So-called rheumatism or acute rheumatic fever (according to new terminology) is a systemic inflammatory disease of connective tissue, in which the pathological process has a tropism towards the membranes of the heart and joints.
Even at the beginning of the 20th century, the concept of “rheumatism” meant almost any disease of the joints - doctors did not have the need or opportunity to differentiate these ailments, especially since the range of healing procedures was not diverse. Today, a rheumatologist has a wide range of diagnostic methods in his arsenal, allowing him to distinguish rheumatism from many other rheumatological diseases, each of which has its own treatment strategy.
Rheumatism is a disease predominantly of children aged 6 to 15 years, and only 1 child in 1000 suffers in this age group.
Primary rheumatism in adult patients is observed less frequently. According to statistics, women are 2-3 times more likely to suffer from this disease than men.
Rheumatism usually begins some time after a streptococcal infection of the nasopharynx, and after a few years it can turn into a chronic, incurable disease. Fortunately, only 1-3% of patients who have an infection become victims of rheumatic fever.
1
Consultation with a rheumatologist
2 Consultation with a rheumatologist
3 Consultation with a rheumatologist
General information about rheumatism
Acute rheumatic fever
ー systemic inflammatory disease characterized by damage to joint tissues, heart and blood vessels. Develops in predisposed individuals after suffering a streptococcal infection (pharyngitis, tonsillitis, scarlet fever, erysipelas). Most often it develops in adolescents and young people due to the high reactivity of their immune system.
With this disease, foci of inflammation appear with tissue destruction in large and medium-sized joints, heart tissue, kidneys, and liver. The greatest danger is rheumatic heart disease. This is the most common cause of the formation of acquired heart defects and carries a risk of developing heart failure, thromboembolism (blockage with blood clots) of the pulmonary and cerebral arteries.
Medical diagnostic methods
To diagnose rheumatism, the patient is usually prescribed:
- ECG to detect disturbances in the contractile rhythm of the heart;
- an x-ray of the heart, which reveals changes in the configuration of heart tissue and signs of a decrease in its contractile function;
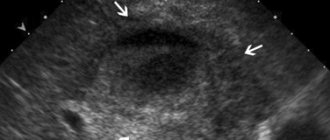
- Heart ultrasound or echocardiography to identify defects;
- laboratory tests, the results of which show the presence of streptococcal infection, inflammatory process and immune pathology.
According to the generally accepted diagnostic rule, the presence of the disease is confirmed by identifying two major criteria or two minor and one major criterion for rheumatism.
Causes of rheumatism
Group A hemolytic streptococcus causes the development of sore throat, scarlet fever, and erysipelas. The human immune system actively reacts to the presence of such a pathogen in the body - it produces specific antibodies that fight the microbe. But the enzymes that streptococcus produces have a toxic effect on the heart muscle. In addition, they have a similar structure to the proteins of the human body, so antibodies begin to attack not only microbes, but also their own tissues, rheumatic carditis, rheumatoid arthritis, and glomerulonephritis develop.
Therefore, rheumatic fever is considered a disease of an infectious-allergic nature - a pathogenic microorganism plays a role in its development, with hyperreactivity of the human immune system.
Many of us have had a sore throat, but only 1-3% of people develop rheumatic fever, due to the following factors:
- incorrect treatment of streptococcal infection;
- genetic predisposition;
- hypothermia;
- deficiency of vitamins and microelements;
- the presence of autoimmune diseases (lupus, scleroderma, etc.).
Clinical picture of rheumatism
The trigger for the development of rheumatism is the entry of streptococcus into the body, as a result of which the immune system begins to produce antibodies to fight the infection. However, in the body itself, namely in connective tissues and heart muscle, there are molecules of the same structure. Due to the presence of this factor, the immune system begins to “fight” its cells. As a result, connective tissue is damaged, and this is fraught with heart defects and joint deformation.
Forms of rheumatism
- cardiac form (cardiac rheumatism), when all the membranes of the heart are affected (pancarditis), myocardium (myocarditis), endocardium (endocarditis);
- articular form (rheumatism of the joints);
- cutaneous form;
- pulmonary form (pleurisy);
- rheumatic chorea (St. Vitus' dance).
Classification of rheumatism
Based on the nature of the flow, the following forms are distinguished:
- acute (up to 3 months);
- subacute (3-6 months);
- prolonged (more than 6 months);
- latent (hidden) - occurs without characteristic symptoms, without laboratory changes, is detected after the formation of heart defects;
- recurrent - wave-like course with rapid development of internal organ failure.
There are active and inactive phases of the disease. In the active, a specific laboratory picture is observed (increased levels of C-reactive protein (CRP) - reflecting acute inflammatory processes, antistreptolysin).
Clinical forms of rheumatism:
- rheumatic carditis - inflammation of the heart tissue;
- polyarthritis ー multiple joint damage;
- ring-shaped erythema - a specific rash on the skin;
- chorea - severe neurological symptoms (hand tremors, muscle weakness, involuntary movements);
- subcutaneous nodules - with the formation of dense nodules under the skin in the joint area.
Forecast
The prognosis remains conditionally unfavorable (mortality rate up to 30%). Causes of death can be: progressive heart failure, rhythm disturbances, renal failure, thromboembolic complications. Timely administration of antibiotic therapy in adequate dosages and over a long course makes an almost absolute cure possible. Relapses of endocarditis, as a rule, occur a month after the end of antibiotic therapy and cause the development of valvular lesions (40% of cases) and the progression of heart failure, increasing the patient’s level of disability.
Symptoms and signs of rheumatism
The disease can be suspected by the following manifestations:
- development of the disease 1-2 weeks after tonsillitis, pharyngitis, scarlet fever, erysipelas;
- a sharp increase in body temperature, general weakness;
- joint pain (knee, ankle, elbow, wrist);
- swelling and redness of the skin over the joints, stiffness of movement;
- pain in the heart area;
- shortness of breath, dizziness, headache;
- muscle weakness, involuntary twitching of the limbs;
- pink rash in the form of a ring on the body, passes quickly;
- rheumatic nodules - painless, dense small formations under the skin in the joint area;
- nagging pain in the lower back, darkening, redness of urine.
If such symptoms appear, you should make an appointment with a physician, cardiologist or rheumatologist.
Modern methods of treating rheumatism
A patient with an acute form is hospitalized in a hospital. Treatment includes:
- Bed rest for 2-3 weeks.
- A nutritious diet with limited salt.
- Antibacterial therapy - to combat streptococcal infection.
- Nonsteroidal anti-inflammatory drugs, such as diclofenac, to reduce inflammation.
- In severe cases, glucocorticosteroids (drugs of adrenal hormones that suppress the immune system and have a powerful anti-inflammatory effect).
- After discharge, you need to be observed and continue treatment with a rheumatologist at the clinic. Long-term use of anti-inflammatory drugs and antibiotics helps prevent relapse. The doctor may refer you for rehabilitation to a specialized sanatorium.
Rheumatism is a disease that is usually not life-threatening. Its most serious complication is heart disease, which may require surgical treatment.
If you are worried about pain in your heart or joints, and your therapist finds it difficult to establish the correct diagnosis, make an appointment with a rheumatologist at the Medical Center International Clinic Medica24. You can undergo an examination with us and continue treatment on an outpatient basis if you have been discharged from the hospital with a diagnosis of rheumatism. Make an appointment by phone: +7 (495) 230-00-01
The material was prepared by oncologist, traumatologist-orthopedist of the international clinic Medica24 Andemir Olegovich Akhov.
Features of the course of rheumatism in children
Rheumatic fever is more severe in children than in adults. The leading clinical form is carditis; heart defects form more often and faster in children.
Articular syndrome in children is less pronounced, and other extracardiac manifestations (annular rash, subcutaneous nodules, chorea) are more common with more pronounced manifestations.
But, despite its more severe course, the disease in children responds better to drug treatment, and relapses can be avoided. If symptoms of rheumatism appear, hurry up and show your child to the pediatrician. Do not deny your child medical care, follow all recommendations, all the appointments of the pediatrician, this can be vital.
Treatment
Treatment of patients with rheumatism is carried out in a hospital setting. The patient is prescribed strict bed rest until clinical signs of activity are eliminated, diet No. 10 with a recommendation to increase protein content and reduce salt intake.
Drug treatment protocol:
- Etiotropic therapy - penicillin antibiotics 1.5-4 million OD per day for 10-12 days, then Bicillin-5 1.5 million. every 3 weeks. An alternative is macrolides (erythromycin);
- Pathogenetic treatment.
- Glucocorticosteroids - prednisolone 0.7-1 mg/kg with high activity of the process;
- Non-steroidal anti-inflammatory drugs - Indomethacin, Ortofen, COX-2 inhibitors, salicylates;
- Aminoquinolines - Delagil or Plaquenil for a prolonged recurrent course and primary valvular damage;
- Symptomatic therapy - correction of heart failure, detoxification, antiplatelet agents, cardiac glycosides, tranquilizers, metabolic agents.
Diagnosis of rheumatism
The diagnosis is made by clinical and laboratory signs. Main criteria: polyarthritis, carditis, chorea, annular rash, subcutaneous nodules.
Laboratory tests are required to confirm the diagnosis:
- general blood analysis;
- C-reactive protein level;
- level of antibodies to streptococcus and its toxins (antistreptolysin, antistreptokinase).
To assess the level of heart damage, you need to do:
- chest x-ray;
- ECG;
- echocardiography (ultrasound of the heart with Doppler sonography).
Rheumatic fever is often “missed” due to a blurred clinical picture and diagnostic errors. To prevent this from happening, get tested in trusted laboratories.
The Paracelsus Medical Center uses certified expert-class diagnostic equipment, which undergoes standardization and calibration.
All doctors work according to the principles of evidence-based medicine (international protocols drawn up on the basis of clinical trials). This minimizes the likelihood of a false diagnosis.
Tactics for managing patients with rheumatism at the outpatient stage
Rheumatic diseases are one of the most common pathologies of the human body, and, despite the successes in the treatment of rheumatism (R) and heart defects, their importance not only in the medical, but also in the social aspect throughout the world cannot be overestimated. According to WHO, more than 1/3 of cases of temporary disability and 10% of total disability are caused by rheumatic diseases.
Almost every 8–10th person over 15 years of age suffers from some kind of rheumatological disease. Moreover, in young people, disability with rheumatism exceeds this indicator with coronary heart disease and hypertension. According to a national study conducted in the United States in the early 1990s, rheumatic diseases rank second among the diseases of the adult population. Every year in Russia, heart valve defects are registered in more than 230 thousand adult patients and 8.3 thousand adolescent and childhood patients. The incidence of diseases of the musculoskeletal system and connective tissue has a steady upward trend. Despite the fact that the disease begins more often in childhood and young adulthood, heart lesions resulting from R are also diagnosed in adulthood. This is due to the fact that rheumatism with a latent course or asymptomatic manifestations of the disease currently dominates.
Rheumatology, which is an integral medical branch, unites a number of areas of medicine: general therapy, cardiology, nephrology, orthopedics and traumatology, rehabilitation. Careful supervision and continuity between various departments in the management of patients with rheumatic processes are the main principles of the organization of medical care for patients with rheumatic diseases. It is quite difficult to recognize the disease at an early stage. This, on the one hand, is associated with a change in the nature of the course towards the predominance of subclinical, so-called minor forms of the disease, and on the other hand, with the loss of doctors’ alertness towards rheumatism.
Currently, there is a scientific debate around the very term “rheumatism” and the need to revise the classification and nomenclature of the nosological form in question. The term “rheumatic fever” seems to be the most justified, since it draws the doctor’s attention to the need to clarify the connection with infection caused by group A β-hemolytic streptococcus (GABHS), and the subsequent prescription of antibiotics to eradicate this infection in the acute period (primary prevention), as well as to prevent recurrences attacks (secondary prevention). Any practicing physician and researcher should take into account the postulate of J. Rotta, according to which “rheumatism will not disappear as long as group A streptococcus circulates, and the human population, for a number of objective reasons, cannot be rid of streptococcus.”
Clinical picture and course of the disease
Rheumatism as a systemic disease is characterized by a polysyndromic clinical picture. At the same time, along with general changes in the condition of patients, there are signs of involvement in the pathological process of the joints, heart, nervous system and (less often) other organs and systems.
In typical cases, the disease develops 1–3 weeks after GABHS or (less commonly) another infection. With repeated attacks, this period may be reduced. In some patients, even primary rheumatism occurs 1–2 days after cooling without any connection with infection.
In case of P, in addition to heart damage, other organs and systems are often involved in the pathological process. Its characteristic manifestations include articular syndrome, which is accompanied by pain in the joints (arthralgia) and swelling of the periarticular tissues. Intensive use of antibiotics, corticosteroids, changes in the virulence of microbial flora, as well as prevention of R in recent years have led to the fact that indolent R (prolonged, with minimal activity) with predominant damage to the heart has become the dominant clinical form. The decrease in acute forms of P contributed to a more favorable course of the disease: the number of patients with pancarditis, pericarditis, and nephritis decreased. The nature of recurrent rheumatic carditis has also changed: today it does not always result in the formation of heart disease.
During P, two phases are distinguished - active and inactive, which is extremely important for the treatment and prevention of disease progression. Clinical manifestations of P depend on the activity of the inflammatory process. Timely detection of minimal process activity and anti-inflammatory therapy can significantly reduce the number of complications and improve the prognosis of the disease. The influence of minimal P activity on the progression of heart disease, worsening heart failure, and an increase in the number of complications of rheumatic heart disease—arrhythmias, thromboembolism, and acute coronary insufficiency—has been proven.
Relapses of the disease often develop after any intercurrent diseases, surgical interventions, or physical overload.
Diagnosis is based on the syndromic principle formed by the domestic pediatrician A. A. Kisel in 1940, who identified the “Big” diagnostic criteria: migratory polyarthritis, carditis, chorea, annular erythema, rheumatic nodules, drawing attention to the diagnostic significance of their combination . In 1944, the American cardiologist T.D. Jones classified the indicated pentad of syndromes as “large” diagnostic criteria, highlighting along with them “small” clinical and laboratory parameters. The diagnosis of P becomes more likely when “major” criteria (absolute Kisel-Jones criteria) are combined with “minor” ones, which include fever, arthralgia, a history of P or the presence of mature valvular heart disease, changes in laboratory parameters: increased ESR, leukocytosis, positive reaction to C-reactive protein, dysproteinemia, increased levels of immunoglobulins, etc. Data from ECG, FCG, EchoCG and X-ray examination are also taken into account. Great importance is attached to data confirming streptococcal infection: elevated titers of streptococcal antibodies, culture of group A streptococcus from the throat and a recent nasopharyngeal infection.
Laboratory monitoring allows you to choose patient management tactics and make timely adjustments to therapy. To monitor the course of the disease and identify the active phase of the process, tests such as determining the concentration in the blood serum of C-reactive protein, rheumatoid factor and antibody titer to streptococcus (ASO titer) are effective. The importance of immunological parameters for the diagnosis of chronic inflammatory process has now been proven. To detect minimal activity of rheumatism, the most sensitive indicators are the neutrophil level. Changes in the values of NBT test indicators indicate the activity of rheumatism.
Establishing a reliable diagnosis of rheumatism, especially at the initial stage, is often a difficult task. Competent differential diagnosis is of great importance in the correct diagnosis and choice of management tactics.
Treatment of rheumatism
The basis of treatment for P is a phasing system, the essence of which is continuous monitoring and treatment of the patient at all stages of the process (hospital - in the acute phase; local sanatorium, clinics - in the subacute phase; resort - in the inactive phase of the disease).
In case of an acute process, treatment begins in a hospital, continues in a cardio-rheumatological sanatorium and then on an outpatient basis.
The therapeutic program for the treatment of patients with rheumatism consists of antimicrobial and anti-inflammatory treatment, measures aimed at restoring immunological homeostasis, organizing a rational balanced diet and adaptation to physical activity, as well as preparation for work load, timely surgical treatment of patients with heart defects.
Pathogenetic therapy of P still remains an important problem in modern medicine. Along with immune disorders, rheumatism develops such complex pathological processes as inflammation, sclerosis, depolymerization of the main components of connective tissue and others, on which the outcome of the disease itself depends. Therefore, it is important that antirheumatic drugs affect the above processes.
In acute polysyndromic course of P or with the development of pancarditis, glucocorticosteroids are indicated - prednisolone or methylprednisolone (metipred, solu-medrol - 0.6-0.8 mg/kg/day) for 10-14 days, less often longer, under clinical and instrumental supervision data, including dynamic echocardiography monitoring. The simultaneous use of corticosteroids and non-steroidal anti-inflammatory drugs (NSAIDs) (M. A. Yasinovsky) can increase the therapeutic effect, and by reducing the dose of hormonal drugs, reduce the risk of adverse reactions.
Currently, the most pathogenetically substantiated in the treatment of R is the therapy of NSAIDs, which, in addition to anti-inflammatory, analgesic and antipyretic effects, have a certain effect on the body’s immune response.
When treating R in adults, the drug of choice is diclofenac (dicloran, voltaren, diclobene) (orally 100 mg/day, in tablets of 50 and retard capsules of 100 mg, rectally - 100 mg/day, in suppositories of 50 and 100 mg), having high anti-inflammatory activity comparable to that of prednisolone.
The negative effects of NSAIDs on the mucous membrane are associated with the development of minor symptoms from the digestive tract and more serious complications - damage to the mucous membrane of the stomach and duodenum. A new generation of drugs - specific NSAIDs (Ambene, Airtal, Ketonal, Movalis, Nimesil, Nemulide) allows you to avoid the above-mentioned severe complications if you need to take constant, long-term use of NSAIDs. A prominent representative of this class of drugs is Celebrex (200–400 mg), which has a pronounced anti-inflammatory and analgesic effect and does not have a harmful effect primarily on the gastrointestinal tract. Due to the leading role of streptococcal infection in the development of P, the use of antibacterial drugs is of great importance. β-lactam antibiotics remain the drug of choice: penicillins (amoxicillin - 1.5 g in 3 doses; phenoxymethylpenicillin - 1.5 g in 3 doses; benzathine penicillin - 2.4 million units intramuscularly), cephalosporins (cefadroxil - 1 g in 2 doses ); for intolerance to β-lactam antibiotics - macrolides (spiramycin - 6 million units in 2 doses; azithromycin - 0.5 g on the 1st day, then 0.25 g in 1 dose; roxithromycin - 0.3 g in 2 doses; clarithromycin - 0.5 g in 2 doses; midecamycin - 1.2 g in 3 doses); for intolerance to macrolides and β-lactam antibiotics - lincosamines (lincomycin - 1.5 g in 3 doses; clindamycin - 0.6 g in 4 doses). The immunosuppressive effect of penicillin antibiotics reduces the risk of developing R.
Quinoline drugs (Delagil, Plaquenil) have a therapeutic effect in continuously relapsing forms of P and have a weak immunosuppressive effect. For the treatment of P, they are usually used in combination with salicylates. The dose of delagil is 0.25 g, plaquenil is 0.3–0.4 g/day. The course of treatment for a continuously relapsing course ranges from 3 to 6 months, and sometimes 9–12 months.
Cytostatic immunosuppressants - 6-mercaptopurine, imuran (azathioprine), chlorobutine, endoxan - are indicated only for patients with continuously relapsing or protracted course of R, who are resistant to treatment with both classical antirheumatic drugs, including corticosteroids, and quinoline drugs with their long-term, many-month course application. The dose of 6-mercaptopurine, imuran (azothioprine) is 0.1–1.5 mg/1 kg of weight, chlorobutine is 5–10 mg/day.
The connection between rheumatism and heart damage is reflected in the aphorism belonging to the French physician Lasegue: “Rheumatism licks the joints and bites the heart.” Aortic heart defects can be asymptomatic for a long time (sometimes for 20–25 years), and then very quickly decompensation occurs with the development of severe heart failure and cardiac arrhythmias, most often atrial fibrillation. Mitral heart defects have typical clinical symptoms and gradually decompensate, leading to heart failure.
The progression of heart failure is due to the activation of neurohumoral systems, in particular the sympathoadrenal and renin-angiotensin systems. ACE inhibitors and AT1 blockers are currently the drugs of choice for the treatment of any stage of heart failure. The inclusion of ACE inhibitors (captopril, enalapril, quinapril, lisinopril, moexipril, ramipril, cilazapril) in the complex therapy of patients with heart failure due to rheumatic heart defects helps to significantly reduce its size, increase the ejection fraction, and improve performance. The drugs are well tolerated by patients: captopril is prescribed starting with a dose of 6.25 mg 3 times a day, gradually titrating it to 75 mg/day if well tolerated; enalapril - from 1.25 to 10 mg/day. The use of AT1 blockers (Diovan 40 mg once daily) requires caution in the presence of stenoses. Treatment of patients with heart failure should include diuretics (veroshpiron, thiazide, indapamide retard), nitrates (nitroglycerin, isoket, nitromint, olycard retard), β-blockers (atenolol, bisoprolol, metoprolol, sotalol).
At the stage of formed heart disease, rheumatism becomes a surgical problem, and it is very important to make an adequate decision on its surgical correction in a timely manner. Diagnosis and treatment of active P at the preoperative stage are of great importance for obtaining positive long-term results. For reliable diagnosis of chronic inflammatory process, it is important to use immunological markers. All efforts of doctors involved in preparing patients for surgical correction of heart disease (since only surgical intervention can radically help such patients) should be aimed at eliminating the inflammatory process and reducing signs of heart failure.
Despite the successes achieved in the treatment of patients with rheumatic heart disease, in a number of patients the therapeutic effect of traditional therapy remains unsatisfactory, and this forces us to look for new ways to further improve treatment measures. In the treatment of rheumatological patients, along with standard treatment methods, the latest methods and achievements of domestic rheumatology are used. According to indications, the following are carried out: hyperbaric oxygenation, pulse therapy with steroid hormones (metipred, solu-medrol) and cytostatics (6-mercaptopurine, imuran (azothioprine), chlorbutin, endoxan), efferent methods of treatment (hemosorption, plasmapheresis).
The basis of primary prevention of R is timely diagnosis and adequate treatment of GABHS tonsillitis or pharyngitis, for the treatment of which β-lactam antibiotics (penicillins, cephalosparins, carbapenems) are the drug of choice.
Secondary prevention of R is aimed at preventing repeated attacks and progression of the disease and involves regular administration of long-acting penicillin (benzathine penicillin), the use of which in the form of bicillin-5 has significantly (4–12 times) reduced the frequency of repeated rheumatic attacks and, therefore, increased life expectancy patients with rheumatic heart disease. It should be noted that the effectiveness of benzathine benzylpenicillin prophylaxis is currently the subject of debate. Studies conducted at the Institute of Rheumatology of the Russian Academy of Medical Sciences and the State Research Center for Antibiotics have shown that benzathine-benzylpenicillin, prescribed at a dose of 2.4 million units intramuscularly every 3 weeks, is currently a highly effective and safe drug for secondary prevention. When prescribing a preventive course of bicillin, it is necessary to take into account the presence of immunological markers of inflammation and the degree of reactivity of the body, differentially prescribing the drug to each patient.
Clinical observation and preventive treatment play an important role in the management of patients with rheumatic diseases. The objectives of clinical examination include: implementation of therapeutic measures aimed at the final elimination of the active rheumatic process; carrying out symptomatic treatment of circulatory disorders in patients with heart defects; prescribing general health measures, hardening procedures, dosed physical exercises; implementation of secondary prevention of relapse of the disease. At the clinical examination stage, issues related to the ability to work and employment of patients are also resolved, and problems of surgical correction of defects are discussed together with cardiac surgeons. Successful radical correction of the defect, performed in a timely manner, before the development of irreversible pathological changes in the heart and other organs, helps restore the personal and social status of the operated people and provides a certain economic effect.
Spa treatment
Balneotherapy in a resort promotes the restructuring of hemodynamics - an increase in cardiac output with a slight decrease in heart rate, achieving a higher level of functioning of the cardiovascular system, and consequently, preventing the development of circulatory failure, which is the main prerequisite for the widespread use of baths for rheumatic heart lesions. In addition, balneotherapy affects the immunological reactivity of the body, enhancing nonspecific protection and reducing the severity of autoimmune disorders.
During the period when P activity decreases to a minimum, treatment is indicated in local cardiological sanatoriums, where, along with drug treatment and the listed physical factors, climatotherapy using a gentle method and moderate physical activity are used.
Currently, resort treatment of patients with even minimal P activity is considered acceptable against the background of ongoing drug antirheumatic treatment in specialized sanatoriums.
The choice of resort is determined by the specific (influence of chemicals and gases dissolved in water) effect of mineral waters. For the treatment of P, balneotherapeutic resorts with carbon dioxide, sulfide, radon, sodium chloride, iodine-bromine and nitrogen-siliceous waters are indicated. Balneotherapy is contraindicated for heart failure above stage 2A, aortic heart disease with heart failure above stage 1, and severe heart rhythm disturbances.
For the purpose of differentiated treatment of patients with rheumatism, it is necessary to take into account the peculiarities of the action of mineral waters.
Carbon dioxide waters (Borjomi, Matsesta) have a pronounced positive effect on the contractile function of the myocardium, normalize the rhythm of cardiac activity and peripheral hemodynamics. Carbon dioxide baths are effective in patients with stenosis of the left atrioventricular orifice. They can be used for atrial fibrillation (moderately tachysystolic form).
For combined mitral-aortic heart defects, it is preferable to prescribe radon baths, which cause a mild hemodynamic restructuring. Like carbon dioxide, radon baths have a positive effect on abnormal heart rhythm, as well as sedative and analgesic effects, improve tissue trophism and metabolism.
Sodium chloride baths help improve blood circulation, microcirculation and tissue trophism, eliminate blood hypercoagulation and normalize immunological processes.
During the remission phase, mud therapy can also be used in the form of applications to the area of the affected joints.
After mitral commissurotomy, it is recommended to send patients to cardiological sanatoriums at their place of residence (in the inactive phase or in the presence of activity no higher than stage 1, NC no higher than stage 2A). 6–8 months after surgery, in the absence of contraindications, patients can be sent to climatic and balneological resorts. After heart valve replacement, sanatorium treatment is carried out only in cardiological sanatoriums at the place of residence, where patients are prescribed climate therapy using a gentle method and moderate physical training.
Non-drug therapeutic factors make it possible to reduce the level of medication load, provide more rational, comprehensive treatment, and help increase the average life expectancy and improve the quality of life of this group of patients.
Note!
- More than 1/3 of cases of temporary disability and 10% of general disability are caused by rheumatic diseases.
- The disease develops 1–3 weeks after GABHS or (less commonly) another infection.
- In recent years, sluggish rheumatism with predominant damage to the heart has become the dominant clinical form.
- “Major” diagnostic criteria: migratory polyarthritis, carditis, chorea, annular erythema, rheumatic nodules.
- “Minor” diagnostic criteria: fever, arthralgia, history of rheumatism or the presence of formed valvular heart disease, changes in laboratory parameters - increased ESR, leukocytosis, positive reaction to C-reactive protein, dysproteinemia, increased levels of immunoglobulins, etc.
- The basis for the treatment of rheumatism is a phasing system, the essence of which is continuous monitoring and treatment of the patient at all stages of the process (hospital - in the acute phase; local sanatorium, clinic - in the subacute phase; resort - in the inactive phase of the disease).
Clinical example
Patient V.M., born in 1950, is a painter by profession. I went to the clinic about ARVI. She complained of a runny nose, dry cough, weakness, malaise, and palpitations on exertion. There is no typical rheumatic history. Physical examination revealed a systolic murmur at the apex of the heart. Special research methods: electrocardiography with functional load, cardiac fluoroscopy, phonocardiography, analysis of the phase structure of systole, blood flow velocity, minute volume of blood, capillary permeability, oscillography - indicated the presence of stenosis of the left atrioventricular orifice. According to laboratory tests, no active process was identified. In the hospital, the patient received antirheumatic treatment with subsequent observation in a clinic. After 6 months, an increase in the symptoms of cardiovascular failure was noted. Repeated examination revealed progression of stenosis of the left atrioventricular orifice. After a course of preoperative therapy, the patient was referred for surgical treatment and underwent commissurotomy. From the hospital, after a course of primary rehabilitation, the patient was transferred to a cardiological sanatorium to continue rehabilitation treatment.
A. K. Protasova , Doctor of Medical Sciences N. V. Manshina E. V. Maklakova Medical, Moscow
Prevention of rheumatism
Basic preventive measures:
- timely treatment of streptococcal infections;
- completing the full course of antibiotic therapy, if one was prescribed (you cannot stop taking antibiotics earlier than prescribed by the doctor);
- avoiding hypothermia and contact with people with tonsillitis;
- general measures to strengthen the immune system (balanced diet, physical activity, walks in the fresh air).
How to treat?
Since the disease is systemic in nature, treatment of rheumatism is carried out under the strict supervision of medical specialists. As a rule, complex therapy is used, the main goals of which are to suppress infection, stop the inflammatory process and prevent or treat cardiovascular pathologies. The therapy consists of three stages.
- Hospital treatment. It includes drug therapy - taking non-steroidal anti-inflammatory drugs, antibiotic therapy, and other prescriptions depending on the symptoms. If necessary, to eliminate the source of chronic infection, tonsils can be removed, but not earlier than 2-3 months after the onset of the disease. In addition, the patient is prescribed nutritional therapy and exercise therapy. Special diets for rheumatism involve split meals (at least 5-6 meals a day), a high protein content and a minimum of carbohydrates, fresh and processed vegetables. Protein foods are mainly fish, eggs and dairy products.
- Cardio-rheumatic sanatorium. The therapy started in the hospital continues, dosed physical activity, walks, hardening and restorative physical procedures, and dietary nutrition are added to it.
- Dispensary observation. At this stage, the goal of treatment efforts is preventive measures to prevent relapses and stop the process.
Timely detection and adequate therapy, as a rule, lead to complete recovery of patients.