Jugular vein thrombosis is not a deadly disease and responds well to conservative treatment if you urgently contact a medical facility if any sign indicating its development appears.
It can also serve as a “litmus test” for the fact that not everything is in order in the body and further detailed diagnostics are required to identify the root causes that pushed the circulatory system to form blood clots.
We will talk further about why this pathological condition occurs, how it manifests and is treated.
Features of the disease and ICD classification
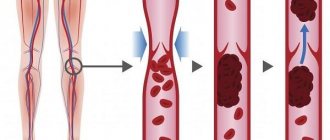
This disease is a pathological condition caused by blockage of the vessel cavity with a blood clot, which causes blood flow disturbances and, as a result, some organs and systems suffer. The lack of adequate therapy can cause the development of a number of rather dangerous complications, so it is extremely important to stop not only its manifestations, but also the cause itself.
It is impossible to unambiguously answer the question about the age category of patients suffering from this disease. Both young people and elderly people are susceptible to it, but in the latter the disease is somewhat more common. Doctors also note that gender may be a risk factor. Thus, among patients who come to medical institutions with a similar problem, the majority are men.
According to the international classification of diseases, created to systematize the statistical information obtained, this pathology has ICD 10 code I82.
Anatomical features
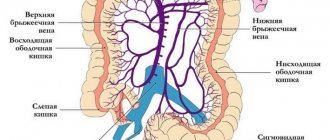
In order to better understand the mechanisms of occurrence and possible localization of pathology, one should turn to anatomy.
In the human body there are 3 main pairs of jugular veins susceptible to thrombosis:
- Internal . The largest among the listed vessels, responsible for the drainage of blood from the skull and normal metabolism in the brain. The venous line begins from the jugular foramen, descends to the area of the sternoclavicular junction, and merges with the subclavian artery. In medical practice, it is most often used for the purpose of catheterization for hemodialysis, plasmapheresis, and long-term infusion therapy.
- Outdoor _ In terms of its size, it ranks second among the vessels of this system and is responsible for draining blood saturated with carbon dioxide from the external parts of the cervical spine and head. It is located close enough to the surface that it can be seen and felt.
- Front . The pair is located under the chin and is part of the venous arch.
Each of these pairs is susceptible to thrombosis, but as statistics show, it is the outer vessel that most often clogs the thrombus.
Symptoms
The manifestation of classic symptoms of such a disease directly depends on the degree of blockage of the vessel by a blood clot. If its size is insignificant and the blood flow is practically not disturbed, the disease is asymptomatic, without causing discomfort to the person. Therefore, the patient most often does not suspect its presence.
If thrombosis of the jugular vein in the neck is provoked by an almost complete blockage of its cavity, then the following typical signs are inevitable:
- Painful sensations in the neck and collarbone area . Sometimes the pain spreads to the shoulder and arm, which significantly interferes with identifying the location of the blood clot. The pain syndrome in this pathology is constant, aching in nature.
- Swelling of the neck in the area where the affected vessel is located , with its obvious bulging, which is noticeable even in the absence of stress on the throat, such as singing or screaming. The swelling can increase in the first hours, the neck at the site of its appearance hurts with any influence (palpation, contact with clothing).
- Change in the skin in the affected area to a red-bluish color.
- There may be limited mobility of the upper limbs due to muscle weakness.
- Headache caused by poor blood flow.
Such symptoms do not become permanent. There are two possible options for the further development of the disease: the onset of a subsiding stage or transition to a chronic form. If the first is characterized by a gradual decrease in negative manifestations, up to their almost complete disappearance, then in the second case, the unpleasant sensations are dulled, but do not completely disappear.
If any of the above clinical manifestations appear, you should immediately seek medical help.
Which method of diagnosing jugular vein thrombosis to choose: ultrasound, MRI, CT, angiography
Selection Methods
- CT, MRI.
Is MSCT of the jugular vein informative for thrombosis?
- In acute and subacute cases, there is usually an increase in the lumen of the jugular vein with a decrease in density in the center of the vessel (thrombus in the lumen of the vein)
- After intravenous administration of a contrast agent, the contrasted blood creates a ring around the thrombus
- With chronic progressive obliteration, complete occlusion of the vein occurs or blood outflow occurs through collateral vessels
- Strengthening of the vein wall indicates the presence of thrombophlebitis
- Possible abscess formation.
Is MRI effective for jugular vein thrombosis?
- Acute, subacute:
- Space-occupying formation with characteristic properties of the blood-thrombus signal
- Increased signal intensity around the thrombus on T2-weighted image.
— Chronic:
- Increased signal intensity in the vein on T1-weighted image
- Decrease in signal intensity on a T1-weighted image (disintegration of blood in a thrombus).
— MR angiography: Lack of signal from moving blood or filling defect in the lumen of the vein.
Sample normal values
- The normal diameter of the internal jugular vein is highly variable
- Right side: 12 mm (6 to 23 mm)
- Left side: 10.5 mm (5 to 19 mm).
Features
- Partially occlusive thrombus in the lumen of the internal jugular vein.
Causes
Thrombosis of the internal, external and external jugular veins, in contrast to the venous system located in the lower extremities, is much less common in medical practice.
It is impossible to unambiguously identify the factor influencing the formation of a blood clot that clogs the lumen of blood vessels.
Most often, the cause of the development of the pathological condition is damage to the vascular walls due to mechanical stress. Due to the intensive production of platelets and fibrin, the body independently “patches” damage, thereby forming blood clots.
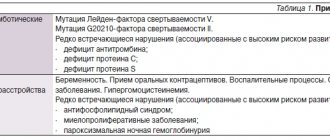
However, there are a number of reasons not related to mechanical damage. Depending on their origin, thrombosis factors are conventionally divided into three groups: hereditary, acquired and complex. Let's look at each of them in more detail.
Hereditary
These factors include:
- congenital mutations;
- anomalies in the structure of the venous system;
- deficiency of C and S – proteins and antithrombin 3 substance;
- congenital changes in coagulation;
- some autoimmune diseases, such as systemic lupus erythematosus.
Purchased
There is a fairly large number of reasons that form the tendency to the appearance of this pathology, acquired during life. These include:
- Carrying out orthopedic operations and the postoperative period.
- Insertion of intravenous catheters.
- Obesity and low physical activity.
- Postpartum period.
- Long-term fixation of the limbs with a plaster cast.
- Taking hormonal contraceptives and increasing estrogen levels.
- Frequent and long flights.
- Smoking.
- Peptic ulcer disease.
- The presence of benign or malignant neoplasms.
- Receiving chemotherapy.
Complex
Doctors include increased levels of fibrinogen, some coagulation factors and homocysteine as complex factors.
Ultrasound diagnosis of venous thrombosis in an outpatient setting
Ultrasound scanner HS60
Professional diagnostic tools.
Assessment of tissue elasticity, advanced 3D/4D/5D scanning capabilities, BI-RADS classifier, options for expert cardiological studies.
Introduction
Acute venous thrombosis is a common and dangerous disease. According to statistics, its frequency in the general population is about 160 per 100,000 population [1]. Thrombosis in the inferior vena cava (IVC) system is the most common and dangerous type of this pathological process and is the main source of pulmonary embolism (84.5%). The superior vena cava system accounts for 0.4-0.7% of pulmonary embolisms (PE), the right side of the heart - 10.4%. Thrombosis of the veins of the lower extremities accounts for up to 95% of cases of all thrombosis in the IVC system. Acute venous thrombosis is diagnosed intravitally in 19.2% of patients [2]. In the long term, deep vein thrombosis (DVT) leads to the formation of postthrombophlebitic disease, manifested by chronic venous insufficiency up to the development of trophic ulcers, which significantly reduces the ability to work and the quality of life of patients.
The main mechanisms of intravascular thrombus formation, known since the time of R. Virchow, are slowing of blood flow (stasis), hypercoagulation, injury to the vessel wall (endothelial damage). Acute venous thrombosis quite often develops against the background of various oncological diseases (malignant tumors of the gastrointestinal tract, female genital area, etc.) due to the fact that cancer intoxication causes the development of hypercoagulable changes and inhibition of fibrinolysis, as well as due to mechanical compression of the veins by the tumor and germination it into the vascular wall. Predisposing factors for DVT are also considered obesity, pregnancy, taking oral hormonal contraceptives, hereditary thrombophilias (deficiency of antithrombin III, protein C and S, Leiden mutation, etc.), systemic connective tissue diseases, chronic purulent infections, allergic reactions [3, 4]. Elderly and senile patients and persons suffering from chronic venous insufficiency of the lower extremities, as well as patients with myocardial infarction, decompensated heart failure, stroke, bedsores, and gangrene of the lower extremities are at the greatest risk of developing DVT. Trauma patients are of particular concern, since femoral fractures are mainly found in elderly and senile people, most burdened by somatic diseases [5]. Thrombosis in trauma patients can occur with any injury to the lower extremities, since all etiological factors of thrombosis (vascular damage, venous stagnation and changes in blood coagulation properties) take place [6].
Reliable diagnosis of phlebothrombosis is one of the current clinical problems. Physical examination methods make it possible to make a correct diagnosis only in typical cases of the disease, and the frequency of diagnostic errors reaches 50% [7]. For example, thrombosis of the veins of the calf muscles with preserved patency of the remaining veins is often asymptomatic. Because of the risk of missing acute DVT of the legs, clinicians often make this diagnosis in every case of pain in the calf muscles [8]. Particular attention should be paid to “trauma” patients, in whom the presence of pain, swelling and discoloration of the limb may be a consequence of the injury itself, and not of DVT. Sometimes the first and only manifestation of such thrombosis is massive pulmonary embolism.
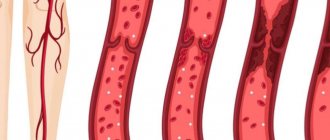
The tasks of instrumental examination include not only confirming or refuting the presence of a thrombus, but also determining its extent and degree of embologenicity. Isolating embolic-dangerous thrombi into a separate group and studying their morphological structure are of great practical importance, since without this it is impossible to develop effective prevention of pulmonary embolism and select optimal treatment tactics. Thromboembolic complications are more often observed in the presence of a floating thrombus with a heterogeneous structure and an uneven hypo- or isoechoic contour, in contrast to thrombi that have a hyperechoic contour and a homogeneous structure. An important criterion for the embologenicity of a thrombus is the degree of its mobility in the lumen of the vessel. Embolic complications are more often observed with severe and moderate mobility of thrombomass [9, 10].
Venous thrombosis is a fairly dynamic process. Over time, the processes of retraction, humoral and cellular lysis help reduce the size of the thrombus. At the same time, processes of its organization and recanalization are underway. In most cases, vascular patency is gradually restored, the valve apparatus of the veins is destroyed, and the remains of blood clots in the form of wall overlays deform the vascular wall. Difficulties in diagnosis may arise when repeated acute thrombosis occurs against the background of partially recanalized veins in patients with postthrombophlebitic disease. In this case, a fairly reliable criterion is the difference in vein diameter: in patients with signs of recanalization of thrombus masses, the vein diameter decreases due to the subsidence of the acute process; with the development of rethrombosis, there is again a significant increase in the diameter of the vein with unclear (“blurred”) contours of the walls and surrounding tissues [9]. The same criteria are used in the differential diagnosis of acute parietal thrombosis with postthrombotic changes in the veins.
Of all the non-invasive methods used to diagnose thrombosis, ultrasound scanning of the venous system has recently been increasingly used. The triplex angioscanning method, proposed by Barber in 1974, includes the study of vessels in B-mode, analysis of the Doppler frequency shift in the form of classical spectral analysis and color flow mapping (in speed and energy modes). The use of spectral Doppler ultrasound made it possible to accurately measure blood flow within the lumen of the veins. The use of color Doppler mapping (CDC) made it possible to quickly distinguish occlusive from non-occlusive thrombosis, identify the initial stages of recanalization of thrombi, and also determine the location and size of venous collaterals. In dynamic studies, the ultrasound method allows for fairly accurate monitoring of the effectiveness of thrombolytic therapy. In addition, with the help of ultrasound, it is possible to determine the causes of clinical symptoms similar to those in venous pathology, for example, to identify a Baker's cyst, intermuscular hematoma or tumor. The introduction into practice of expert-class ultrasonic devices with sensors with frequencies from 2.5 to 14 MHz made it possible to achieve almost 99% diagnostic accuracy.
Material and methods
The examination included examination of patients with clinical signs of venous thrombosis and pulmonary embolism. Patients complained of swelling and pain in the lower (upper) limb, pain in the calf muscle (usually of a bursting nature), “pulling” pain in the popliteal region, pain and compaction along the saphenous veins. On examination, moderate cyanosis of the leg and foot, dense swelling, pain on palpation of the leg muscles were revealed; in most patients, positive Homans and Moses symptoms.
All subjects underwent triplex scanning of the venous system using modern ultrasound machines with a linear sensor with a frequency of 7 MHz. At the same time, the condition of the veins of the thigh, popliteal vein, veins of the leg, as well as the great and small saphenous veins was assessed. A 3.5 MHz convex probe was used to visualize the iliac veins and IVC. When scanning the IVC, iliac vein, great saphenous vein, femoral veins and veins of the leg in the distal lower extremities, the patient was in the supine position. The study of the popliteal veins, veins of the upper third of the leg and the small saphenous vein was carried out with the patient lying on his stomach with a cushion placed under the ankle joints. Difficulties in diagnosis arose when visualizing the distal part of the superficial femoral vein in obese patients, visualizing the veins of the leg with pronounced trophic and indural changes in tissue. In these cases, a convex sensor was also used. Scanning depth, echo signal amplification and other study parameters were selected individually for each patient and remained unchanged during the entire examination, including observations over time.
The scan was started in cross-section to exclude the presence of a floating tip of the thrombus, as evidenced by complete contact of the venous walls during light compression with the sensor. After making sure that there was no freely floating tip of the thrombus, a compression test with a sensor was carried out from segment to segment, from proximal to distal sections. The proposed method is the most accurate not only for detecting thrombosis, but also for determining its extent (excluding the iliac veins and IVC, where the patency of the veins was determined in the CD mode). Longitudinal scanning of the veins confirmed the presence and characteristics of venous thrombosis. In addition, longitudinal sectioning was used to locate the anatomical venous confluence. During the examination, the condition of the walls, the lumen of the veins, the localization of the thrombus, its extent, and the degree of fixation to the vascular wall were assessed.
Ultrasonic characterization of venous thrombi was carried out in relation to the lumen of the vessel: they were distinguished as parietal, occlusive and floating thrombi. Signs of parietal thrombosis were considered to be visualization of a thrombus with the presence of free blood flow in the lumen of the vein, the absence of complete collapse of the walls when the vein is compressed by a sensor, the presence of a filling defect during color circulation, and the presence of spontaneous blood flow during spectral Dopplerography (Fig. 1).
Rice. 1.
Non-occlusive thrombosis of the popliteal vein. Longitudinal scanning of the vein. Envelope blood flow in energy flow coding mode.
Ultrasound criteria for floating thrombi were: visualization of the thrombus as an echogenic structure located in the lumen of the vein with the presence of free space, oscillatory movements of the apex of the thrombus, absence of contact of the vein walls during compression with the sensor, presence of free space when performing respiratory tests, circumflex type of blood flow during color circulation, the presence of spontaneous blood flow with spectral Doppler ultrasound. When a floating thrombus was detected, the degree of its mobility was assessed: pronounced - in the presence of spontaneous movements of the thrombus during quiet breathing and/or breath-holding; moderate - when oscillatory movements of a blood clot are detected during functional tests (cough test); insignificant - with minimal thrombus mobility in response to functional tests.
Research results
From 2003 to 2006, 236 patients aged from 20 to 78 years were examined, 214 of them with acute thrombosis and 22 with pulmonary embolism.
In the first group, in 82 (38.3%) cases, the patency of the deep and superficial veins was not impaired and clinical symptoms were due to other reasons (Table 1).
Table 1
. Conditions with symptoms similar to DVT.
| Pathology | Number of patients | |
| abs. | % | |
| Injury | 33 | 40,2 |
| Joint diseases | 18 | 22,0 |
| Lymphovenous insufficiency | 12 | 14,6 |
| Large Baker's cyst | 6 | 7,3 |
| Lymphadenitis | 5 | 6,1 |
| Intramuscular hematoma | 4 | 4,9 |
| Extravasal compression | 4 | 4,9 |
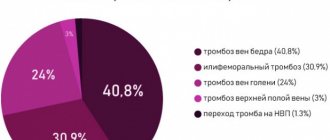
The diagnosis of thrombosis was confirmed in 132 (61.7%) patients, while in most cases (94%) thrombosis was detected in the IVC system. DVT was detected in 47% of cases, superficial veins - in 39%, damage to both the deep and superficial venous systems was observed in 14%, including 5 patients with involvement of perforating veins.
The probable causes (risk factors) of the development of venous thrombosis are presented in table. 2.
table 2
. Risk factors for thrombosis.
| Risk factor | Number of patients | |
| abs. | % | |
| Trauma (including long-term plaster immobilization) | 41 | 31,0 |
| Varicose veins | 26 | 19,7 |
| Malignant neoplasms | 23 | 17,4 |
| Operations | 16 | 12,1 |
| Taking hormonal medications | 9 | 6,8 |
| Thrombophilia | 6 | 4,5 |
| Chronic limb ischemia | 6 | 4,5 |
| Iatrogenic causes | 5 | 4,0 |
In our observations, the most common form of thrombosis was detected, as well as damage to the veins at the level of the popliteal-tibial and femoral-popliteal segments (Table 3).
Table 3
. Localization of DVT.
| Localization | Number of patients | |
| abs. | % | |
| Veins of the leg | 19 | 14,4 |
| Popliteal vein | 8 | 6,0 |
| Popliteus tibial segment | 34 | 25,8 |
| Femoropopliteal segment | 21 | 15,9 |
| Ileofemoral segment | 5 | 3,8 |
| Femoro-popliteal-tibial segment | 38 | 38,8 |
| Iliofemoral-popliteal-tibial segment | 7 | 5,3 |
More often (63%) there were thromboses that completely occluded the lumen of the vessel; in second place in frequency (30.2%) were mural thrombi. Floating thrombi were diagnosed in 6.8% of cases: in 1 patient - in the saphenofemoral anastomosis with ascending thrombosis of the trunk of the great saphenous vein, in 1 - ileofemoral thrombosis with a floating apex in the common iliac vein, in 5 - in the common femoral vein with thrombosis of the femoral-popliteal vein segment and in 2 - in the popliteal vein with DVT of the leg.
The length of the non-fixed (floating) part of the thrombus, according to ultrasound data, varied from 2 to 8 cm. Moderate mobility of thrombotic masses was more often detected (5 patients), in 3 cases the mobility of the thrombus was minimal. In 1 patient, during quiet breathing, spontaneous movements of the thrombus in the lumen of the vessel were visualized (high degree of mobility). In our observations, floating thrombi with a heterogeneous echostructure were more often detected (7 people), with the hyperechoic component predominant in the distal section, and the hypoechoic component in the area of the thrombus head (Fig. 2).
Rice. 2.
Floating thrombus in the common femoral vein. B-mode, longitudinal scanning of the vein. Thrombus of a heteroechoic structure with a clear hyperechoic contour.
In the first case, an isoechoic thrombus with a hyperechoic contour was recorded (Fig. 3), in the second - a homogeneous “organized” thrombus with a clear contour (Fig. 4).
Rice. 3.
Floating thrombus in the superficial femoral vein. B-mode, longitudinal scanning of the vein. Thrombus of an isoechoic structure with a hyperechoic contour.
Rice. 4.
Floating thrombus in the superficial femoral vein. B-mode, longitudinal scanning of the vein. Thrombus of homogeneous echostructure with a clear contour.
In the group of patients with clinical pulmonary embolism, 5 (22.7%) patients had DVT of various stages of development (mainly the femoropopliteal segment).
Over time, 82 patients were examined to assess the course of the thrombotic process, of which 63 (76.8%) had partial recanalization of thrombotic masses. In this group, 28 (44.4%) patients had a central type of recanalization (with longitudinal and transverse scanning in the color flow mode, the recanalization channel was visualized in the center of the vessel); in 23 (35%) patients, parietal recanalization of thrombotic masses was diagnosed (most often, blood flow was determined along the wall of the vein directly adjacent to the artery of the same name); In 13 (20.6%) patients, incomplete recanalization was detected with fragmentary asymmetric staining in the Color Doppler mode. Thrombotic occlusion of the vein lumen was observed in 5 (6.1%) patients; in 6 (7.3%) cases, restoration of the vein lumen was noted. Signs of rethrombosis persisted in 8 (9.8%) patients.
conclusions
A comprehensive ultrasound examination, including angioscanning using spectral, color and power Doppler modes and echography of soft tissues, is a highly informative and safe method that allows the most reliable and quick solution to issues of differential diagnosis and treatment tactics in outpatient phlebological practice. It is advisable to conduct this study on an outpatient basis for earlier identification of patients for whom thrombolytic therapy is not indicated (and sometimes contraindicated), and to refer them to specialized departments; when confirming the presence of venous thrombosis, it is necessary to identify individuals at high risk of developing thromboembolic complications; monitor the dynamics of the thrombotic process and thereby adjust treatment tactics.
Literature
- Lindblad, Sternby NH, Bergqvist D. Incidence of venous thromboembolism verified by necropsy over 30 years. //Br.Med.J. 1991. V. 302. P. 709-711.
- Savelyev V.S. Pulmonary embolism - classification, prognosis and surgical tactics. // Thoracic and cardiovascular surgery 1985. N°5. pp. 10-12.
- Barkagan Z.S. Hemorrhagic diseases and syndromes. Ed. 2nd, revised and additional M.:Medicine 1988; 525 pp.
- Bergqvist D. Postoperative thromboembolism. // New York 1983. P. 234.
- Savelyev V.S. Phlebology. M.: Medicine 2001; 664 pp.
- Kokhan E.P., Zavarina I.K. Selected lectures on angiology. M.: Nauka 2000. P. 210, 218.
- Hull R., Hirsh J., Sackett DL et al. Combined use of leg scenning and impedance plethysmography in suspected venous thrombosis. An alternative to venography. // N.Engl.J.Med. 1977. N° 296. P. 1497-1500.
- Savelyev V.S., Dumpe E.P., Yablokov E.G. Diseases of the main veins. M., 1972. S. 144-150.
- Albitsky A.V., Bogachev V.Yu., Leontyev S.G. and others. Ultrasound duplex angioscanning in the diagnosis of rethrombosis of the deep veins of the lower extremities. // Kremlin Medicine 2006. N°1. pp. 60-67.
- Kharchenko V.P., Zubarev A.R., Kotlyarov P.M. Ultrasound phlebology. M.: ZOA "Eniki". 176 p.
Ultrasound scanner HS60
Professional diagnostic tools.
Assessment of tissue elasticity, advanced 3D/4D/5D scanning capabilities, BI-RADS classifier, options for expert cardiological studies.
Diagnostics
If characteristic complaints appear, the first priority is to consult a doctor. This may be a therapist or phlebologist who will collect an anamnesis of the disease based on the patient’s complaints and visual examination.
However, for an accurate diagnosis, it is necessary to conduct instrumental and laboratory studies to establish the location, extent of the lesion and determine the quality of blood parameters. The following diagnostic methods are widely used:
- Ultrasound examination with Dopplerometry of the vascular network of the neck and head. The most informative diagnostic method, which allows not only to determine the exact location of the blood clot, but also to determine the disturbance of blood flow. When symptoms of jugular vein thrombosis appear, this study is prescribed first.
- Magnetic resonance imaging. MRI is used to study the condition of internal organs and tissues. Has the highest accuracy of any commonly used imaging modality such as radiography or computed tomography.
- Thrombodynamics . With its help, clotting disorders are identified and, based on the results obtained, the most effective therapy and dosage of thinning drugs are selected.
- Thrombin generation test . Thrombin acts as a catalyst in the process of transforming fibrinogen into fibrin. It is also often used in the practice of cardiologists and phlebologists.
- Thromboelastography . An instrumental method for assessing the viscosity of a blood clot, the result of which is displayed on paper.
- Prothrombin time test . Shows the clotting time of plasma under the influence of specially added thromboplastin.
Also, the attending physician may prescribe additional diagnostic methods, at his discretion, based on the specific situation. Read about how to diagnose and treat internal varicose veins in the legs in our material.
This is interesting! Contraindications to magnetic resonance venography include installed dental implants, braces and braces.
Clinical manifestations
A typical picture of symptoms of jugular vein thrombosis:
— Random find:
- Swelling of the neck
- Located in the lateral sections of the neck, below the hyoid bone or in the supraclavicular region.
— Paraneoplastic syndrome (Trousseau syndrome).
— Compression or infiltration associated with the tumor process.
— Acute thrombophlebitis:
- Increased body temperature
- Soft, painless swelling (differential diagnosis with abscess)
- Gentle head position
- Rarely - fulminant sepsis.
— Chronic jugular vein thrombosis: Dense, sometimes painless swelling (differential diagnosis with a tumor).
Drug treatment
The basis of therapy for the formation of blood clots in the circulatory system is the use of direct and indirect anticoagulant drugs. They are aimed at thinning the blood by reducing the level of fibrinogen, a substance whose concentration increases to form clots.
Direct anticoagulants include:
- Fibrinolysin,
- Fraxiparine,
- Heparin.
After a decrease in the prothrombin index, they switch to medications with an indirect anticoagulant effect, such as Curantil or Aspirin.
Another important aspect in complex therapy is the prescription of phlebotonics, whose action is aimed at improving metabolic processes and eliminating inflammation.
Remember! The dosage of any medications and the method of their use are prescribed exclusively by a competent medical professional.
If necessary, antispasmodics are prescribed to reduce the tone of the vascular walls and relieve pain. The addition of sepsis indicates the need for antibacterial therapy.
You can find out what varifort for varicose veins is and the opinion of Elena Malysheva from our article.
What diseases have symptoms similar to jugular vein thrombosis
Abscess
— Rarely tubular in shape
— Marked enhancement after administration of contrast agent
— May be adjacent to a vein or occur elsewhere
Tumor (with necrosis)
— Almost never has a tubular shape
— There is usually a lower signal intensity on T1-weighted image than that of the thrombus
— May be adjacent to a vein or occur elsewhere
Enlarged lymph nodes (inflammation or tumor)
— Usually multiple lesions or conglomerate
— Enhancement after contrast administration
— Located along the vein, the image of which is often normal.
Surgical intervention
If conservative therapy does not bring the desired result, minimally invasive surgical procedures can be used to eliminate the blood clot. The frequency of surgical treatment for this disease is significantly inferior to classical therapy.
The most common methods are:
- Aspiration thrombectomy is the mechanical removal of thrombolytic mass through a puncture made through the skin.
- Endovascular thrombolysis is the delivery of a thrombolytic drug directly to the site of a vascular lesion by subcutaneous insertion of a special catheter. Thus, its patency is partially or completely restored.
Read about the manifestations and methods of treating varicocele on both sides in our material.
Complications
Despite the fact that thrombosis of the internal jugular vein does not lead to pulmonary embolism (PE) as often as thrombosis of the vessels of the lower extremities, it is extremely undesirable to delay its treatment.
Neglect of one’s own health, manifested in failure to receive timely consultation with a doctor or self-medication, can lead to the development of the following pathological conditions that pose a real danger to human life and health and require immediate medical intervention:
- Swelling of the optic nerve , leading to decreased visual acuity or its complete loss.
- Sepsis is an infection of the body by pathogenic microorganisms, the appearance of which is provoked by local infectious inflammation. In the absence of adequate treatment, serious irreversible consequences are possible.
- TELA . A deadly pathology that develops extremely rarely, but it should not be ruled out. If timely assistance is not provided, the mortality rate is 90%.
Principles of treatment of jugular vein thrombosis
- Broad-spectrum antibacterial agents (active against aerobes and anaerobes) for the treatment and prevention of infectious processes
- Anticoagulant therapy (heparin 30,000 units/day for 10 days)
- Resection or ligation of the vein is indicated in rare cases, since cases of pulmonary embolism from the head and neck vessels are very rare
- In most cases, spontaneous recovery occurs due to recanalization of the thrombus or outflow of blood through collateral vessels.
Forecast
Timely seeking help from a medical institution and correctly selected treatment methods eliminate the development of complications. In this case, a favorable outcome of the disease can be predicted. An exception should be considered pathology caused by metastases during the development of malignant neoplasms.
When sepsis is added, it is impossible to clearly assess what the prognosis will be. However, it should be noted that if inflammatory processes occur, provoked by the lack of timely treatment of jugular vein thrombosis, it will be doubtful. When diagnosing a reversible process of organ damage, the recovery period can be 3-6 months.
What is important to know about jugular vein thrombosis
- Inflammatory etiology is becoming less common
- Usually iatrogenic causes (insertion of a catheter, pacemaker, radiation therapy)
- Jugular vein thrombosis accounts for 5% of all thromboses
- Men and women get sick equally often
- The disease occurs in all age groups
- Acute, subacute or chronic occlusion of the internal jugular vein by a thrombus
- Three groups of reasons (Virchow’s triad):
— Endothelial defect (for example, due to prolonged catheterization or injection drug addiction).
- Slowing or stopping blood flow (for example, due to compression or invasion by a tumor).
- Blood clotting disorders (for example, caused by a tumor process).
Prevention
To prevent the development of pathology, you first need to be attentive to your own health and undergo regular medical examinations. If a person is at risk, it is necessary to systematically conduct a study such as coagulometry - a blood test for clotting. Thus, it is possible to promptly detect hypercoagulation leading to the formation of blood clots in the vascular system.
Particular attention should be paid to the choice of clothing. It should not hinder movement or squeeze the body. For everyday wear, preference should be given to loose items made from natural fabrics and of appropriate size. We described how to avoid varicose veins on the legs in our article.
Compliance with the drinking regime will prevent dehydration of the body and, as a result, thickening of the blood. Therefore, the minimum amount of clean water consumption should be 2 liters per day.
Giving up bad habits, adjusting your diet and diet, and daily moderate physical activity have a beneficial effect on the general condition of the body. Excluding fried and fatty foods from the menu reduces the chances of developing thrombosis, both of the superior jugular vein and similar pathologies everywhere.
We talked about whether an exercise bike will help with varicose veins here.