Frequency of testing for detected mutations
A lot depends on the age of the patient. It is the attending physician who determines the time for laboratory and hardware tests. The important points are:
— original background;
— availability of therapy (its results).
Is the diagnosis of thrombophilia accompanied by observation by a hematologist or hemostasiologist?
Diagnosing this disease requires the gynecologist to have certain knowledge and skills related to it. However, in the absence of constant monitoring by a hematologist or hemostasiologist during pregnancy, such consultations are usually not required.
When is screening for genetic thrombophilia required?
This must be done if the following indications are present:
- hereditary predisposition (complex family history - close relatives under 50 years of age suffered from heart attacks, thrombosis, strokes, pulmonary embolism, or died suddenly from unknown causes);
- history of thrombosis;
— undergoing an in vitro fertilization procedure with negative results;
- unfavorable obstetric history in the form of previous diseases (placental abruption, placental insufficiency, fetal growth restriction syndrome, preeclampsia, antenatal death, etc.);
- temporary or permanent increase in the level of homocysteine or antiphospholipid antibodies.
Prevention of thrombosis
Prevention of thrombosis in thrombophilia in most cases is based on lifestyle changes. Patients are advised to avoid strenuous exercise and injury while maintaining the same amount of physical activity. An important preventive measure is wearing compression stockings. Doctors always decide on preventive measures strictly individually after assessing the thrombotic risk.
Bibliography
- Kyrle PA, Rosendaal FR, Eichinger S. Risk assessment for recurrent venous thrombosis //Elsevier.2010;376(9757):2032–2039.
- Khan S., Dickerman JD Hereditary thrombophilia. // Thromb. J. BioMed Central. 2006;4:15.
- Vasiliev S.A., Vinogradov V.L., et al. Thrombosis and thrombophilia: classification, diagnosis, treatment, prevention // RMZH - 2013.- No. 17. - P.896.
- Robertson L. et al. Thrombophilia in pregnancy: a systematic review // Br. J. Haematol. Blackwell Science Ltd.2006;132(2):171–196.
- Sibai BM, How HY, Stella CL Thrombophilia in pregnancy: Whom to screen, when to treat. 2007;19(1):50–64.
- Battinelli EM, Marshall A., Connors JM The role of thrombophilia in pregnancy. // Thrombosis. Hindawi.2013; 2013:516420.
- Andriyashkin A.V. Russian clinical recommendations for the diagnosis, treatment and prevention of venous thromboembolic complications // Phlebology - 2015. -T. 9. – No. 2. – P.1–52.
SARU.ENO.19.03.0436
Does genetic thrombophilia affect the characteristics of childbirth?
This pathology is not a reason to choose, for example, a cesarean section. The method of delivery is chosen as in other cases.
Taking tests
The number and time of tests is determined by the gynecologist. The result of donating blood from a vein is usually ready the next day (urgent analysis is available).
The state of the blood coagulation system is assessed by:
- hemostasiogram;
- platelet aggregation;
- D-dimer.
Which medical specialist prescribes the course of treatment?
If the gynecologist is sufficiently qualified, no additional consultations are required for treatment.
Does the gynecologist understand hemostasis?
The medical center employs gynecologists, whose level of qualifications and experience in medical practice undoubtedly meet the necessary requirements.
Causes of pathology
As a result of various pathological processes in the body, blood clots can form that block blood flow. Most often, this phenomenon is caused by a mutation in the clotting factor gene (or, as it is also called, Leiden). A mutation in the prothrombin gene can also lead to the development of pathology.
If a patient has even one of these mutations, the risk of thrombophilia increases several times. Various provoking factors can also worsen the situation:
- excess weight;
- taking oral contraceptives;
- smoking;
- sedentary lifestyle;
- oncological pathologies;
- IVF protocols;
- pregnancy period.
Folic acid preparations
Today, no one doubts that folic acid should be used two months before the planned pregnancy by the patient when she is planning a pregnancy, in order to reduce the risk, namely, chromosomal abnormalities, neural tube defects, and microcephaly. Low doses, 400 mcg, are usually recommended for this purpose. The maximum is 800 mcg.
If we are talking about patients with high homocysteine levels, that is, this is a moderate and severe form of hyperhomocysteine, of course, such doses are not enough to reduce homocysteine levels. Such patients should receive doses of at least 5 milligrams per day, along with vitamins B, B6, B12. We start with injection therapy, then move on to tablet forms of B vitamins and antiplatelet agents.
Treatment of thrombophilia when planning pregnancy
Medicines, diet and strict regimen are the three main directions in the treatment of the disease.
Medicines for thrombophilia are anticoagulants, drugs to reduce blood clotting, they are prescribed individually and exclusively by specialists.
Additionally, for the treatment of thrombophilia when planning pregnancy, it is recommended to take Omega-3. Taking Omega-3 reduces blood viscosity, reduces the production of thromboxane, which constricts blood vessels, and improves the fluidity of red blood cell membranes. All this has an antithrombotic effect when taken on a regular basis. Therefore, doctors recommend a continuous course of Omega-3 to prevent thrombosis, especially for women with high blood clotting rates.
The Pregnoton Mama complex, recommended for pregnant women and preparation for pregnancy, contains Omega-3 in an effective dosage. You can take the drug throughout the entire period of pregnancy.
Our services in phlebology
The administration of CELT JSC regularly updates the price list posted on the clinic’s website. However, in order to avoid possible misunderstandings, we ask you to clarify the cost of services by phone: +7
| Service name | Price in rubles |
| Appointment with a surgical doctor (primary, for complex programs) | 3 000 |
| Appointment with a cardiovascular surgeon (phlebologist), MD. Malakhova Yu.S. with ultrasound examination (primary) | 4 500 |
| Duplex scanning of the veins of both lower extremities | 6 000 |
| Duplex scanning of the veins of one lower limb | 3 500 |
All services
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions
Criteria for APS syndrome
Laboratory criteria for antiphospholipid syndrome are the circulation of lupus anticoagulant, quantitative determination of cardiolipin antibodies to beta-2-glycoprotein. And it is extremely important to study twice with an interval of 12 weeks.
Today, 12 weeks of pregnancy is an extremely long period of time to wait for confirmation of the diagnosis of “antiphospholipid syndrome,” especially if the patient has already had miscarriages, and only then decide whether or not to prescribe anticoagulants.
Therefore, in our practice, in such patients, if the presence of a high titer of antibodies to beta-2-glycoprotein or antibodies to other phospholipid cofactors (prothrombin, circulation of lupus anticoagulant, pronounced phenomenon of this anticoagulant) is confirmed, even once, we regard this as antiphospholipid syndrome and immediately begin anticoagulant therapy. Genetic thrombophilia can be very different, depending on its form, we can predict those forms that are characteristic of this thrombophilia and the risk of thrombotic complications.
If we are talking about a deficiency of protein C, protein S, then, as a rule, there are often early losses. However, the genetic form of thrombophilia is more characterized by late losses, when the pregnancy is terminated after 20 weeks of pregnancy.
Micronized progesterone preparations
During pregnancy, micronized progesterone preparations are used due to the fact that this group of drugs does not have any pathogenic effect on intrauterine development.
Let me step aside a little from the problem of thrombophilia. A huge number of researchers are specifically studying the problem of intrauterine programming of a child. There is no doubt that intrauterine development is nothing more than a certain program, which has its own laws and which is laid down very early.
But during intrauterine development, this programming can be disrupted, and this can be a consequence of the occurrence of various fetal deformities and behavioral disorders.
This is the same diabetes, metabolic syndrome and so on. The use of drugs during pregnancy, especially in the early stages of pregnancy, requires a very careful approach. To date, mechanized progesterone preparations have been recognized as absolutely safe: Utrozhestan, Crinon and an oil solution of progesterone.
Gynecological cleansing
Several weeks may pass from the moment the fetus dies until it is rejected by the uterus. The remaining traces of the deceased embryo provoke the development of the inflammatory process, bleeding and other complications. To eliminate risks, doctors recommend undergoing gynecological cleansing.
The procedure is performed under general anesthesia and usually takes about 15-20 minutes. In rare cases, complications may occur. The obtained tissue samples are sent to the laboratory for histological analysis. Genetic testing helps determine the cause of miscarriage. Histology determines the presence or absence of atypical cells in the uterus.
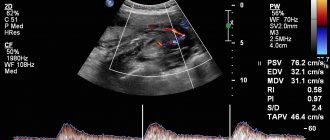
Diagnostics
Tests after a frozen pregnancy should be taken with the mandatory inclusion of ultrasound in the list of studies - the most accurate diagnostic technology in this case. In addition to stating the fact of fetal death, the method will determine the period of developmental cessation.
Therapeutic treatment begins after diagnosis. If the pathology is confirmed, there are several response options:
- Expecting a miscarriage is a natural process for the body to rid itself of a foreign body. Ideally, the amniotic sac will be released completely with the embryo and amniotic fluid contained in it.
- Prescription of specialized drugs, the action of which is aimed at contracting the uterus and pushing out the dead fetus from the internal cavity. The method is applicable if the pregnancy did not last longer than 8 weeks.
- Surgery - intervention is carried out using different methods. These include gynecological cleansing and vacuum aspiration.
After the procedures, a control ultrasound is performed to assess whether the internal space of the uterus is completely cleared and whether there are any foreign tissues left in it that can cause inflammation and cause sepsis to develop.
Antiplatelet agents
The antiplatelet agents we use in pregnant women are low doses of aspirin. The small doses that are currently used throughout the world in pregnant women include doses of no more than 100 milligrams. Although in practice we, as a rule, do not increase the dose of aspirin above 75-80 milligrams. But in some cases, the issue of aspirin resistance arises, which occurs in almost 30-40% of the population.
It is possible to check the presence of aspirin resistance only by studying platelet aggregation activity. This is also an extremely painful issue of modern diagnostics and the modern so-called “hemostasiogram” in quotes. Because today, each laboratory understands coagulogram and hemostasiogram as its own set of parameters of the coagulation and anticoagulation system.
The process of studying platelet aggregation activity is labor-intensive.
It is extremely necessary for pregnant women, especially in patients with antiphospholipid syndrome, thrombocytopenia, and thrombocytopathy. Because both high platelet function and low platelet function are two ends of a big problem. On the one hand, there is a risk of thrombosis, and on the other, there is a risk of bleeding. The correct selection of antiplatelet agents is extremely important.
Vacuum aspiration
In addition to curettage, a vacuum aspiration method can be performed, which allows you to get rid of the remains of the embryo in a more delicate way. Indications for the procedure are:
- period no more than 12 weeks;
- confirmation of a frozen pregnancy using additional examination methods;
- incomplete exit of parts of the embryo from the uterus, the presence of foreign elements in the organ;
- threat to the mother's life or risk of developing fetal pathology;
- lag of placental tissue at the time of childbirth, when its remains are found in the uterine cavity;
- accumulation of blood clots or fluid in the uterus;
- the need for a biopsy.
The procedure is not relevant::
- with inflammatory processes developing in the uterus;
- to neutralize the risks of ectopic pregnancy;
- if there are changes in the uterus due to neoplasms or tumor.
The method is also not recommended if the period after the previous abortion does not exceed six months.
Aspiration is carried out in several ways:
- Under intravenous anesthesia with vacuum . The technology is not practiced beyond 4 weeks of pregnancy.
- Under local anesthesia with manual vacuum . Used up to 12 weeks of pregnancy.
Before aspiration, it is necessary to undergo a visual examination by a specialist, take recommended tests, and a smear to determine the microflora. Examination methods include ultrasound, blood and urine tests, tests for hidden infections in the body. Consultation with a therapist is mandatory.
The consequences of aspiration can be complicated by:
- menstrual irregularities;
- disruptions in the hormonal system;
- incomplete cleansing of the uterine cavity.
For a month after the procedure, you should refrain from sexual intercourse, visiting the bathhouse, and staying in the sun. It is not recommended to take a bath or go to the pool. Medicines should be taken in accordance with the schedule drawn up by a specialist.
Antispasmodics are prescribed to neutralize pain. You should not be active or engage in physical labor for 24 hours after surgery, as exertion may cause bleeding. Painful sensations in the lower abdomen and lumbar region may persist for several days.
Immediate consultation with a doctor is required if:
- a sharp increase in body temperature;
- continuous heavy discharge;
- pain, which even taking potent medications cannot relieve;
- unusual strong odor from the genitals.
Frozen pregnancy, the causes and consequences of which negatively affect the emotional background of the mother who has lost her child, also occurs in completely healthy couples. In the West, the practice of a thorough examination is recommended only after the third repetition of fetal growth arrest in the womb. As for the tests after an anomaly has occurred, the list is quite extensive: OBC, OAM, blood for hormone levels, smear for microflora, research for hidden sexually transmitted infections, tests for TORCH infections, transvaginal ultrasound. If necessary, the list can be supplemented with other diagnostic procedures. It is recommended to obtain advice from a geneticist, endocrinologist and immunologist.