years of experience, we care about our patients and are aimed at high-quality diagnosis and treatment.
Our multifunctional clinic has been operating since 2002. Over all these years of work, we have created all the necessary conditions, each patient receives professional medical services at the highest level: